Abstract
Background
The 26S ubiquitin-proteasome system (UPS) is a principal proteolytic pathway of intracellular molecules regulating apoptosis, cell cycle, cell proliferation or differentiation, inflammation and etc. The recent study suggests that the rs1048990 (C/G) polymorphism of the proteasome subunit α type 6 (PSMA6) gene is associated with the increase of the risk of myocardial infarction by the dysregulation of IκB degradation. We hypothesized that 26S UPS is important in the development of insulin resistance and type 2 diabetes (T2DM) by controlling the degradation of IκB and insulin receptor substances as a substrate. We therefore investigated whether the rs1048990 (C/G) polymorphism of PSMA6 gene and the rs2230087 (G/A) polymorphism of proteasome subunit β type 5 gene (PSMB5), that is chymotrypsin-like protease determining the rate of proteolysis, are associated with susceptibility to T2DM in Korean subjects.
Methods
We examined the polymorphisms of these genes in 309 diabetic subjects and 170 non-diabetic controls. The polymorphisms of rs1048990 (C/G) and rs2230087 (G/A) were genotyped by real-time PCR.
Results
The frequency of the G allele of rs1048990 (C/G) and the A allele of rs2230087 (G/A) polymorphisms was significantly higher in diabetic patients (28% and 13%) compared to that in controls (13% and 1%; P = 0.000 and P = 0.000, respectively). Logistic regression analysis of the rs1048990 (C/G) polymorphism showed that the odds ratio (OR) (adjusted for age, smoking, waist circumference, fasting plasma glucose, systolic blood pressure, HDL-C, triglyceride, and total cholesterol) was 3.93 (95% confidence interval [CI], 2.35-6.59; P = 0.000) for the G allele and 5.09 (95% CI, 2.71-9.57; P = 0.000) for CG and GG genotype when compared with the CC genotype. Logistic regression analysis of the rs2230087 (G/A) polymorphism showed that the adjusted OR was 5.70 (95% CI, 1.63-19.98; P = 0.007) for the A allele and 6.08 (95% CI, 1.66-22.29; P = 0.006) for GA and AA genotype when compared with the GG genotype. In multiple logistic regression analysis with T2DM as the independent Variable rs1048990 (C/G) and rs2230087 (G/A) polymorphisms were the predictor for T2DM.
Figures and Tables
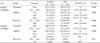
Table 1
Clinical and metabolic characteristics of study subjects

Values are presented as mean ± SD. BP, blood pressure; BMI, body mass index; FBS, fasting blood glucose; HBA1c glycosylated hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; s-Cr serum creatinine; T-chol, total cholesterol; TG, triglyceride; WHR waist-hip ratio.
Table 2
Genotype distribution of rs1048990 and rs2230087 polymorphisms in controls and diabetic patients

Table 3
Genotype distribution and allele frequency of rs1048990 and rs2230087 polymorphisms in controls and diabetic patients

Table 4
Age- and sex- adjusted or multivariate-adjusted ORs and 95% CIs of rs1048990 (A) and rs2230087 (B) polymorphisms in controls and diabetic patients

Table 6
Clinical and metabolic characteristics according to genotypes

Values are presented as mean ± SD. *P < 0.05. †P < 0.05, Significant even after adjustment for sex by binary logistic regression analysis. ‡Smoking: current or previous history of smoking. Other abbreviations see in Table 1.
References
2. Jiang Y, Beaudet AL. Human disorders of ubiquitination and proteasomal degradation. Curr Opin Pediatr. 2004. 16:419–426.

4. Ozaki K, Sato H, Iida A, Mizuno H, Nakamura T, Miyamoto Y, Takahashi A, Tsunoda T, Ikegawa S, Kamatani N, Hori M, Nakamura Y, Tanaka T. A functional SNP in PSMA6 confers risk of myocardial infarction in the Japanese population. Nat Genet. 2006. 38:921–925.

5. Yamamoto Y, Gaynor RB. IkappaB kinases: key regulators of the NFkappaB pathway. Trends Biochem Sci. 2004. 29:72–79.
6. Yuan M, Konstantopoulos N, Lee J, Hansen L, Li ZW, Karin M, Shoelson SE. Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of Ikkbeta. Science. 2001. 293:1673–1677.
7. White MF. The insulin signalling system and the IRS proteins. Diabetologia. 1997. 40:Suppl 2. S2–S17.

8. White MF. The IRS-signaling system: a network of docking proteins that mediate insulin and cytokine action. Recent Prog Hormone Res. 1998. 53:119–138.

9. Rome S, Meugnier E, Vidal H. The ubiquitin-proteasome pathway is a new partner for the control of insulin signaling. Curr Opin Clin Nutr Metab Care. 2004. 7:249–254.

10. Kisselev AF, Akopian TN, Castillo V, Goldberg AL. Proteasome active sites allosterically regulate each other, suggesting a cyclical bite-chew mechanism for protein breakdown. Mol Cell. 1999. 4:395–402.

11. Sjakste T, Kalis M, Poudziunas I, Pirags V, Lazdins M, Groop L, Sjakste N. Association of microsatellite polymorphisms of the human 14q13.2 region with type 2 diabetes mellitus in Latvian and Finnish populations. Ann Hum Genet. 2007. 71:772–776.

12. Lightcap ES, McCormack TA, Pien CS, Chau V, Adams J, Elliott PJ. Proteasome inhibition measurements: clinical application. Clin Chem. 2000. 46:673–683.

13. Hideshima T, Mitsiades C, Akiyama M, Hayashi T, Chauhan D, Richardson P, Schlossman R, Podar K, Munshi NC, Mitsiades N, Anderson KC. Molecular mechanisms mediating antimyeloma activity of proteasome inhibitor PS-341. Blood. 2003. 101:1530–1534.

14. Ha H, Yu MR, Choi YJ, Kitamura M, Lee HB. Role of high glucose-induced nuclear factor-B activation in monocyte chemoattractant protein-1 expression by mesangial cells. J Am Soc Nephrol. 2002. 13:894–902.

15. Bierhaus A, Schiefofer S, Schwaninger M, Andrassy M, Humpert PM, Chen J, Hong M, Luther T, Henle T, Kloting I, Morcos M, Hofmann M, Tritschler H, Weigle B, Kasper M, Smith M, Perry G, Schmidt AM, Stern DM, Haring HU, Schleicher E, Nawroth PP. Diabetes-associated sustained activation of the transcription factor nuclear factor-B. Diabetes. 2001. 50:2792–2808.

16. Emilo Ho, Tammy MT. Antioxidants, NF-kB activation and, diabetogenesis. Proc Soc Exp Biol Med. 1999. 222:205–213.
17. Karin M, Delhase M. The I kappa B kinase (IKK) and NF-kappa B: key elements of proinflammatory signalling. Semin Immunol. 2000. 12:85–98.
18. Sriwijitkamol A, Christ-Roberts C, Berria R, Eagan P, Pratipanawatr T, DeFronzo RA, Mandarino LJ, Musi N. Reduced skeletal muscle inhibitor of kappaB beta content is associated with insulin resistance in subjects with type 2 diabetes: reversal by exercise training. Diabetes. 2006. 55:760–767.
19. Araki E, Lipes MA, Patti ME, Brning JC, Haag B 3rd, Johnson RS, Kahn CR. Alternative pathway of insulin signalling in mice with targeted disruption of the IRS-1 gene. Nature. 1994. 372:186–190.

20. Brüning JC, Winnay J, Bonner-Weir S, Taylor SI, Accili D, Kahn CR. Development of a novel polygenic model of NIDDM in mice heterozygous for IR and IRS-1 null alleles. Cell. 1997. 88:561–572.

21. Tamemoto H, Kadowaki T, Tobe K, Yagi T, Sakura H, Hayakawa T, Terauchi Y, Ueki K, Kaburagi Y, Satoh S, Sekihara H, Yoshioka S, Horikoshi H, Furuta Y, Ikawa Y, Kasuga M, Yazaki Y, Aizawa S. Insulin resistance and growth retardation in mice lacking insulin receptor substrate-1. Nature. 1994. 372:182–186.

22. Withers DJ, Burks DJ, Towery HH, Altamuro SL, Flint CL, White MF. Irs-2 coordinates Igf-1 receptor -mediated beta-cell development and peripheral insulin signalling. Nat Genet. 1999. 23:32–40.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download