Abstract
Purpose
The purpose of this study was to evaluate the effectiveness of the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISSIT) model sexual program on female sexual function for women with gynecologic cancer.
Methods
The integrative 6-hr (two hours per session) program reflecting physical and psychosocial aspects of women's sexuality was developed based on Annon's PLISSIT model. Participants were 61 women with cervical, ovarian, or endometrial cancer. Of them, 29 were assigned to the experimental group and 32 to the control group. The women completed the Female Sexual Function Index (FSFI) including sexual desire, arousal, lubrication, orgasm, satisfaction, and pain. Independent t-test and repeated measured ANOVA were used to test the effectiveness of the program.
Results
Significant group differences were found on FSFI sub-domain scores including sexual desire, arousal, lubrication, orgasm, and satisfaction but not pain. Significant time differences were found on all domains except for pain in the experimental group repeated measured ANOVA.
Conclusion
The results indicate that the three-week PLISSIT model sexual program is effective in increasing sexual function for women with gynecologic cancer. Nurses may contribute to improving women's sexual function by utilizing the program. Strategies to relieve sexual pain need to be considered for greater effectiveness of the program.
Figures and Tables
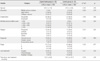
Table 2
General and Medical Characteristics and Homogeneity between Experimental and Control Group (N=61)
References
1. Annon JS. The PLISSIT model: A proposed scheme for the behavioral treatment of sexual problems. Journal of Sex Education and Therapy. 1976. 2:1–15.
2. Ayaz S, Kubilay G. Effectiveness of the PLISSIT model for solving the sexual problems of patients with stoma. Journal of Clinical Nursing. 2008. 18:89–98. doi: 10.1111/j.1365-2702.2008.02282.x.
3. Bancroft J, Loftus J, Long JS. Distress about sex: A national survey of women in heterosexual relationship. Archives of Sexual Behavior. 2003. 32:193–208. doi: 10.1023/A:1023420431760.
4. Brotto LA, Heiman JR, Goff B, Greer B, Lentz GM, Swisher E, et al. A psychoeducational intervention for sexual dysfunction in women with gynecologic cancer. Archives of Sexual Behavior. 2008. 37:317–329. doi: 10.1007/s10508-007-9196-x.
5. Chun N. A structural equation model on sexual function in women with gynecologic cancer. Journal of Korean Academy of Nursing. 2008. 38:639–648. doi: 10.4040/jkan.2008.38.5.639.
6. Chun N. Predictors of sexual desire, arousal, lubrication, orgasm, satisfaction, and pain in women with gynecologic cancer. Journal of Korean Academy of Nursing. 2010. 40:24–32. doi: 10.4040/jkan.2010.40.1.24.
7. Chun N, Kwon JY, Noh GO, Kim SH. Symptom clusters in women with gynecologic cancer. Clinical Nursing Research. 2006. 14:61–70.
8. Cohen J. Statistical power analysis for the behavior sciences. 1988. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc.
9. Jensen PT, Groenvold M, Klee MC, Thranov I, Petersen MA, Machin D. Longitudinal study of sexual function and vaginal changes after radiotherapy for cervical cancer. International Journal of Radiation Oncology, Biology, Physics. 2003. 56:937–949. doi: 10.1016/S0360-3016(03)00362-6.
10. Jun EY, Kim S, Chang SB, Oh K, Kang HS, Kang SS. The effect of a sexual life reframing program on marital intimacy, body image, and sexual function among breast cancer survivors. Cancer Nursing. 2011. 34:142–149. doi: 10.1097/NCC.0b013e3181f1ab7a.
11. Katz A. Do ask, do tell, why do so many nurses avoid the topic of sexuality? American Journal of Nursing. 2005. 105:66–68.
12. Krychman ML. Sexual rehabilitation medicine in a female oncology setting. Gynecologic Oncology. 2006. 101:380–384. doi: 10.1016/j.ygyno.2006.03.001.
13. Ministry of Health and Welfare. Annual report of cancer statistics in Korea in 2008, the Korea central cancer registry, National Cancer Center. 2010. 12. Seoul: Author.
14. Nichols FH, Humenick SS. Childbirth Education. 2000. 2nd ed. Philadelphia, PA: W. B. Saunders.
15. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex and Marital Therapy. 2000. 26:191–208. doi: 10.1080/009262300278597.
16. Speer JJ, Hillenberg B, Sugrue DP, Blacker C, Kresge CL, Decker VB, et al. Study of sexual functioning determinants in breast cancer survivors. The Breast Journal. 2005. 11:440–447. doi: 10.1111/j.1075-122X.2005.00131.x.
17. Stead ML. Sexual function after treatment for gynecological malignancy. Current Opinion in Oncology. 2004. 16:492–495.
18. Stead ML, Brown JM, Fallowfield L, Selby P. Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. British Journal of Cancer. 2003. 88:666–671. doi: 10.1038/sj.bjc.6600799.
19. Stewart DE, Wong F, Duff S, Melancon CH, Cheung AM. "What doesn't kill you makes you stronger": An ovarian cancer survivor survey. Gynecologic Oncology. 2001. 83:537–542. doi: 10.1006/gyno.2001.6437.
20. Takahashi M, Kai I. Sexuality after breast cancer treatment: Changes and coping strategies among Japanese survivors. Social Science and Medicine. 2005. 61:1278–1290. doi: 10.1016/j.socscimed.2005.01.013.
21. Schultz WC, Van De Wiel HB. Sexuality, intimacy, and gynecological cancer. Journal of Sex and Marital Therapy. 2003. 29:121–128.
22. Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): Cross-validation and development of clinical cutoff scores. Journal of Sex and Marital Therapy. 2005. 31:1–20. doi: 10.1080/0092623059- 0475206.
23. Yu HS. Predictors of female sexual dysfunction. 2003. Seoul: Seoul National University;Unpublished master's thesis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download