Abstract
Background
It is well known that renal TGFβ expression is related to the development of diabetic nephropathy. Alpha-lipoic acid (ALA), a potent antioxidant and cofactor of mitochondrial respiratory enzymes, can improve the insulin resistance and the vascular endothelial dysfunction, and suppresses the development of diabetic vascular complications. This study was undertaken to investigate whether ALA could reduce urinary protein excretion and renal TGFβ protein expression in obese type 2 diabetes mellitus animal model, Otsuka Long-Evans Tokushima Fatty (OLETF) rat.
Methods
Obese 30 male OLETF rats were randomly divided to 3 groups at the age of 30 weeks. The rats in the Control group fed normal rat chow while the rats in the ALA group were fed with rat chow containing ALA (0.5% of food weight). Ten rats in the Pair-fed group were fed with normal rat chow, but were given the same amount of food as consumed by the ALA group. During 5 weeks of ALA feeding, food intake and body weight were checked in metabolic chamber. Blood glucose levels, HbA1c and urinary protein excretion were measured at 30 weeks and 35 weeks of age, and renal TGFβ protein expression at 35 weeks of age was measured by Western blot and represented by relative unit (RU). Immunohistochemical staining for TGFβ protein in renal tissue was also examined at 35 weeks of age.
Results
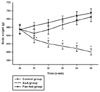
Food intake, body weight, blood glucose levels, HbA1c and urinary protein excretion among the Control, ALA and Pair-fed groups at 30 weeks of age were not different. At 35 weeks of age, food intake was significantly decreased in the ALA group than the Control group (Control group vs. ALA group, 27.7 ± 1.1 g/day vs. 22.4 ± 1.4 g/day, P < 0.001), and body weight was significantly decreased in the ALA group than the Control and Pair-fed groups (Control group: 694.4 ± 10.3 g, ALA group: 600.4 ± 7.4 g, Pair-fed group: 685.4 ± 11.6 g, P < 0.001). Blood glucose levels were significantly decreased in the ALA group than the Control and Pair-fed groups (Control group: 157.7 ± 4.6 mg/dL, ALA group: 130.7 ± 4.8 mg/dL, Pair-fed group: 153.7 ± 3.3 mg/dL, P < 0.001) although blood glucose levels from 30 weeks to 34 weeks of age and HbA1c at 35 weeks of age were not different among the groups. Urinary protein excretion and renal TGFβ protein expression were significantly decreased in the ALA group than the Control and Pair-fed groups (urinary protein excretion, Control group: 5.033 ± 0.254 mg/mgCr, ALA group: 3.633 ± 0.303 mg/mgCr, Pair-fed group: 4.977 ± 0.339 mg/mgCr, P < 0.001; renal TGFβ protein expression, Control group: 7.09 ± 0.17 RU, ALA group: 4.14 ± 0.26 RU, Pair-fed group: 7.00 ± 0.29 RU, P < 0.001). In the ALA group at 35 weeks of age, urinary protein excretion and renal TGFβ protein expression were positively related in the Control, ALA and Pair-fed groups (Control group, r = 0.847, P = 0.002; ALA group, r = 0.954, P < 0.001; Pair-fed group, r = 0.858, P = 0.002). TGFβ staining in glomeruli was observed in all groups but was decreased in the ALA group at 35 weeks of age.
Conclusion
These results suggest that ALA may prevent the increase of food intake, body weight, blood glucose, urinary protein excretion and renal TGFβ protein expression in obese type 2 diabetic rat model. The effect of ALA on diabetic nephropathy presented as proteinuria and renal TGFβ expression in diabetic patients needs to be further clarified.
Figures and Tables
 | Fig. 1The body weight was significantly decreased in the ALA group than the Control and Pair-fed groups after ALA (0.5% wt/wt) administration. *P < 0.001 vs. the Control and Pair-fed groups. |
 | Fig. 2The blood glucose levels were significantly decreased in the ALA group than the Control and Pair-fed groups at 35 week after ALA (0.5% wt/wt) administration. *P < 0.001 vs. the Control and Pair-fed groups. |
 | Fig. 3The renal TGFβ protein expression was significantly decreased in the ALA group than the Control and Pair-fed groups at 35 week after ALA (0.5% wt/wt) administration. RU, relative unit. *P < 0.001 vs. the Control and Pair-fed groups. |
 | Fig. 4The renal tissue at 35 weeks of age was stained with periodic acid Schiff (PAS). The glomerular hypertrophy and mesangial matrix expansion are shown in the Control (A), ALA (B) and Pair-fed groups (C) (H&E stain, ×400). |
 | Fig. 5The TGFβ immunostaining of glomeruli at 35 weeks of age is observed in all groups but decreases in the ALA group (brown color, ×400). Immunoperoxidase TGFβ, hematoxylin counterstaining. |
References
1. Raptis AE, Viberti G. Pathogenesis of diabetic nephropathy. Exp Clin Endocrinol Diab. 2001. 109:424–437.
4. Lee SH, Bae JS, Park SH, Lee BH, Park RW, Choi JY, Park JY, Ha SW, Kim YL, Kwon TH, Kim IS. Expression of TGFβ-induced matrix protein Big-h3 is up-regulated in the diabetic rat kidney and human proximal tubular epithelial cells treated with high glucose. Kidney Int. 2003. 64:1012–1021.
5. Mishra R, Emancipator SN, Kern T, Simonson MS. High glucose evokes an intrinsic proapoptotic signaling pathway in mesangial cells. Kidney Int. 2005. 67:82–93.
6. Border WA, Noble NA. Transforming growth factor in tissue fibrosis. N Eng J Med. 1994. 331:1286–1292.
7. Peters H, Noble NA, Border WA. Transforming growth factor β in human glomerular injury. Curr Opin Nephrol Hypertens. 1997. 6:389–393.
8. Fumo P, Kuncio GS, Ziyadeh FN. PKC and high glucose stimulate collagen alpha I(IV) transcriptional activity in reporter mesangial cell line. Am J Physiol. 1994. 267:632–638.
9. Ziyadeh FN. The extracellular matrix in diabetic nephropathy. Am J Kid Dis. 1993. 22:736–744.
10. Zhu M, Mizuno A, Noma Y, Murakami T, Kuwajima M, Shima K, Lan MS. Defective morphogenesis and functional maturation in fetal islet-like cell clusters from OLETF rat, a model of NIDDM. Int J Exp Diabetes Res. 2001. 1:289–298.
11. Sugimoto K, Tsuruoka S, Fujimura A. Effect of enalapril on diabetic nephropathy in OLETF rat: The role of anti-oxidative action in its protective properties. Clin Exp Pharmacol Physiol. 2001. 28:826–830.
12. Kanagawa K, Nakamura H, Murata I, Yosikawa I, Otsuki M. Increased gastric acid secretion in cholecystokinin-1 receptor deficient Otsuka Long-Evans Tokushima fatty rats. Scand J Gastroenterol. 2002. 37:9–16.
13. Reed L. Biochemistry of lipoic acid. Vitam Horm. 1962. 20:1–38.
14. Rudich A, Tirosh A, Potashnik R, Khamaisi M, Bashan N. Lipoic acid protects against oxidative stress induced impairment in insulin stimulation of protein kinase B and glucose transport in 3T3-L1 adipocytes. Diabetologia. 1999. 42:949–957.
15. Maddux BA, See W, Lawrence JC Jr, Goldfine AL, Goldfine ID, Evans JL. Protection against oxidative stress-induced insulin resistance in rat L6 muscle cells by micromolar concentrations of alpha-lipoic acid. Diabetes. 2001. 50:404–410.
16. Midaoui AE, de Champlain J. Prevention of hypertension, insulin resistance, and oxidative stress by alpha-lipoic acid. Hypertension. 2002. 39:303–307.
17. Jacob S, Ruus P, Hermann R, Tritschler HJ, Maerker E, Renn W, Augustin HJ, Dietze GJ, Rett K. Oral administration of RAC-alpha-lipoic acid modulates insulin sensitivity in patients with type-2 diabetes mellitus: a placebo-controlled pilot trial. Free Radic Biol Med. 1999. 27:309–314.
18. Song KH, Lee WJ, Koh JM, Kim HS, Youn JY, Park HS, Koh EH, Kim MS, Youn JH, Lee KU, Park JY. α-Lipoic acid prevents diabetes mellitus in diabetes-prone obese rats. Biochem Biophys Res Comm. 2005. 326:197–202.
21. Cameron NE, Cotter MA, Horrobin DH. Effect of alpha-lipoic acid on neurovascular function in diabetic rats: interaction with essential fatty acids. Diabetologia. 1998. 41:390–399.
22. Stevens MJ, Orosova I, Cao X. Effects of alpha-lipoic acid on peripheral nerve conduction, blood flow, energy metabolism and oxidative stress in experimental diabetic neuropathy. Diabetes. 2000. 49:1006–1015.
23. Packer L. Molecular aspects of lipoic acid in the prevention of diabetes complications. Nutrition. 2001. 17:888–895.
24. Kim MS, Park JY, Namkoong C, Jang PG, Ryu JW, Song HS, Yun JY, Nam-Goong IS, Ha J, Park IS, Lee IK, Viollet B, Youn JH, Lee HK, Lee KU. Anti-obesity effects of alpha-lipoic acid mediated by suppression of hypothalamic AMP-activated protein kinase. Nat Med. 2004. 10:727–733.
26. Melhem MF, Craven PA, Derubertis FR. Effects of dietary supplementation of α-lipoic acid on early glomerular injury in diabetes mellitus. J Am Soc Nephrol. 2001. 12:124–133.
27. Morcos M, Borcea V, Isermann B, Gehrke S, Ehret T, Henkels M, Schiekofer S, Hofmann M, Amiral J, Tritschler H, Ziegler R, Wahl P, Nawroth PP. Effect of α-lipoic acid on the progression of endothelial cell damage and albuminuria in patients with diabetes mellitus: an exploratory study. Diabetes Res Clin Pract. 2001. 52:175–183.
28. Cooper ME. Interaction of metabolic and haemodynamic factors in mediating experimental diabetic nephropathy. Diabetologia. 2001. 44:1957–1972.
29. van Det NF, Verhagen NA, Tamsma JT, Berden JH, Bruijn JA, Daha MR, van der Woude FJ. Regulation of glomerular epithelial cell production of fibronection and transforming growth factor beta by high glucose, not by angiotensin II. Diabetes. 1997. 46:834–840.
30. Sharma K, Ziyadeh FN. Biochemical events and cytokine interactions linking glucose metabolism to the development of diabetic nephropathy. Semin Nephrol. 1997. 17:80–92.
31. Aoyama I, Shimokata K, Niwa T. Oral adsorbent AST-120 ameliorates interstial fibrosis and transforming growth factor b1 expression in spontaneously diabetic (OLETF) rats. Am J Nephrol. 2000. 20:232–241.
32. Hida K, Wada J, Zhang H, Hiragushi K, Tsuchiyama Y, Shikata K, Makino H. Identification of genes specifically expressed in the accumulated visceral adipose tissue of OLETF rats. J Lipid Res. 2000. 41:1615–1622.
33. Sharma K, Ziyadeh FN. Renal hypertrophy is associated with upregulation of transforming growth factor beta I gene expression in diabetic BB rat and NOD mouse. Am J Physiol. 1994. 267:1094–1101.
34. Nakamura T, Fukui M, Ebihara I, Osada S, Nagooka I, Tomino Y, Koide H. mRNA expression of growth factor in glomeruli from diabetic rats. Diabetes. 1993. 42:450–456.
35. Sharma K, Jin Y, Guo J, Ziyadeh FN. Neutralization of transforming growth factor beta by anti TGFβ antibody attenuates kidney hypertrophy and the enhanced extracellular matrix gene expression in STZ-induced diabetic mice. Diabetes. 1996. 45:522–530.
36. Rumble JR, Cooper ME, Soulis T, Cox A, Wu L, Youssef S, Jasik M, Jerums G, Gilbert RE. Vascular hypertrophy in experimental diabetes: Role of advanced glycation end products. J Clin invest. 1997. 99:1016–1027.
37. Yagi K, Kim S, Wanibuchi H, Yamashita T, Yamamura Y, Iwao H. Characteristics of Diabetes, Blood Pressure and Cardiac and Renal Complications in Otsuka Long-Evans Tokushima Fatty Rats. Hypertens. 1997. 29:728–735.
38. Schiffer M, Bitzer M, Roberts IS, Kopp JB, ten Dijke P, Mundel P, Bottinger EP. Apoptosis in podocytes induced by TGFβ and Smad7. J Clin Invest. 2001. 108:807–816.
39. Schiffer M, Schiffer LE, Gupta A, Shaw AS, Roberts IS, Mundel P, Bottinger EP. Inhibitory smads and TGFβ signaling glomerular cells. J Am Soc Nephrol. 2002. 13:2657–2666.
40. Kim JH, Kim BK, Moon KC, Hong HK, Lee HS. Activation of the TGF-beta/Smad signaling pathway in focal segmental glomerulosclerosis. Kidney Int. 2003. 64:1715–1721.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download