Abstract
Purpose
This study was done to examine the threshold value of estimated height loss at which the risk of osteoporosis increases and to verify its discriminative ability in the detection of osteoporosis.
Methods
It was conducted based on epidemiological descriptive methods on 732 Korean women at a public healthcare center in Seoul between July and November 2010. ANOVA, Pearson correlation, logistic regression analysis and receiver operating characteristics (ROC) curve were used for data analysis.
Results
There was an age-related correlation between bone mineral density (lumbar spine: F=37.88, p<.001; femur: F=54.27, p<.001) and estimated height loss (F=27.68, p<.001). Estimated height loss increased significantly with decreasing bone mineral density (lumbar spine: r=-.23, p<.001; femur: r=-.34, p<.001). The odds ratio for the point at which the estimated height loss affects the occurrence of osteoporosis was found to increase at a cut-off value of 2 cm and the area under ROC curve was .71 and .82 in lumbar spine and femur, respectively.
Osteoporosis is a condition whereby patients are at increased vulnerability to the bone fragility and susceptibility to fracture due to a low bone mass and the micro architectural deterioration of the bony tissue. It is characterized by a derangement of bone metabolism that restricts the active life of more than half of osteoporotic women and of most men and women over the age of 70 years. In Korea, the number of patients with osteoporosis has increased steeply by 13% on average annually during a recent 4-year period (i.e., 2005-2009). People aged 50 years or older account for 91.4% of all osteoporosis patients. Moreover, the prevalence of osteoporosis has been reported to be 13.1 times in female patients than in male patients (Korea Institute for Health and Social Affairs, 2010a). These data have lead to the widespread recognition that osteoporosis develops exclusively in the middle-aged and older people, and in women in particular.
The clinical issues associated with osteoporosis could be pathological fractures and the risk of death due to fat embolism caused by fractures. Kyphosis due to vertebral fracture and loss of height can cause respiratory and cardiac function impairment. Patients must tolerate lower back pain during their normal daily lives that results from bearing their own weight when erect. Elderly people with osteoporosis are particularly vulnerable to hip fracture and becoming subsequently bedridden. As such, osteoporosis ultimately leads to other serious complications and sequelae, which together with the clinical consequences of it (Fancis, Aspray, Hide, Suteliffe, & Wilkinson, 2008; Park, 2005; Schlaich et al., 1998).
Due to the seriousness of osteoporosis, clinical and public health nurses from Korea have long operated a program for the prevention of osteoporosis. In particular, each public health center is equipped with a densitometer and recommends the measurement of bone mineral density in their community residents.
An osteoporotic state is characterized by decreased bone mineral density and a subsequent increase in fracture risk. Accordingly, bone mineral density is recognized as a good prognostic indicator for the occurrence of osteoporotic fracture. However, the radiological definition of osteoporosis remains a tool for establishing the criteria for pharmacological treatments or for the management of the condition, which are applied to diet therapy, exercise therapy, and educational programs. These are intensively provided by nurses for patients of a specific age group in whom the condition has already progressed to the osteoporotic state of lower bone mass. It can therefore be stated that the efficiency of preventive nursing care in maintaining and improving the quality of life related to osteoporosis is truly insufficient, and particularly so for middle-aged and older women. Moreover, 51.3% of patients with osteoporotic fractures over the age of 50 didn't have their bone density measured to identify whether or not they had osteoporosis. In these circumstances (KIHASA, 2010b), it is not cogent to recommend the examination of bone mineral density to people of all the age groups from the perspective of the cost-to-benefit ratio. Even without the relatively expensive bone density examination, more routine and generalized indicators between the different groups would lead to more active coping with and would thus be beneficial to patients with osteoporosis.
Height is one of basic biological characteristics known to change with aging and usually decreases because of osteoporotic deformity and fracture as well as degeneration (Sorkin, Muller, & Andres, 1999). Thus, one of the potential factors used to determine the overall risks of developing an osteoporotic state is the height loss that occurs with physical aging; this is also a marker of the outcome of bone deformities, which are hallmarks of osteoporosis (Adachi et al., 2001; Yoshimura et al., 2008). In particular, the osteoporotic deformity of the spine may deform the thoracic vertebrae, impair respiratory functions and, ultimately, lower the quality of life (Schlaich et al., 1998). Accordingly, this factor can be selected as being beneficial factors in preventive strategies for osteoporosis.
There is no doubt that height is an anthropometric factor that plays a pivotal role in predicting the occurrence of osteoporosis. Previous studies involving subjects in the United Kingdom, Australia, and Iran, and also multinational studies have found that osteoporosis is related to changes in height, the risks of developing osteoporosis, including vulnerability to fracture, increase when the height decreases by 2-5 cm (Center et al., 1998; Krege, Siminoski, Adachi, Misurski, & Chen et al., 2006; Moayyeri, Ahmadi-Abhari, Hossein-nezhad, Larijani, & Soltani, 2006; Siminoski et al., 2005; Tobias et al., 2007). For Japanese women this value was found to be over 4 cm (Masunari, Fujiwara, Nakata, Nakashima, & Nakamura, 2007), while the North American Menopause Society (2006) reported it to be 3.8 cm. Thus, although loss of height has been reported to be one of the risk factors associated with the occurrence of osteoporosis, the specific criteria regarding the determination of osteoporosis are variable.
One of the greatest risk factors for osteoporosis is aging of the skeletal system. Of all patients with osteoporotic vertebral fractures, only one-third are in need of the medical care because of the acute onset of lower-back pain (Francis et al., 2008). It is also regrettable that for the aforementioned patients, the management of symptoms is no longer based on the recognition that osteoporosis is also an unavoidable aging phenomenon, although they are told that the pain originates from the osteoporosis. However, it is hopeful that the seriousness and status of bone loss can also be recognized simply based on changes in height.
Moreover, no studies have investigated osteoporosis-induced changes in height in Koreans in both the medical and nursing fields. Furthermore, based on the consideration that people with greater height are at increased risk of developing osteoporotic fractures (Joakimsen, Fønnebø, Magnus, Tollan, & Johanne Søgaard, 1998; Meyer, Falch, O'Neill, Tverdal, & Varlow, 1995), it would be useful to detect osteoporosis to examine the magnitude of height loss that is associated with risk of developing osteoporosis and to test its discriminative ability in Koreans, who are shorter than many other races.
Most of us are the tallest at around 30-35 years old because of the peak bone mass at that time. Accordingly, the maximum height may be the value which we had a long time ago. Thus, most research analyzing the difference between the maximum height value and the current height may estimate height loss by depending on the memory of subjects (Ismail et al., 1999; Tobias et al., 2007).
Given this background, we conducted the present study to examine the threshold risk value of estimated height loss at which the risk of osteoporosis increases and to verify its discriminative ability in the detection of osteoporosis in women who experience a marked pattern of the spontaneous bone loss. Thus, this study suggested the usefulness of estimated height loss for the detection of osteoporosis. Early detection of osteoporosis by height measurement will provide the subjects more progressive motives related to the behaviors to reduce bone loss rate including change from ordinary exercises to weight bearing exercises stimulating the bones or restriction of high sugar or high protein diet accelerating the elimination of Ca. Furthermore, height measurement result can be utilized as the objective data for nursing strategy to prevent bone density from entering into fracture zone.
This study was based on the epidemiological descriptive methods to examine the threshold cut-off value of estimated height loss at which the risk of osteoporosis increases and to verify its discriminative ability in the detection of osteoporosis in women.
This study cohort comprised a total of 732 women after excluding of 85 subjects (74 men, 11 subjects with insufficient information) from the 817 individuals who voluntarily registered for a regular check-up of bone mineral density at a public healthcare center located in Seoul between July and November 2010. DXA, the latest, high-precision equipment, was purchased and residents were given information about the purchase; it was recommended for use in 2009.
The subject of this study was limited to women because osteoporosis occurrence of women is 2.7 times as high as men in a lifetime due to more diverse change of bone metabolism than men (KIHASA, 2010b) and so women are generally included in high risk group of osteoporosis.
Bone mineral density is an indicator for the mineral substances within the bone and hence the density (Park, 2004). We measured the bone mineral density with the aid of dual energy X-ray absorptiometry (DXA: Prodigy Advance, GE Lunar, USA, 2008), the method for measuring the mineral density of the central bone, which was obtained from the lumbar vertebrae at the level of L1-4, where the bone mineral density is measured the most frequently, and from the femur, which is significant for the prediction of osteoporosis (Kanis & Glüer, 2000; Yang, 2008). An anthropomorphic phantom was scanned daily for calibration of DXA. Precision of the DXA was monitored using the same phantom, and fluctuation was found to be less than 1%.
Bone mineral density is expressed as BMD in units of g/cm2 and the standardized T-score, an indicator of the absolute risk for fracture. The T-score is calculated from a formula: (measurements obtained from subjects-mean values obtained from young healthy adults)/SD (standard deviation). The T-scores for normal bone, osteopenia (or lower-than-normal bone mass), and osteoporosis are >-1.0, -1.0≤T-score<-2.5, and ≥-2.5, respectively. The BMD was measured by a well-trained radiology technician at a public healthcare center, whose results were interpreted by the investigators together with a physician from a public healthcare center.
Current height was measured after asking the subjects remove their shoes, raise their heels, buttocks, and waist upwards, and keep their head facing straight forward. Subjects took a deep breath and then their height was measured following relaxation and exhalation. The current height was measured in all subjects. Subjects were then asked to recall their maximum height from when they were younger before their current height was measured. Then, the recall data were recorded only for those subjects with a vivid memory of their maximum height.
The data were thus collected similarly to studies that were conducted to confirm the relationships between bone mineral density, vertebral shape, and height, and to examine whether there was a decrease in the height recalled over the previous 20 years (Nicholson, Haddaway, Davie, & Evans, 1993; Moayyeri et al., 2006; Siminoski, Washawski, Jen, & Lee, 2006), and methods for recalling height at the age of 25 years, as used in a study using a questionnaire or a interview (Ismail et al., 1999; Tobias et al., 2007). The height loss was calculated by subtracting the current measurement of height from the recalled maximum height.
For the data collection, the senior executive director of a public healthcare center with activities associated with the healthcare promotion for residents in the city of Seoul, and the general manager of the department of radiology were given an explanation regarding the purpose and intent of this study. They then provided informed consent to collect the data from subjects who were registered on a bone densitometry program. Each subject was asked for her recalled maximum height. Next, their height was measured using an automatic height-measuring device, and then her BMD was measured.
In order to minimize recall bias, 164 of all the subjects were excluded from the estimated height analysis due to the inability to accurately measure their height because of a recent fracture or an inability to remember their maximum height immediately or accurately. Thus, the estimated height loss analysis used the data only from 568 subjects (rate of rejection is 22.4%). Furthermore, the subjects had to recall their maximum height before measuring their current height and bone density in order to prevent the influence of their present measurement on their memory.
Prior to the initiation of data collection, an explanation regarding the objectives and necessity of the current study for research purposes was provided to the subjects, who then gave their informed consent to participate. The subjects were also assured that their data would be used solely for research and analysis, and that their personal information would be kept strictly confidential. They were also informed of their right to voluntarily withdraw from the study at any time. For further analysis of the data, the results of the BMD were provided in an anonymous manner.
An analysis of the collected data was performed using the SPSS-WIN (12.0) statistical program, where were analyzed using descriptive statistics. ANOVA and Pearson's correlation analysis were also performed to identify the relationship between age, bone mineral density, and height loss. T-score was used in the analyses to enable differentiation between the different BMD statuses (in terms of osteoporosis vs osteopenia vs normal). The odds ratio (OR) of developing osteoporosis was analyzed using a logistic regression analysis, where the dependent variables were set based on a cut-off T-score of -2.5 for discriminating osteoporosis.
BMI and the maximum height were adjusted in the logistics analysis process. The age variable had the multicollinearity with height loss variable. So the age variable was deleted because other variables lost their roles when the variables with high collinearity were applied (Collinearity Statistics: Tolerance=.11, VIF=9.15). For the odds ratio, the first variable (age) estimated the dependent variable and the second variable (height reduction) judged the remaining variances. In this case, the correlation among variables is high so that almost no variance which can be described by the second variable(height loss) is left after the description by the first variable (age). Accordingly, the analysis was done after deleting the age variable naturally increasing. Subjects were divided into four groups based on their height loss as follows: no loss, 1 cm, 2 cm, 3 cm and ≥4 cm. This was followed by a comparison between the four groups using odds ratios (ORs). The estimated height loss was classified by 1 cm unit.
For the usefulness of height loss to detect osteoporosis, the discriminative ability was evaluated by the size of area under curve (AUC) using receiver operating characteristics (ROC). AUC indicates the ability to discriminate the osteoporotic status (.90-1: excellent/ .70-.90: good/ .50-.70: poor/ .50: fail) (Song, 2009). The sensitivity in the ROC curve is the actual number of patients among those with osteoporosis. The specificity is calculated by the number of patients among those without osteoporosis. The overall discriminative index for test results is calculated by the positive likelihood ratio (LR+, sensitivity/(1-specificity). The LR+ of height loss was calculated by the ratio between those with osteoporosis and those without osteoporosis.
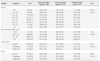
As given Table 1, the greatest proportion of the subjects (n=166, 22.7%) were aged between 60 and 65 years, followed by 55-60 years (17.3%), 65-70 years (16.7%), 50-55 years (15.6%), 70-75 years (9.8%), 45-50 years (8.6%), 45 years or younger (5.9%), and 75 years or older (3.4%). Thus, approximately three-quarters of the entire cohort were aged between 50 and 70 years old.
Subjects recalled maximum heights of 155.8-160.4 cm across the age groups, and their current heights were 148.3-159.4 cm. Height appeared to decrease with increasing age; that is, people become shorter as they age. In the entire cohort, height decreased by 0.41-4.0 cm on average compared to their previously recalled maximum. There was a significant difference between age and estimated height loss (F=27.68, p<.001).
According to World Health Organization guidelines, one of the risk factors associated with osteoporosis, the body mass index (BMI, kg/m2), cannot be applied to the Korean population because it was proposed specifically for Caucasian people (Yu, 2001). However, the Korean Society for the Study of Obesity proposed the following cut-off values for Koreans: underweight, BMI<18.5; normal weight, 18.5<BMI<23; overweight, 23<BMI<25; and obese, BMI≥25. Of the subjects in the present study, 1.4% were underweight, 39.4% were of normal weight, 27.2% were overweight, and 32.0% were obese. Thus, subjects with a 'normal' weight were the most prevalent. There was a significant difference between BMI and estimated height loss (F=6.50, p<.001).
Based on the bone mineral density in their lumbar vertebrae (T-score), 275 women (38.0%) had an osteopenic status, 238 women (32.8%) had a normal status and 212 women (29.2%) had an osteoporotic status. Thus, the distribution of bone mineral densities among our subjects did not deviate from normal. However, 413 women (56.5%) had an osteopenic status in the femur, 181 women (24.8%) had an osteoporotic status, and 137 women (18.7%) had a normal status. Thus, there appeared to be a higher proportion of our subjects with an osteopenic status in the femur as compared with the lumbar vertebra. There was a significant difference between bone mineral density and estimated height loss (lumbar: F=17.35, p<.001, femur: F=43.98, p<.001).
There was an age-dependent tendency toward a reduction in the mean BMD in both the lumbar vertebra and the femur. There was a statistically significant difference between age and BMD (lumbar: F=37.88, p<.001; femur: F=54.27, p<.001) (Figure 1).
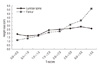
There was a significant negative correlation between bone mineral density and estimated height loss (lumbar, r=-.23, p<.001; femur, r=-.34, p<.001) (Figure 1). The estimated height loss increased further when the BMD decreased. As shown in Figure 2, there was a significant relationship between bone mineral density, as expressed using the standardized T-score, and height loss (lumbar, F=4.60, p<.001; femur, F=12.99, p<.001). A lower bone mineral density had a greater influence on height loss in the femur than in the lumbar vertebrae.
The estimated height loss was 2 cm (i.e., the greatest loss) 130 (22.9%) of the women, ≥4 cm in 122 (21.5%), 1 cm in 116 (20.4%), 'no loss' in 116 (20.4%), and 3 cm in 84 (14.8%).
The odds ratio (OR) at which estimated height loss affects the occurrence of osteoporosis was determined using logistic linear regression analysis. This regression analysis revealed χ2=57.33 (p<.001) and -2LL=589.23 in the lumbar vertebra and χ2=78.68 (p<.001) and -2LL=473.48 in the femur, indicating that the current model would be appropriate.
The OR of developing osteoporosis in the lumbar vertebrae increased by approximately two or three times (OR=2.64, 2.88, and 3.29) when the height was decreased by 2, 3, and ≥4 cm, respectively, as compared with cases in which there was no decrease in height. However, in the femur the OR of developing osteoporosis was found to increase by 2.96, 3.40, and 10.94 times when the height was decreased by 2, 3, and ≥4 cm, respectively. Thus, the risk of developing osteoporosis was approximately four times higher in cases in which the height was decreased by more than 4 cm than when the decrease was only 2 cm. These results indicate that the OR of developing osteoporosis was markedly higher in the femur than in the lumbar vertebra. When the height loss was approximately 1 cm, there was no statistically significant OR of developing osteoporosis. The OR of developing osteoporosis was found to be significantly higher at all other values of height loss except for this value of 1 cm (Table 2)
Table 3 shows the result using AUC to verify the discriminative ability of estimated height loss to detect osteoporosis. AUC was .71 (SE=.03, p<.001, 95% CI, 0.66-0.77) in Lumbar and .82 (SE=.02, p<.001, 95% CI, 0.78-0.87) in Femur. In accordance with ROC results, the value multiplying sensitivity by specificity at the point of height loss 2cm showed the highest increase and from the same point, the increase amount was significantly reduced (lumbar: sensitivity=81.6%, specificity=50.6%, femur: sensitivity=92.4%, specificity =50.2%). The positive likelihood ratio (LR+) was 1.7 and 1.9 in lumbar and femur at the point of 2 cm, respectively. Sensitivity, specificity and positive likelihood ratio (LR+) depending on cutoff value of height loss were 93.9%, 25.4% and 1.3 at 1cm, 55.1%, 70.3% and 1.9 at 3 cm, and 36.1%, 83.6% and 2.2 at 4cm or higher in lumbar, respectively. They were 99.0%, 22.8% and 1.3 at 1cm, 71.4%, 71.7% and 2.5 at 3 cm and 55.2%, 86.2% and 4.0 at 4.0 or higher in femur, respectively.
Our results showed that bone mineral density which is the total bone mass accounting for 15-17% of the body weight (Kim, 2001) decreased with increasing age. This concurs with the suggestion backed up by previous research (Milliken et al., 2009; Versluis et al., 1999; Yoshimura et al., 2008) that there is no equilibrium of bone remodeling with age. In women in particular, this can be explained by estrogen deficiency due to the decreased ovarian function associated with menopause, which has the effect of markedly increasing the rate of bone loss, followed by a subsequent age-related gradual reduction in osteogenic function, leading to the continuation of that bone loss.
We found that the estimated height loss increased with age. Yoshimura et al. (2008) reported that 299 of 400 patients experienced a reduction in height. According to a study conducted on 1,270 middle-aged Norwegian people and 494 Dutch women, the magnitude of height loss also increased in an age-dependent manner (Joakimsen et al., 1998; Versluis et al., 1999). Our findings are in agreement with these reports, suggesting the existence of correlations between aging, decreased bone mineral density, and height loss.
In our series the magnitude of estimated height loss increased when the bone mineral density was decreased. These results are consistent with previous authors postulating that the magnitude of height loss was greater in subjects with a vertebral deformity, one of the hallmarks of osteoporosis, and height is an indicator for vertebral fracture, one of the conditions of osteoporotic status (Ismail et al., 1999; Nicholson et al., 1993). These results indicated that the height loss could be one of the major factors for low bone density.
In the present study, the risk of developing osteoporosis was found to increase at a height-loss cut-off value of 2 cm. However, in the femur the risk of developing osteoporosis was five times higher at a height-loss cut-off value of 4 cm than 2 cm. In a multinational study conducted by Siminoski et al. (2005) involving 985 postmenopausal women, the risk of developing osteoporosis was 13.5 times higher (i.e., OR) in cases with a height loss of 2.0-3.0 cm, and 20.6 times higher in those with a height loss greater than 4 cm. These values are higher than found in the present study, a difference that might be attributable to the distribution of elderly subjects. According to another multinational study conducted by Krege et al. (2006) involving 2,127 women with osteoporosis from 25 countries, the risk of developing osteoporosis increased by more than 3 times at a height-loss cut-off value of >2 cm.
As described above, multinational studies involving larger samples found that the risk of developing osteoporosis increased at a height-loss cut-off value of 2 cm. The height loss value identified in this study was also similar to the results in those studies.
In accordance with the analysis using an AUC (area under curve), it was found that the AUC sizes of both the value of the lumbar and femur for all results were good. Thus, the estimated height loss has good discriminative ability for osteoporosis. AUC was 0.66 in the research by Siminoski et al. (2006) and 0.74 including other risk factors in the research by Tobias et al. (2007). These studies support our results which indicated that height loss would have discriminative ability for detection of osteoporosis. For positive likelihood ratio (LR+) with high clinical practicality as the general index to distinguish the results, it is considered that the discriminant power is good when LR+ is higher than 1 at the significance level 95%. In accordance with the analysis results using LR+, LR+ was higher than 1 at cutoff values of all height losses. However, since 1cm is not significant in logistic analysis, it can't be the basis to determine the occurrence of osteoporosis and significantly increased from the point 2 cm. the change of the value multiplying sensitivity and specificity around the point 2 cm was also changed. At the same time, LR+ was higher than 1. Accordingly, it was confirmed that the optimal cutoff value was the height loss point 2 cm. The higher height loss was, the more sensitivity dropped and specificity increased. The same patterns were observed in the study by Siminoski et al. (2006), estimating the occurrence ratio of osteoporotic fracture. The higher the height loss was, the higher the discriminant power on occurrence of osteoporosis was. It is considered as the natural consequence.
However, the risk of developing osteoporosis or an osteoporotic fracture increased at a height-loss cut-off value of >3.2 cm in 123 Australian women (Center et al., 1998) and at a cut-off value of >3.3 cm in 540 British women (Tobias et al., 2007). According to these studies conducted solely on Caucasian people, who are on average taller than Koreans, the risk of developing osteoporosis increased at a height-loss cut-off value of approximately 3 cm. Studies conducted on European subjects (Meyer et al., 1995) and Norwegian middle-aged subjects (Joakimsen et al., 1998) have shown that the incidence of osteoporosis or an osteoporotic fracture is higher in tall people and the height loss rate of tall people is higher than that of shorter people (Sorkin et al., 1999). It can therefore be inferred that height loss varies depending on the initial maximum height.
In 397 Japanese subjects aged between 27 and 101 years, the height loss was found to be 3.9 cm on a 2-year regular check-up. Based on these results, height loss exceeding 4 cm was proposed as criteria for determining the occurrence of osteoporosis (Masunari et al., 2007). A study conducted on 457 Iranian subjects found that the T-score was lower in subjects in whom the height loss was greater than 5 cm (Moayyeri et al., 2006). However, it should also be noted that the degree of height loss was higher in a Hiroshima cohort, even though Japanese people being shorter than Caucasians, which might be due to regional differences, or the subjects consisting of super-elderly people. For Iranians, the folk costume covering the entire body may be one of the reasons for high prevalence of vitamin D deficiency (the prevalence rate of moderate vitamin D deficiency was 57.6%. Moayyeri et al., 2006). Preventing the exposure under the sunlight causes deficiency of vitamin D generated on the skin and so interrupts absorption of Ca. Accordingly, it reduces bone density. Thus, blocking exposure to sunlight can be the reason for height loss. This warrants further study.
As a result, it is expected that height-loss cut-off values of 2 cm, which were also suggested by the International Society of Clinical Densitometry (Vokes et al., 2006), will be advocated by further studies conducted using Korean cohorts, and then established as criteria for the prediction of osteoporosis. However, in the current situation where there was currently no reliable reference range of height-loss cut-off values for the occurrence of osteoporosis, this study was conducted under conditions in which two-thirds of the cohort were concentrated in the 50-70 years age group, a time of life during which there are abrupt changes in bone metabolism, and the sample was relatively large. Thus, we suggest that the height-loss cut-off value of 2.0 cm can be used as a reliable indicator for predicting the risk of developing osteoporosis.
The estimated height loss is useful as an early detection index for osteoporosis. Accordingly, it is imperative for women with a high risk of osteoporosis to identify their height loss and so find out their osteoporotic state earlier. The indirect confirm on the bone density by self measurement of height will encourage the subjects to participate in various types of programs including leisure-time physical activities and exercise therapy more actively. An MRI study showed that bone height was negatively correlated with aging (Pfirmann, Metzdorf, Elfering, Hodler, & Boos, 2006). Height, bone loss, or aging may be a natural phenomenon which is experienced simultaneously. The inter-variable effects on height loss require further study.
In most cases, people who are relatively young undergo more frequent measures of height allowing height change to be identified after a lapse of a certain period. The recalled maximum height used in this study did not include the height records measured more than 20 years ago. Recall was minimized by excluding data from those subjects who could not accurately remember their height from 20 years previously. The main limitation of this study is that the data of maximum height was gathered only from the memory of subjects. Additionally, the subjects were collected only from one healthcare center. Although it is possible that this finding would apply to other groups, such generalizations should be made with caution.
This study suggested the usefulness of height loss as a factor to estimate the risk of occurrence of osteoporosis and provided the motivation to continue to measure and record height. This finding, which take into consideration the anthrophometric features of Koreans, also help the public to easily recognize that a change in height is a risk factor and may indicate an increased probability of osteoporosis. Furthermore, it is required to make the subjects measure height loss on a regular basis and be aware of the necessity of height measurement. Such behaviors will be used as the strategy to prevent osteoporosis. In addition, when the height measurement results from the health examination which National Health Insurance Corporation requested the public to take every second year are accumulated for at least 20 years, the results will be more objective height loss data.
It is expected to result in more effective preventive care for osteoporosis by extensive application of height measurement as a self assessment tool on osteoporotic status.
In the present study, the estimated height loss underwent significant further increase when the BMD decreased. At a height-loss of 2cm, the odds ratio (OR) for an increasing occurrence of osteoporosis increased in both the lumbar and femur. It showed good discriminative ability and a good positive likelihood ratio at the same point. As a result, it was verified that a height loss of 2cm was the optimal cut-off value for detection of osteoporosis.
Estimated height loss is useful as an early detection index for osteoporosis. This study confirmed the usefulness of height loss as a factor for estimating the risk of occurrence of osteoporosis and provided motivation for measurement on a regular basis. This study suggests that in depth education is needed about the changes during a person's life span in height and bone density. An identical research conducted on men would help confirm the height change patterns of Koreans. Nursing practices require the detailed and standard height measurement manual for using accurate height data. Using height measurements in clinical and community settings and in daily life like on a driver's license would help people realize decreases in height to prevent osteoporosis.
Figures and Tables
Figure 1
Bone mineral density and estimated height loss by age (N=732).
Bone mineral density (BMD) is significant different from the age (Lumbar spine: F=37.88, p<.001, Femur: F=54.27, p<.001); The correlation BMD and height loss is negatively significant (Lumbar spine: r=-.23, p<.001, Femur: r=-.34, p<.001).
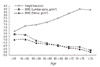
Figure 2
Estimated height loss by bone mineral density (N=568).
T-score is absolute value (ex: l T-score l 2.5 → -2.5); Estimated height loss is significant different from T-score (Lumbar spine: F=4.60, p<.001; Femur: F=12.99, p<.001).
References
1. Adachi JD, Ioannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, et al. The influence of osteoporotic fractures on health-related quality of life in community dwelling men and women across Canada. Osteoporosis International. 2001. 12:903–908. doi: 10.1007/s001980170017.
2. Center JR, Nguyen TV, Pocock NA, Noakes KA, Kelly PJ, Eisman JA, et al. Femoral neck axis length, height loss, and risk of hip fracture in males and females. Osteoporosis International. 1998. 8:75–81. doi: 10.1007/s001980050051.
3. Francis RM, Aspray TJ, Hide G, Suteliffe AM, Wilkinson P. Back pain in osteoporotic vertebral fractures. Osteoporosis International. 2008. 19:895–903. doi: 10.1007/s00198-007-0530-x.
4. Ismail AA, Cooper C, Felsenberg D, Varlow J, Kanis JA, Silman AJ, et al. Number and type of vertebral deformities: Epidemiological characteristics and relation to back pain and height loss. Osteoporosis International. 1999. 9:206–213. doi: 10.1007/s001980050138.
5. Joakimsen RM, Fønnebø V, Magnus JH, Tollan A, Johanne Søgaard A. The Tromsø study: Body height, body mass index and fractures. Osteoporosis International. 1998. 8:436–442. doi: 10.1007/s001980050080.
6. Kanis JA, Glüer CC. An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporosis International. 2000. 11:192–202. doi: 10.1007/s001980050281.
7. Kim KS. The 4th summing-up in osteoporosis, 2001: Physiology of the bone. 2001. Seoul: The Korean Society of Bone Metabolism;9–12.
8. Health and welfare reports-domestic. Korea Institute for Health and Social Affairs. 2010a. Retrived March 10, 2010. from http://www.kihasa.re.kr/html/jsp.
9. Health and welfare reports-domestic. Korea Institute for Health and Social Affairs. 2010b. Retrived January 27, 2010. from http://www.kihasa.re.kr/html/jsp.
10. Krege JH, Siminoski K, Adachi JD, Misurski DA, Chen P. A simple method for determining the probability a new vertebral fracture is present in postmenopausal women with osteoporosis. Osteoporosis International. 2006. 17:379–386. doi: 10.1007/s00198-005-2005-2.
11. Masunari N, Fujiwara Y, Nakata E, Nakashima E, Nakamura T. Historical height loss, vertebral deformity, and health related quality of life in Hiroshima cohort study. Osteoporosis International. 2007. 18:1493–1499. doi: 10.1007/s00198-007-0392-2.
12. Meyer HE, Falch JA, O'Neill T, Tverdal A, Varlow J. Height and body mass index in Oslo, Norway, compared to other regions of Europe: Do they explain differences in the incidence of hip fracture? Bone. 1995. 17:347–350. doi: 10.1016/s8756-3282(95)00245-6.
13. Milliken LA, Cussler E, Zeller RA, Choi JE, Metcalfe L, Going SB, et al. Changes in soft tissue composition are the primary predictors of 4-year bone mineral density changes in postmenopausal women. Osteoporosis International. 2009. 20:347–354. doi: 10.1007/s00198-008-0664-5.
14. Moayyeri A, Ahmadi-Abhari S, Hossein-nezhad A, Larijani B, Soltani A. Bone mineral density and estimated height loss based on patients' recalls. Osteoporosis International. 2006. 17:834–840. doi: 10.1007/s00198-005-0046-1.
15. Nicholson PHF, Haddaway MJ, Davie MWJ, Evans SF. Vertebral deformity, bone mineral density, back pain and height loss in unscreened women over 50 years. Osteoporosis International. 1993. 3:300–307. doi: 10.1007/BF01637315.
16. North American Menopause Society. Management of osteoporosis in postmenopausal women: Position statement of the North American Menopause Society. Menopause. 2006. 13:340–367.
17. Park IH. The 7th osteoporosis summing-up: Diagnosis of osteoporosis. 2004. Seoul: The Korean Society of Bone Metabolism;7–12.
18. Park HM. Phytoestrogen. 2005. Seoul: Koonja.
19. Pfirrmann CWA, Metzdorf A, Elfering A, Hodler J, Boos N. Effect of aging and degeneration on disc volume and shape: A quantitative study in asymptomatic volunteers. Journal of Orthopaedic Research. 2006. 24:1086–1094. doi: 10.1002/jor.20113.
20. Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. Reduced pulmonary function in patients with spinal osteoporotic fracture. Osteoporosis International. 1998. 8:261–267. doi: 10.1007/s001980050063.
21. Siminoski K, Jiang G, Adachi JD, Hanley DA, Cline G, Ioannidis G, et al. Accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporosis International. 2005. 16:403–410. doi: 10.1007/s00198-004-1709-Z.
22. Siminoski K, Washawski RS, Jen K, Lee K. The accuracy of historical height loss for the detection of vertebral fractures in postmenopausal women. Osteoporosis International. 2006. 17:290–296. doi: 10.1007/s00198-005-2017-y.
23. Song SW. Using the receiver operating characteristic curve to measure sensitivity and specificity. Korean Journal of Family Medicine. 2009. 30:841–842. doi: 10.4082/kjfm.2009.30.11.841.
24. Sorkin JD, Muller DC, Andres R. Longitudinal change in height of men and women: Implications for interpretation of the body mass index. American Journal of Epidemiology. 1999. 150:969–977.
25. Tobias JH, Hutchinson AP, Hunt LP, McCloskey EV, Stone MD, Martin JC, et al. Use of clinical risk factors to identify postmenopausal women with vertebral fractures. Osteoporosis International. 2007. 18:35–43. doi: 10.1007/s00198-006-0209-8.
26. Versluis RG, Petri H, van de Ven CM, Scholtes AB, Broerse ER, Springer MP, et al. Usefulness of armspan and height comparison in detecting vertebral deformities in women. Osteoporosis International. 1999. 9:129–133. doi: 10.1007/s001980050125.
27. Vokes T, Bachman D, Baim S, Binkley N, Broy S, Ferrar L, et al. Vertebral fracture assessment: The 2005 ISCD official position. Journal of Clinical Densitometry. 2006. 9:37–46. doi: 10.1013/j.jocd.2006.05.006.
28. Yang SG. The 8th osteoporosis summing-up: Diagnosis of the osteoporosis. 2008. Seoul: The Korean Society of Bone Metabolism;99–113.
29. Yoshimura N, Kinoshita H, Takijiri T, Oka H, Muraki S, Mabuchi A, et al. Association between height loss and bone loss, cumulative incidence of vertebral fractures and future quality of life: The Miyama study. Osteoporosis International. 2008. 19:21–28. doi: 10.1007/s00198-007-0474-1.
30. Yu HJ. Training course 2001: Diagnosis of obesity. 2001. Seoul: Korean Society for the Study of Obesity;5–9.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download