Abstract
Background
Glycated hemoglobin (HbA1c) levels represent a 2~3 month average of blood glucose concentration. The use of HbA1c as a diagnostic tool for diabetes is gaining interest. Therefore, we determined the cutoff point of HbA1c for predicting abnormal glucose tolerance status in non-diabetic Korean subjects.
Methods
We analyzed the data from 1,482 subjects without diabetes mellitus in whom a 75-g oral glucose tolerance test (OGTT) was performed due to suspected abnormal glucose tolerance. We obtained an HbA1c cutoff point for predicting diabetes using Receiver Operating Characteristic (ROC) curve analysis.
Results
A cut-off point of 5.95% HbA1c yielded sensitivity of 60.8% and specificity of 85.6%, respectively, for predicting diabetes. There was a difference in HbA1c cut-off value between men and women, 5.85% and 6.05%, respectively.
Conclusion
To use the cut-off point of 5.95% HbA1c for predicting undiagnosed diabetes in Koreans may be reliable. However, studies of different ethnic groups have reported disparate HbA1c cut-off points. Thus, ethnicity, age, gender, and population prevalence of diabetes are important factors to consider in using elevated HbA1c value as a tool to diagnose diabetes.
Figures and Tables
Fig. 1
Receiver operating characteristic curves for HbA1c corresponding undiagnosed diabetes defined by ADA criteria.
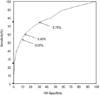
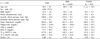
Table 3
Comparisons of mean value for HbA1c in groups divided by glucose metabolism in different gender groups

*P < 0.05 in post-hoc analyses with combined and diabetes groups except for female groups (significant differences only with diabetes group), †P < 0.05 in post-hoc analyses with all other groups, ‡Statistical significances were tested by one-way ANOVA test. As a post hoc analysis, Tukey's multiple comparison is performed. combined, IFG and IGT; HbA1c, glycated hemoglobin; I-IFG, isolated impaired fasting glucose; I-IGT, isolated impaired glucose tolerance.
Table 4
Comparison of sensitivity and specificity for predicting diabetes based on fasting glucose and 2 hour oral glucose tolerance test, at various levels of HbA1c

References
1. King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025. prevalence, numerical estimates, and projections. Diabetes Care. 1998. 21:1414–1431.
2. Saudek CD, Herman WH, Sacks DB, Bergenstal RM, Edelman D, Davidson MB. A new look at screening and diagnosing diabetes mellitus. J Clin Endocrinol Metab. 2008. 93:2447–2453.
3. Skyler JS, Bergenstal R, Bonow RO, Buse J, Deedwania P, Gale EA, Howard BV, Kirkman MS, Kosiborod M, Reaven P, Sherwin RS. Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a Scientific Statement of the American College of Cardiology Foundation and the American Heart Association. J Am Coll Cardiol. 2009. 53:298–304.
4. American Diabetes Association. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997. 20:1183–1197.
5. Bennett CM, Guo M, Dharmage SC. HbA1c as a screening tool for detection of type2 diabetes: a systematic review. Diabet Med. 2007. 24:333–343.
6. Petersen PH, Jorgensen LG, Brandslund I, De Fine Olivarius N, Stahl M. Consequences of bias and imprecision in measurements of glucose and Hba1c for the diagnosis and prognosis of diabetes mellitus. Scand J Clin Lab Invest Suppl. 2005. 240:51–60.
7. Sacks DB, Bruns DE, Goldstein DE, Maclaren NK, Mcdonald JM, Parrott M. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem. 2002. 48:436–472.
8. Consensus committee. Consensus statement on the worldwide standardization of the hemoglobin A1C measurement: the American Diabetes Association, European Association for the study of Diabetes, International Federation of Clinical Chemistry and Laboratory Medicine, and the International Diabetes Federation. Diabetes Care. 2007. 30:2399–2400.
9. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004. 27:suppl 1. S5–S10.
10. The Diabetes Control and Complication Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993. 329:977–986.
11. UK Prospective diabetes study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.
12. Standl PE. International diabetes federation european policy group standards for diabetes. Endocr Pract. 2002. 8:suppl 1. S37–S40.
13. Cobin RH, Davidson JA, Ganda OP, Garber AJ, Hellman R, Jellinger PS, Levetan CS, Palumbo PJ, Rodbard HW. American College of Endocrinology consensus statement on guidelines for glycemic control. Endocr Pract. 2002. 8:suppl 1. S5–S11.
14. Buell C, Kermah D, Davidson MB. Utility of A1C for diabetes screening in the 1999-2004 NHANES population. Diabetes Care. 2007. 30:2233–2235.
15. Nakagami T, Tominaga M, Nishimura R, Yoshiike N, Daimon M, Oizumi T, Tajima N. Is the measurement of glycated hemoglobin A1c alone an efficient screening test for undiagnosed diabetes? Japan National Diabetes Survey. Diabetes Res Clin Pract. 2007. 76:251–256.
16. Selvin E, Zhu H, Brancati FL. Elevated A1C in adults without a history of diabetes in the U.S. Diabetes Care. 2009. 32:828–833.
17. Kim SY, Park JH, Kang SM, Jin HY, Baek HS, Park TS. Value of HbA1c for diabetic screening in subject with normal fasting glucose. Korean Diabetes J. 2008. 32:suppl 2. S218.
18. Ku YH, Yoo SH, Jung HS, Lim S, Moon MK, Choi SH, Jang HC, Park KS, Kim SY, Lee HK, Cho YM. Diagnostic value of HbA1c different clinical setting with different prevelence of diabetes mellitus. Korean Diabetes J. 2008. 32:suppl 8. S311.
19. Kim KS, Kim SK, Lee YK, Park SW, Cho YW. Diagnostic value of glycated hemoglobin (HbA1c) for the early detection of diabetes in high risk subjects. Diabet Med. 2008. 25:997–1000.
20. Engelgau MM, Narayan KM, Herman WH. Screening for type 2 diabetes. Diabetes Care. 2000. 23:1563–1580.
21. International Expert Committee. International expert committee report on the role of the A1c assay in the diagnosis of diabetes. Diabetes Care. 2009. 32:1327–1334.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download