Abstract
Background
Hypertension and age are recognized as important risk factors for left ventricular (LV) diastolic dysfunction. Some studies have shown that diabetes itself may also be an independent risk factor for LV diastolic dysfunction, although this is controversial. The aim of this study was to determine the factors associated with LV diastolic dysfunction in patients with type 2 diabetes in the absence of hypertension or ischemic heart disease (IHD).
Methods
Participants in this study consisted of 65 type 2 diabetes patients (M : F = 45 : 20; mean age 51 [26 to 76] years; mean body mass index [BMI] 25.0 ± 2.5 kg/m2) without hypertension, heart disease, or renal disease. Individuals with ischemic electrocardiographic changes were excluded. LV diastolic function was evaluated by Doppler echocardiographic studies.
Results
Fifteen patients (23.1%) showed LV diastolic dysfunction on Doppler echocardiographic studies. Patients with LV diastolic dysfunction were older than those without diastolic dysfunction (60.0 ± 2.5 vs. 50.5 ± 1.9 years; P < 0.01). After adjusting for age and sex, BMI was higher (26.6 ± 0.7 vs. 24.6 ± 0.3 kg/m2; P < 0.01) and diabetes duration was longer (9.65 ± 1.48 vs. 4.71 ± 0.78 years; P < 0.01) in patients with LV diastolic dysfunction than in those without diastolic dysfunction. There were no differences in sex, smoking, blood pressure, lipid profiles, hemoglobin A1C, fasting glucose, fasting insulin, or diabetic microvascular complications between the LV diastolic dysfunction group and the normal diastolic function group. After adjusting for age, sex, and BMI, diabetes duration was found to be independently associated with LV diastolic dysfunction (odds ratio 1.38; confidence interval 1.12 to 1.72; P = 0.003).
Heart failure is a common comorbidity and fatal complication of diabetes mellitus. The Framingham heart study demonstrated an increased risk of heart failure in patients with diabetes: a two-fold higher incidence in men and a five-fold higher incidence in women with diabetes compared with age-matched non-diabetic subjects [1]. Many epidemiological studies have confirmed a significantly increased prevalence of cardiac dysfunction in diabetic patients, independent of the influence of relevant covariates [2-4]. Left ventricular (LV) diastolic dysfunction is thought be an early preclinical manifestation of heart failure [5]. The incidence of diastolic dysfunction in diabetic patients has been demonstrated to be 30-75% in recent studies [6-8].
Considering the high prevalence and significant morbidity and mortality of heart failure in patients with type 2 diabetes, identification of risk factors for LV diastolic dysfunction and an index of early-stage diabetic cardiomyopathy are necessary to delay or prevent the onset of heart failure. Age, hypertension, and ischemic heart disease (IHD) are thought to be important risk factors for diastolic dysfunction in both patients with diabetes and non-diabetics [9-11]. Although several studies have shown that poor glycemic control and longer duration of diabetes may be associated with early diastolic dysfunction in type 2 diabetes [12-14], there have been few studies on the factors associated with LV diastolic dysfunction in type 2 diabetes without hypertension or IHD. Therefore, we sought to determine the risk factors associated with subclinical LV diastolic dysfunction in type 2 diabetic patients without hypertension or IHD.
This study was approved by the Institutional Review Board of Ilsan-Paik Hospital. The study subjects consisted of 65 type 2 diabetic patients without hypertension or IHD (M : F = 45 : 20; mean age 51 [26-76] years; mean body mass index [BMI] 25.0 ± 2.5 kg/m2) who initially visited the outpatient diabetes clinic at Inje University Ilsan-Paik Hospital between January 2006 and April 2006. Inclusion criteria were: i) normal arterial blood pressure (< 130/85 mm Hg) without antihypertensive medication, ii) no symptoms or signs of heart disease, iii) no history of coronary heart disease (stable angina, unstable angina, myocardial infarction, or revascularization) or valvular heart disease, iv) sinus rhythm and no evidence of IHD on resting 12-lead ECG, v) no evidence of severe medical illness including liver cirrhosis, end-stage renal disease, or cancer. Patients were excluded from participation in the study if either of the following criteria applied: i) diabetes diagnosed before the age of 26, or ii) history of type 1 diabetes or diabetic ketoacidosis.
Height and weight were measured in the morning with the subjects wearing light clothing but no shoes. Blood pressure was measured with a mercury sphygmomanometer on the right arm with the subjects in a sitting position after a 5-minute rest. BMI was calculated as weight in kilograms divided by the square of the height in meters. Diabetes duration and diabetic complications were ascertained from review of medical records. Diabetic complications were recorded as retinopathy, neuropathy (absence of ankle jerks and reduced vibratory sensation, or impairment on nerve conduction studies or autonomic function tests), overt proteinuria (24 hour urine protein ≥ 300 mg/day), or microalbuminuria. Fasting plasma glucose (FPG), total cholesterol, high-density lipoprotein (HDL)-cholesterol, low-density (LDL)-cholesterol, lipoprotein a [Lp(a)], triglycerides, and uric acid were measured with an autoanalyzer (Beckman Coulter, Miami, FL, USA). Level of hemoglobin A1C (HbA1C) (high performance liquid chromatography; Tosoh, Tokyo, Japan), serum insulin (two-site chemiluminescent immunometric assay; Roche, Basel, Switzerland), and high-sensitivity C-reactive protein (hs-CRP, enzyme-linked immunosorbent assay; DRG Diagnostics, Marburg, Germany) were also measured.
All echocardiographic examinations were performed on a GE VingMed Vivid 5® Echocardiography System (GE Medical Systems, Milwaukee, WI, USA) with a 2.5 MHz transducer. All smokers were prevented from smoking for at least 30 minutes before the examination. The examination was performed while the patient was in a period of quiet respiration. Echocardiograms were stored digitally and analyzed by one examiner. All recordings were performed at a high sweep speed (100 mm/sec) with simultaneous electrocardiographic (ECG) recording and included complete M-mode, 2-dimensional, and Doppler echocardiographic examinations, with emphasis on evaluation of LV diastolic function [10-12]. For evaluation of diastolic myocardial function, mitral inflow velocities (E- and A-waves, cm/sec), deceleration time (DT), isovolumic relaxation time (IVRT), systolic (S) and diastolic (D) pulmonary venous forward flow, pulmonary venous atrial reversal velocity (Ar), and early (E') and late (A') diastolic velocity of mitral annulus were measured in compliance with the standard protocols [10-12]. Left ventricular systolic function was determined by estimation of left ventricular ejection fraction (LVEF). The normal range of LVEF was 65 ± 10%.
The following criteria were used for the diagnosis of LV diastolic function [15]: impaired relaxation pattern was defined as E/A ratio < 1.0 and DT > 200 ms; pseudonormal pattern as E/A ratio from 1.0 - 2.0 with at least two of the following: S/D ratio < 1, or Ar ≥ 35 cm/sec, or E' < A' and E/E' ratio > 10; and restrictive pattern as E/A ratio > 2.0 and DT < 150 ms. All diastolic dysfunctions in this study were impaired relaxation pattern.
Data are presented as mean ± SEM. Statistical analysis was performed using SPSS for Windows (SPSS Inc., Chicago, IL, USA). Differences in variables between patients with and without LV diastolic dysfunction were analyzed using Mann-Whitney test and Fisher's exact test. Analysis of covariance (ANCOVA) test was used for age and sex-adjusted characteristics according to the presence of diastolic dysfunction (Table 1). ANCOVA test was also used to assess the independent association of duration of diabetes with the presence of diastolic dysfunction, with age, sex, and BMI as covariates (Fig. 1). Logistic regression analysis was used to examine independent determinants for diastolic dysfunction, with age, sex, BMI, and duration of diabetes as covariates. All probability values were two-tailed, and statistical significance was defined as P < 0.05.
The median duration of diabetes for the study subjects was 5 years (range, 0 to 26). Mean HbA1C was 8.0 ± 2.1%. Fifteen patients (23.1%) showed diastolic dysfunction on Doppler echocardiographic studies. The characteristics of the patients with and without prevalent diastolic dysfunction are compared in Table 1. Patients with LV diastolic dysfunction were older than patients without LV diastolic dysfunction (60.0 ± 2.5 vs. 50.5 ± 1.9 years; P < 0.01). There was no difference in the sex ratio between the two groups. After adjusting for age and sex, BMI was found to be higher (26.6 ± 0.7 vs. 24.6 ± 0.3 kg/m2; P < 0.01) and diabetes duration was found to be longer (9.65 ± 1.48 vs. 4.71 ± 0.78 years; P < 0.01) in patients with LV diastolic dysfunction than in those without LV diastolic dysfunction. There were no differences in smoking, blood pressure, lipid profiles, HbA1C, fasting plasma glucose, fasting serum insulin, or diabetic microvascular complications between the LV diastolic dysfunction group and the normal LV diastolic function group. There was no difference between the two groups in medications for hyperglycemia or dyslipidemia, including thiazolidinediones, statins, and insulin (data not shown).
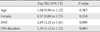
No subject had LV systolic dysfunction and no differences in LVEF were found between the LV diastolic dysfunction group and the normal LV diastolic function group (P = 0.18). The E/A ratio was lower in patients with LV diastolic dysfunction (0.70 ± 0.04 vs. 1.07 ± 0.29; P < 0.001). There were no significant differences in other parameters between the LV diastolic dysfunction group and the normal LV diastolic function group (Table 2).
Logistic regression analysis for diastolic dysfunction with age, sex, BMI, and diabetes duration as covariates showed that diabetes duration and BMI were independent determinants (Table 3). When participants were classified into four groups based on the duration of diabetes (≤ 1, > 1 and ≤ 5, > 5 and ≤ 10, > 10 years), the frequency of LV diastolic dysfunction increased with increasing duration of diabetes after adjusting for age, sex, and BMI (P for trend = 0.005; Fig. 1).
In the present study, we found that duration of diabetes was strongly associated with the presence of LV diastolic dysfunction in type 2 diabetic patients without hypertension or IHD. After adjusting for age, sex, and BMI, the frequency of LV diastolic dysfunction correlated positively with the duration of diabetes.
Some previous studies demonstrated LV diastolic dysfunction in normotensive patients with diabetes, and the existence of LV diastolic dysfunction in the absence of coronary artery disease and hypertension has been ascribed to diabetic cardiomyopathy [6-8]; however, there are very few studies on the factors associated with LV diastolic dysfunction in type 2 diabetes without hypertension or IHD. Aging and duration of diabetes were related to LV dysfunction in normotensive type 2 diabetic patients in a previous study [9], which demonstrated a similar results of the present study.
The proposed mechanisms of diabetic cardiomyopathy from animal studies are: i) excessive production of reactive oxygen species [16], ii) over-activation of poly-(ADP-ribose) polymerase [17], iii) increased activity of protein kinase C [18], iv) dysfunctional calcium handling in cardiomyocytes [19], and v) enhanced activity of the renin-angiotensin-aldosterone system [20]. Several studies have suggested that hyperglycemia alters the metabolism of cardiac myocytes and could be the primary insult in the pathogenesis of diabetic cardiomyopathy [21,22]. Even in type 2 diabetic patients without cardiac involvement, uncontrolled hyperglycemia is known to provoke diastolic LV dysfunction [12,13]. Nichols et al. [23] demonstrated that a reduction in HbA1C coupled with a lower baseline HbA1C was predictive of a decreased incidence of heart failure in a multivariate model, emphasizing the importance of glycemic control for prevention of heart failure.
Some data have suggested that diabetic cardiomyopathy could be one of the microvascular complications of diabetes related to endothelial dysfunction [21,24,25]. Considering that duration of diabetes is the strongest predictor for diabetic microvascular complications, the strong association of duration of diabetes with LV diastolic dysfunction observed in this study is plausible. In this study, the level of HbA1C was not associated with LV diastolic dysfunction, whereas diabetes duration was a significant determinant, suggesting that cumulative exposure to hyperglycemia may be important for the development of LV diastolic dysfunction.
Several studies have reported that obesity is associated with heart failure and ventricular dysfunction [26-29]. In a middle-aged African-American cohort, obesity was associated with concentric hypertrophy, which was strongly associated with diastolic dysfunction [30]. Another study found that reduced LV diastolic function was apparent in 24% of severely obese subjects, and that the risk was linearly associated with BMI [29]. However, the association of obesity with diastolic dysfunction, independent of other causes, remains controversial [5,31]. From the results of this study, we suggest that obesity may be associated with LV diastolic dysfunction independent of other clinical parameters related to diastolic dysfunction in type 2 diabetic patients without hypertension or IHD.
In this study, the prevalence of LV diastolic dysfunction was lower than in other studies [6-8], which could be because of the relatively short duration of diabetes, and our selection criteria excluding patients with hypertension or IHD. We did not find a significant association of diabetic microvascular complications such as retinopathy, nephropathy, and neuropathy with LV diastolic dysfunction, although frequencies of each microvascular complication tended to increase with the presence of LV diastolic dysfunction. This non-significant association may be explained by the earlier development of diabetic cardiomyopathy compared with other microvascular complications [32-34], relatively well-controlled hyperglycemia, short duration of diabetes, and selection criteria excluding patients with hypertension or IHD.
One limitation of our study is that it was cross-sectional and unable to suggest a causal relationship. Other limitations were the uncertainty of ischemic heart disease and diabetes duration. Our exclusion of IHD based on ECG and presence of symptoms might have not ruled out IHD completely. Besides, the onset of type 2 diabetes is not always clear, and previous medical records related to initial diagnosis were not available. Although the good correlation of diabetes duration with diabetic retinopathy (r = 0.516, P < 0.01) may lessen this concern, another prospective study for individuals with newly detected type 2 diabetes is needed to confirm the results of our study.
Despite the limitations of the study, our data showed that duration of diabetes could be a marker for LV diastolic dysfunction independent of other diastolic dysfunction-related variables in type 2 diabetic patients without hypertension or IHD.
Figures and Tables
Fig. 1
Frequency of LV diastolic dysfunction according to diabetes duration in type 2 diabetic patients without hypertension, after adjusting for age, sex, and BMI. LV, left ventricular; BMI, body mass index.

Table 1
Age, sex and age and sex-adjusted characteristics according to the presence of diastolic dysfunction in type 2 diabetic patients without hypertension

Table 2
Echocardiographic parameters
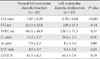
Data are expressed as mean ± SD.
E/A, the ratio of early and late left ventricular diastolic filling; DT, the E-wave deceleration time; IVRT, the isovolumic relaxation time; E' the early diastolic velocity by Tissue Doppler at lateral mitral annulus; A', the late diastolic velocity by Tissue Doppler at lateral mitral annulus; E/E', the ratio of E and E'; LVEF, left ventricular ejection fraction.
References
1. Kannel WB, McGee DL. Diabetes and cardiovascular disease: the Framingham study. JAMA. 1979. 241:2035–2038.
2. Raev DC. Which left ventricular function is impaired earlier in the evolution of diabetic cardiomyopathy? An echocardiographic study of young type 1 diabetic patients. Diabetes Care. 1994. 17:633–639.
3. Candido R, Srivastava P, Cooper ME, Burrell LM. Diabetes mellitus: a cardiovascular disease. Curr Opin Investig Drugs. 2003. 4:1088–1093.
4. Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993. 16:434–444.
5. Persson H, Lonn E, Edner M, Baruch L, Lang CC, Morton JJ, Ostergren J, McKelvie RS. Investigators of the CHARM Echocardiographic Substudy-CHARMES. Diastolic dysfunction in heart failure with preserved systolic function: need for objective evidence: results from the CHARM Echocardiographic Substudy-CHARMES. J Am Coll Cardiol. 2007. 49:687–694.
6. Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG. Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care. 2001. 24:5–10.
7. Zabalgoitia M, Ismaeil MF, Anderson L, Maklady FA. Prevalence of diastolic dysfunction in normotensive, asymptomatic patients with well-controlled type 2 diabetes mellitus. Am J Cardiol. 2001. 87:320–323.
8. Boyer JK, Thanigaraj S, Schechtman KB, Pérez JE. Prevalence of ventricular diastolic dysfunction in asymptomatic, normotensive patients with diabetes mellitus. Am J Cardiol. 2004. 93:870–875.
9. Masugata H, Senda S, Goda F, Yoshihara Y, Yoshikawa K, Fujita N, Daikuhara H, Okuyama H, Taoka T, Kohno M. Left ventricular diastolic dysfunction in normotensive diabetic patients in various age strata. Diabetes Res Clin Pract. 2008. 79:91–96.
10. Danielsen R. Factors contributing to left ventricular diastolic dysfunction in long-term type I diabetic subjects. Acta Med Scand. 1988. 224:249–256.
11. Nicolino A, Longobardi G, Furgi G, Rossi M, Zoccolillo N, Ferrara N, Rengo F. Left ventricular diastolic filling in diabetes mellitus with and without hypertension. Am J Hypertens. 1995. 8:382–389.
12. von Bibra H, Hansen A, Dounis V, Bystedt T, Malmberg K, Rydén L. Augmented metabolic control improves myocardial diastolic function and perfusion in patients with non-insulin dependent diabetes. Heart. 2004. 90:1483–1484.
13. Grandi AM, Piantanida E, Franzetti I, Bernasconi M, Maresca A, Marnini P, Guasti L, Venco A. Effect of glycemic control on left ventricular diastolic function in type 1 diabetes mellitus. Am J Cardiol. 2006. 97:71–76.
14. Celentano A, Vaccaro O, Tammaro P, Galderisi M, Crivaro M, Oliviero M, Imperatore G, Palmieri V, Iovino V, Riccardi G. Early abnormalities of cardiac function in non-insulin-dependent diabetes mellitus and impaired glucose tolerance. Am J Cardiol. 1995. 76:1173–1176.
15. Konduracka E, Gackowski A, Rostoff P, Galicka-Latala D, Frasik W, Piwowarska W. Diabetes-specific cardiomyopathy in type 1 diabetes mellitus: no evidence for its occurrence in the era of intensive insulin therapy. Eur Heart J. 2007. 28:2465–2471.
16. Wold LE, Ceylan-Isik AF, Fang CX, Yang X, Li SY, Sreejayan N, Privratsky JR, Ren J. Metallothionein alleviates cardiac dysfunction in streptozotocin-induced diabetes: role of Ca2+ cycling proteins, NADPH oxidase, poly(ADP-Ribose) polymerase and myosin heavy chain isozyme. Free Radic Biol Med. 2006. 40:1419–1429.
17. Minchenko AG, Stevens MJ, White L, Abatan OI, Komjáti K, Pacher P, Szabó C, Obrosova IG. Diabetes-induced overexpression of endothelin-1 and endothelin receptors in the rat renal cortex is mediated via poly(ADP-ribose) polymerase activation. FASEB J. 2003. 17:1514–1516.
18. Way KJ, Isshiki K, Suzuma K, Yokota T, Zvagelsky D, Schoen FJ, Sandusky GE, Pechous PA, Vlahos CJ, Wakasaki H, King GL. Expression of connective tissue growth factor is increased in injured myocardium associated with protein kinase C beta2 activation and diabetes. Diabetes. 2002. 51:2709–2718.
19. Vetter R, Rehfeld U, Reissfelder C, Weiss W, Wagner KD, Günther J, Hammes A, Tschöpe C, Dillmann W, Paul M. Transgenic overexpression of the sarcoplasmic reticulum Ca2+ATPase improves reticular Ca2+ handling in normal and diabetic rat hearts. FASEB J. 2002. 16:1657–1659.
20. Privratsky JR, Wold LE, Sowers JR, Quinn MT, Ren J. AT1 blockade prevents glucose-induced cardiac dysfunction in ventricular myocytes: role of the AT1 receptor and NADPH oxidase. Hypertension. 2003. 42:206–212.
21. Du X, Matsumura T, Edelstein D, Rossetti L, Zsengellér Z, Szabó C, Brownlee M. Inhibition of GAPDH activity by poly (ADP-ribose) polymerase activates three major pathways of hyperglycemic damage in endothelial cells. J Clin Invest. 2003. 112:1049–1057.
22. Farhangkhoee H, Khan ZA, Mukherjee S, Cukiernik M, Barbin YP, Karmazyn M, Chakrabarti S. Heme oxygenase in diabetes-induced oxidative stress in the heart. J Mol Cell Cardiol. 2003. 35:1439–1448.
23. Nichols GA, Hillier TA, Erbey JR, Brown JB. Congestive heart failure in type 2 diabetes: prevalence, incidence, and risk factors. Diabetes Care. 2001. 24:1614–1619.
24. Bell DS. Diabetic cardiomyopathy. A unique entity or a complication of coronary artery disease? Diabetes Care. 1995. 18:708–714.
25. Okruhlicova L, Tribulova N, Weismann P, Sotnikova R. Ultrastructure and histochemistry of rat myocardial capillary endothelial cells in response to diabetes and hypertension. Cell Res. 2005. 15:532–538.
26. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, Kannel WB, Vasan RS. Obesity and the risk of heart failure. N Engl J Med. 2002. 347:305–313.
27. Taegtmeyer H, McNulty P, Young ME. Adaptation and maladaptation of the heart in diabetes: part I: general concepts. Circulation. 2002. 105:1727–1733.
28. He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001. 161:996–1002.
29. Wong CY, O'Moore-Sullivan T, Leano R, Byrne N, Beller E, Marwick TH. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation. 2004. 110:3081–3087.
30. Fox ER, Taylor J, Taylor H, Han H, Samdarshi T, Arnett D, Myerson M. Left ventricular geometric patterns in the Jackson cohort of the Atherosclerotic Risk in Communities (ARIC) Study: clinical correlates and influences on systolic and diastolic dysfunction. Am Heart J. 2007. 153:238–244.
31. Bajraktari G, Qirko S, Rexhepaj N, Bakalli A, Beqiri A, Elezi S, Ndrepepa G. Non-insulin dependent diabetes as an independent predictor of asymptomatic left ventricular diastolic dysfunction. Croat Med J. 2005. 46:225–231.
32. Di Bonito P, Cuomo S, Moio N, Sibilio G, Sabatini D, Quattrin S, Capaldo B. Diastolic dysfunction in patients with non-insulin-dependent diabetes mellitus of short duration. Diabet Med. 1996. 13:321–324.
33. Vanninen E, Mustonen J, Vainio P, Lansimies E, Uusitupa M. Left ventricular function and dimensions in newly diagnosed non-insulin-dependent diabetes mellitus. Am J Cardiol. 1992. 70:371–378.
34. Gough SC, Smyllie J, Barker M, Berkin KE, Rice PJ, Grant PJ. Diastolic dysfunction is not related to changes in glycaemic control over 6 months in type 2 (non-insulin-dependent) diabetes mellitus. A cross-sectional study. Acta Diabetol. 1995. 32:110–115.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download