Abstract
Chronic obstructive pulmonary disease (COPD) is an ambulatory care-sensitive condition, and effective treatment of outpatients can prevent worsening of the illness and hospitalization. Current COPD guidelines provide appropriate guidance for the diagnosis and treatment of patients with COPD. In fact, it has been shown that when appropriate guidance and treatment are performed, the morbidity and mortality rates of COPD patients are reduced. However, there is a gap between the clinical guidelines and the actual clinical treatment. Therefore, the Health Insurance Review and Assessment Service (HIRA) conducted an evaluation of the adequacy of COPD diagnosis and treatment using the Claims Database of HIRA. This review provides a summary of the COPD adequacy assessment results reported by the HIRA and some brief comments on the results.
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory airway disease that causes irreversible airflow limitation. COPD is a common, preventable and treatable disease. However, according to the fourth Korean National Health and Nutrition Examination Survey conducted in Korea, the prevalence of COPD in subjects aged 40 years and older was 13.4% (males, 19.4%; female, 7.9%)1. However, only a minority of COPD patients receive physician's diagnosis or treatment not only in its early stages but even when lung function is severely impaired2. With its increasing prevalence, COPD is predicted to be the fourth most frequent cause of death worldwide by 2030 and the economic burden of COPD is also increasing3. So, the importance of early detection and intervention of COPD is emphasized4. Worsening of illness and hospitalization of COPD patients can be prevented when an outpatient is effectively treated with well controlled strategy. According to the Organisation for Economic Co-operation and Development (OECD) report, the COPD admission rate per 100,000 population over the age of 16 is 212.2 in Korea and the OECD average is 198.45. Although international variation in admission for COPD is 17-fold across OECD countries, Japan is 23.5 much lower than Korea. Current Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines provides appropriate guidance for the diagnosis and treatment of patients with COPD and, in fact, it has been shown to reduce the morbidity and mortality rate of COPD patients6. However, there is a gap between the clinical guidelines and the actual clinical care. In order to improve the quality of care for patients with COPD and to reduce the severity of illness and improve the adequacy of medical care benefits, the Health Insurance Review and Assessment Service (HIRA) conducted an evaluation of adequacy based on COPD claim data. The first assessment was based on the COPD claims data from May 14, 2014 to April 15, 2015 and the second assessment was based on the claims data from May 15, 2015 to April 16, 2016.
This article will review the second COPD assessment data of HIRA to identify the current status of COPD and make comments on the data.
We used the HIRA data from May 2015 to April 2016 to analyze the cost and utilization of COPD medication7. All hospitals, clinics, and public health centers with a claim for outpatient medical care as a major or primary codes of COPD were evaluated, except dental hospitals or clinics, oriental hospital or clinics and maternity centers. In Korea, private clinics are run by physicians and serve primary care. General practice is available but lab services are limited. Secondary hospitals are regional hospitals and highly differentiated with clinical specialties and bed size ranges 30 to 100. General hospitals provide more than nine specialties and more than 100 beds with specialized technical facilities. Tertiary hospitals are designated by the Minister of Health and Welfare every 3 years by score. Teaching is available and more than 20 specialties are available. There are 43 hospitals designated as tertiary hospitals in Korea from 2015 to 2017.
The patients included are diagnosed with COPD based on the International Classification of Disease, Tenth Revision (ICD-10) codes and medications prescribed. Inclusion criteria are as follows: (1) age ≥40 years; (2) ICD-10 codes for other COPD (J44.x) and emphysema (J43.x), with the exception of J43.0 (unilateral pulmonary emphysema, Macleod's syndrome); (3) the use of more than one of the following COPD medications at least twice per year; and (4) the use of oral or intravenous corticosteroid in admission and the use of COPD medications as outpatients. COPD medications are long-acting muscarinic antagonist (tiotropium, etc.), long-acting β2 agonist (LABA, indacaterol, etc.), inhaled corticosteroid+LABA, short-acting muscarinic antagonist (SAMA, ipratropium), short-acting β2 agonist (SABA, salbutamol, etc.), SAMA+SABA, phosphodiesterase-4 inhibitor (roflumilast), systemic beta agonist (bambuterol, etc.), or methylxanthine.
Total of 6,722 medical facilities, 142,790 patients and 733,165 prescriptions were evaluated (Table 1). Of the 142,790 patients, 66.84% of total patients were from tertiary and general hospitals, 28.03% were from private clinics. Seventy-two point seven five percent (103,882 patients) were male and more than two-thirds of the COPD patients (66.2%) were in their 60s and 70s.
Execution rate of pulmonary function test (PFT), the proportion of long-term out-patient visits, and the proportion of patients with COPD-related inhaler prescriptions are assessment tool which are considered the higher the better outcome (Table 2). Monitoring tools are admission rate due to COPD, emergency room (ER) visit related with COPD and the proportion of disease code with COPD or asthma among respiratory diseases.
Execution rate of PFT was defined as the percentage of COPD patients who underwent one or more PFTs during the assessment period. The execution rate of PFT was tertiary (82.30%), general hospitals (68.43%), secondary hospitals (52.35%), and private clinics (42.36%), respectively (Figure 1). The execution rate of males was 66.5% which was higher than female (51.94%). Sixty percent was in 50s to 70s but the percentage decreased as the age increased. Old patients in 90s showed the lowest execution rate (33.35%). Considering the execution rate of National Health Insurance Service (NHIS), there was no difference between National Health Insurance and Medical Aid. The execution rate of pulmonary function tests is still as low as 42.36% in private clinics. Except in the tertiary hospitals, the rate of PFT execution is less than 70%, more efforts to increase the rate of pulmonary function tests are needed.
The mean proportion of long-term out-patient visits was defined as more than 3 times visits at the same medical facility during the assessment period. The rate of continuous patients' visits was tertiary (91.45%), general hospitals (94.17%), secondary hospitals (93.47%), and private clinics (88.4%). The proportion of male was 92.9% which was higher than female (89.79%). The percentage was in positive correlation with the ages: 90s (93.88%), 80s (92.9%), 70s (92.67%), 60s (91.79%), 50s (90.59%), and 40s (87.62%). Considering the patients with NHIS type, health insurance proportion was 91.84% and Medical Aid was 94%. The average rate of long-term out-patients' visits exceeds the average of 90%, which means that existing COPD patients may continue to be well managed. It is possible to assume that the proportion of patients with persistent visits at tertiary hospitals is slightly lower because of the large number of out-patients.
The percentage of patients with inhaled bronchodilator prescriptions was defined as the percentage of COPD patients who were given inhaled bronchodilator during the evaluation period. The ratios were as follows: tertiary (92.61%), general hospitals (80.04%), secondary hospitals (60.41%), and private clinics (40.46%). As compared to the first evaluation results, the proportion of patients with inhaled bronchodilator prescription was mostly increased in private clinics (5.16%) and decreased in the nursing hospital (1.25%). In terms of gender, the male prescription of inhaled bronchodilator was 76.69%, which was higher than that of female 56.49%. Among the ages, the peak rate was 75.71% in 60s and the others are as follows: 50s>70s>40s>80s>90s. There was no difference between National Health Insurance and Medical Aid.
Bronchodilator is the cornerstone of the COPD treatment; considering the efficacy and side effects, inhaled form is the primary choice8. In 2015, the percentage of prescription of oral agents was 72.78% and inhaled form 71.80% (Table 3). Although the proportion of oral prescriptions was high, compared to the 2014 assessment by HIRA, oral medication decreased by 3.83% and inhalant medication increased by 3.19%. In private clinics, the prescription rate of inhaled bronchodilator was 40.06%, which was increased by 5.16% compared to the previous year. However, the need for improvement still exists; so more inhaler regimens should be made.
The average retention rate of PFT equipment is 64.31% in total, 100% in tertiary hospitals, 98.27% in general hospitals, 87.46% in secondary hospitals, and 62.26% in private clinics (Table 4). The total execution rate of PFT for the medical facilities which own PFT equipment was 67.41% and 26.81% for the facilities which do not own equipment. Especially, in the case of private clinics, the clinics which own PFT equipment did PFT in 51.25% of the patients and on the contrary the clinics which do not own PFT equipment did PFT in only 21.62% of the patients. The rate of prescription of total inhaled bronchodilator was 74.9% in case of medical facilities having PFT equipment and 24.46% not having PFT equipment, and the prescription rate showed a large variation (50.44%). In the case of private clinics, the rate of prescription of inhaled bronchodilator is 47.28% in clinics with PFT equipment, and the rate of prescription is 23.51% without PFT equipment. For the secondary hospitals, the prescription rate was 61.42% in the secondary hospitals which have PFT equipment and 45.18% in the secondary hospitals which did not have equipment. In the case of private clinics, it is necessary to raise the retention rate of equipment to increase the rate of performing pulmonary function test, the rate of continuous visit, and the rate of inhaler prescription.
The admission rate due to COPD was defined as more than one admission experience related to COPD during the assessment period. The patient ratio varied among the health care facilities: tertiary (13.87%), general hospitals (18.67%), secondary hospitals (23.04%), and private clinics (5.09%). The males' admission rate was higher (14.03) than females' (10.75%). As the age increases, the percentage of hospitalized patients became higher. By type of NHIS, patients with National Health Insurance was 12.43%, while those with Medical Aid was 18.40%. These results indicate that low-income COPD patients are relatively inadequately managed for COPD disease and thus have a high admission rate, and therefore, medical and economic policies are needed for low-income COPD patients to lower such admission rates.
The rate of ER visit related with COPD was defined as more than one ER visit due to COPD during the assessment period. The general hospital unit showed the highest rate (9.20%) and private clinics showed the lowest rate (2.39%). The tertiary hospitals and secondary hospitals showed 8.39% and 5.67%, respectively. The male patients visited ER more frequently than female with the rate of 6.93% versus 4.57%. By age, the 80s were the highest at 8.64% and the 40s were the lowest at 3.33%. Generally, as age increases, the rate of ER visits increased. In both genders, 80s–90s showed low PFT execution rate and bronchodilator prescription rate. By these results, admission and ER visit rates were high in old age COPD patients. By type of NHIS, 6.01% was with National Health Insurance and 8.36% was with Medical Aid.
The occupying rate was defined as the percentage of claim with COPD or asthma in the whole claim of respiratory disease during the assessment period. Among the total of 31.88 million claims of respiratory diseases in the evaluation period, 1.04 million claims (3.29%) were cases with COPD, 2.97 million claims (9.33%) were cases with asthma, and 290,000 claims with COPD and asthma (0.93%).
The main reason of this HIRA report is to evaluate the adequacy of COPD in order to improve the quality of patient care, to reduce the number of serious illnesses and to provide appropriate treatment. Since this HIRA report evaluated all medical institutions that treated patients with COPD in South Korea through the HIRA claims data, we can realize whether COPD patients are properly diagnosed with PFT equipment and prescribed appropriate inhaled bronchodilators in the real clinical field. Also, according to each medical facilities, the actual hospitalization rate and ER visit rate of COPD patients can be detected. These assessments will make us aware of the current diagnosis and treatment status and will be a good opportunity to diagnose and treat patients with COPD in the real world.
Figures and Tables
 | Figure 1Percentage of pulmonary function tests (PFTs) performed by medical institutions which have 10 more evaluated patients. |
Table 1
Characteristics of evaluated patients

Table 2
The important assessment parameters
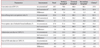
*Tertiary hospitals: teaching is available and more than 20 specialties are available. †General hospitals: more than nine specialties and more than 100 beds with specialized technical facilities are available. ‡Secondary hospitals: regional hospitals and highly differentiated with clinical specialties and bed size ranges 30 to 100. §Clinics: run by physicians and serve primary care. General practice is available but lab services are limited. ∥1st assessment: May 2014–April 2015. ¶2nd assessment: May 2015–April 2016.
Table 3
Prescription pattern of COPD in the first and second assessments

Table 4
Status of pulmonary function test equipment

Acknowledgments
We appreciate all the efforts of the Korea National Health and Nutrition Examination Survey of Korea Centers for Disease Control and Prevention (KCDC).
References
1. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011; 16:659–665.
2. Lee J, Lee JH, Kim JA, Rhee CK. Trend of cost and utilization of COPD medication in Korea. Int J Chron Obstruct Pulmon Dis. 2017; 12:27–33.
3. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006; 3:e442.
4. Lee JY, Rhee CK, Jung KS, Yoo KH. Strategies for management of the early chronic obstructive lung disease. Tuberc Respir Dis. 2016; 79:121–126.
5. Organisation for Economic Co-operation and Development. Health at a glance 2015: OECD indicators. Paris: OECD;2015.
6. Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017; 49:1700214.
7. Health Insurance Review & Assessment Service. Evaluation of appropriate management of COPD in Korea 2017 [Internet]. Wonju: Health Insurance Review & Assessment Service;2017. cited 2017 May 1. Available from: http://www.hira.or.kr/re/diag/getDiagEvlList.do?pgmid=HIRAA030004000000&WT.ac=%EB%B3%91%EC%9B%90%ED%8F%89%EA%B0%80.
8. Beeh KM. The role of bronchodilators in preventing exacerbations of chronic obstructive pulmonary disease. Tuberc Respir Dis. 2016; 79:241–247.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download