Abstract
Background
Fluoroquinolones are considered important substitutes for the treatment of tuberculosis. This study investigates the current status of fluoroquinolone for the treatment of tuberculosis.
Methods
In 2009, a retrospective analysis was performed at one tertiary referral center for 953 patients diagnosed with tuberculosis.
Results
A total of 226 patients (23.6%), who received fluoroquinolone at any time during treatment for tuberculosis, were enrolled in this study. The most common reasons for fluoroquinolone use were adverse events due to other anti-tuberculosis drugs (52.7%), drug resistance (23.5%), and underlying diseases (16.8%). Moxifloxacin (54.0%, 122/226) was the most commonly administered fluoroquinolone, followed by levofloxacin (36.3%, 82/226) and ofloxacin (9.7%, 22/226). The frequency of total adverse events from fluoroquinolone-containing anti-tuberculosis medication was 22.6%, whereas fluoroquinolone-related adverse events were estimated to be 2.2% (5/226). The most common fluoroquinolone-related adverse events were gastrointestinal problems (3.5%, 8/226). There were no significant differences in the treatment success rate between the fluoroquinolone and fluoroquinolone-naïve groups (78.3% vs. 78.4%, respectively).
Conclusion
At our institution, fluoroquinolones are commonly used for the treatment of both multidrug-resistant tuberculosis and susceptible tuberculosis, especially as a substitute for adverse event-related drugs. Considering the low adverse event rates and the comparable treatment success rates, fluoroquinolones seem to be an invaluable drug for the treatment of tuberculosis.
Tuberculosis (TB) is a contagious disease caused by Mycobacterium tuberculosis that continues to be a significant global problem. The recommended first-line regimen for the treatment of active TB consists of a combination of the following medications: isoniazid (INH), rifampin (RFP), pyrazinamide (PZA), and ethambutol (EMB)1. Although this first-line regimen has been shown to be very effective in treating TB, these medications are associated with significant adverse drug reactions234. In addition, the increasing worldwide prevalence of drug-resistant TB requires the use of alternative regimens.
The fluoroquinolones (FQNs) are a family of synthetic broad-spectrum antibacterial drugs. They have been shown to have good anti-mycobacterial activity and are considered important substitutes for the treatment of multidrug-resistant (MDR) TB (defined as resistance to at least INH and RFP)567. The FQNs have less side effects including hepatotoxicity than first-line drugs, and several studies reported that they are well tolerated in the presence of hepatic dysfunction891011121314. In transplant patients, RFP can reduce blood levels of calcineurin inhibitors because RFP is an inducer of the cytochrome P450 3A4 microsomal enzymes. Avoiding the drug-drug interaction, FQNs may be used instead of RFP15 and their long-term safety is also well established1416. Recently, because of the early sterilizing effect of FQNs in mice and humans1718, several studies have been conducted to reduce the duration of therapy by using FQN-based regimens1920212223.
These findings may lead to an increased use of FQNs for the treatment of TB2425. However, despite the increased experience in treating TB with FQNs, the exact characteristics of FQNs, such as drug types, reasons for use, and safety profiles, remain unclear. The aim of this study was to investigate the current status of FQNs use in the treatment of TB in one tertiary referral center in Korea.
The present study included 953 patients notified as TB cases from January 2009 to December 2009 at the Asan Medical Center, Seoul, Korea. TB was confirmed by mycobacterial culture or polymerase chain reaction (PCR), or was diagnosed clinically (histologically or through a therapeutic response to anti-TB therapy). In cases of culture proven TB, we performed drug susceptibility testing (DST). Once patients were diagnosed as active TB, basically they were treated with first-line regimen and then modified according to the result of DST or clinical response. Patients who experienced side event during their anti-TB treatment period, medications were adjusted by physician's decision. Demographic data including age, sex, comorbid conditions, previous history of TB, and drug susceptibility results were gathered retrospectively. All data were obtained from medical records, and survival status was obtained from hospital medical records and/or the records of National Health Insurance of Korea.
Patients who treated with FQN were included either temporary or permanent change during their treatment period. Variable factors related to FQN use were gathered, such as reasons for use, drug types, dosage, and FQN-related adverse events. Because patients were treated with other standard TB medications, the actual causality attributable to FQN may have been confounded. So, we defined adverse events as follows: total adverse events as any adverse event during FQN-containing therapy, possibly FQN-related adverse events as any adverse event that improved after withdrawal of FQN-containing regimen and did not retreated with FQN, and FQN-related adverse events as adverse events that estimated due to FQN by clinician. Treatment outcomes were also evaluated based on the definition recommended by the World Health Organization26.
Sputum specimens were examined microscopically with Ziehl-Neelsen staining, and cultured on both egg-based Ogawa medium and MGIT liquid medium. DST was performed at the Korean Institute of Tuberculosis, which is a Supranational TB Reference Laboratory. DST for INH, RFP, EMB, streptomycin, kanamycin, capreomycin, cycloserine, para-aminosalicylic acid, prothionamide, and ofloxacin was performed using the absolute concentration method with Lowëstein-Jensen media and PZA susceptibility was determined using the pyrazinamidase test.
Statistical analyses were performed with SPSS version 20.0 (IBM Corp., Armonk, NY, USA). A chi-square test or Fisher exact test was used for categorical data, and an unpaired Student's t test or Mann-Whitney test was used for continuous data. p-values less than 0.05 were considered statistically significant (two-tailed).
The mean patient age was 51.1±18.2 years, 519 patients (54.5%) were male and 142 patients (14.9%) had previous history of TB. A total of 619 patients (65.0%) were diagnosed with pulmonary TB and 334 patients (35.0%) were diagnosed with extrapulmonary TB. Among the 953 patients, TB was confirmed bacteriologically (culture or PCR-positive) in 567 (59.5%). Among the pulmonary TB patients, TB was confirmed bacteriologically in 76.7% (475/619, data not shown). Among the 567 patients with bacteriologically confirmed TB, DST results were available in 440 cases (77.6 %). Most of the patients were pan-susceptible, 37 (8.4%) had MDR-TB, and 15 (including 13 MDR-TB) were ofloxacin-resistant. Among the 953 TB patients, 226 (23.7%) received FQN at anytime during their anti-TB treatment period. Compared with the 727 non-FQN group, co-morbid conditions, such as liver disease, renal disease, and diabetes mellitus were more frequent in the FQN group. The proportions of MDR-TB, bacteriologically confirmed TB, and pulmonary TB were also more frequent in the FQN group. Other baseline characteristics were not different between the two groups. The demographic profile of the study patients is listed in Table 1.
Total of 226 patients received FQN during their anti-TB treatment period. Among them, 55 patients (24.3%) were treated with FQN temporarily, and 171 patients (75.7%) were treated with FQN-containing regimen during the rest of their treatment. The status of FQN use in our TB cohort is summarized in Table 2. Moxifloxacin (122 patients, 54.0%) was the most common FQN used, followed by levofloxacin (82 patients, 36.3%) and ofloxacin (22 patients, 9.7%). The most common reason for FQN use was the development of adverse events from administering other anti-TB medications (52.7%), followed by drug resistance (23.5%), and underlying medical conditions such as renal disease (9.7%) or liver disease (7.1%). The median duration of FQN use was 230 days (interquartile range, 79.5–287.0). Moxifloxacin dose was fixed at 400 mg/day. Among 82 levofloxacin users, high-dose levofloxacin (750 mg/day) was prescribed in about two-thirds of patients.
The most common reason for FQN use was adverse events of primary anti-TB medications. Types of adverse events of each standard medication are summarized in Table 3. Because two or more drugs were changed at the same time, most of adverse events of standard medication were unclassifiable to specific drug. Among them, hepatic toxicity and allergic reaction were common side effects. The most common drug which was substituted to FQN was EMB because of mostly eye problem. One patient complained insomnia which was improved after withdrawal of EMB. The second most common drug which was substituted to FQN was RFP, following PZA because of various problems, such as gastrointestinal problem, hepatic toxicity, and allergic reaction.
The second most common cause for FQN use was drug resistance. Resistant pattern is summarized in Table 4. Among 37 MDR-TB patients, 35 patients (94.6%) were treated with FQN. One patient was RFP mono-resistant TB and treated with FQN. Twenty-five patients were INH-resistant TB and 13 patients (52%) were treated with FQN. However, three MDR-TB patients and four INH-resistant TB patients were already treated with FQN due to adverse events of standard anti-TB medications before DST results come out.
Among the patients treated with FQN, DST results were available in 136 patients. As expected, the most frequent reason for FQN use was drug resistance in MDR-TB patients, except two patients who were transfer-out before DST results come out. The median duration of FQN use was significantly longer in MDR-TB patients than in non–MDR-TB patients (531 days vs. 188 days, respectively; p<0.05). Among non–MDR-TB patients, adverse drug reactions to other anti-TB drugs (64/101, 63.4%) were the most common reason for FQN use. Ofloxacin was prescribed only in patients with non–MDR-TB (Table 5).
Among 226 patients who were treated with FQN, 51 patients (22.6%) experienced adverse events from FQN-containing regimen (regardless of causality). The proportion of adverse drug reactions that were possibly due to FQN (did not retreated with FQN) was 9.3% and that were due to FQN was 2.2%. The most frequent adverse drug reaction was gastrointestinal problems for both total adverse events and possibly FQN-related adverse events (Table 6). The second most common adverse event was allergic reaction. Although hepatotoxicity or renal toxicity was the major reasons for FQN use, two patients experienced hepatotoxicity and one patient experienced renal toxicity due to possibly FQN. However, these patients improved after withdrawal of FQN without any management or hospitalization. On comparison of the two groups (moxifloxacin and levofloxacin), there were different incidence of adverse events (p=0.020). Gastrointestinal problems were the most common adverse event in the levofloxacin group, whereas allergic reaction was the most common adverse event in the moxifloxacin group. This trend was also found in cases of adverse events preferentially due to FQN, but with no statistical significance (p=0.140).
Median duration of FQN use in moxifloxacin group was 21 days until side effects occurred. Among 28 patients who experienced any adverse events from moxifloxain-containing regimen, 15 patients were stopped moxifloxacin and five patients were retreated with moxifloxacin after improved symptoms. The most common adverse event was allergic reaction in moxifloxacin group and median duration of moxifloxacin use was 19 days. Among 19 patients who experienced allergic reaction, five patients were stopped moxifloxacin permanently. In levofloxacin group, median duration of levofloxacin use was 36 days until side effects occurred. Among 21 patients who experienced any adverse events form levofloxacin-containing regimen, 14 patients were stopped levofloxacin and five patients were retreated with levofloxacin after improved adverse events. The most common adverse event was gastrointestinal problem in levofloxacin group and median duration of levofloxacin use was 44 days. Among eight patients with had gastrointestinal problem, six patients were stopped levofloxacin and only one patient was retreated with levofloxacin (Table 7).
Among 21 adverse cases which were possibly due to FQN, five cases were estimated due to FQN. One patient complained facial flushing after taking moxifloxacin, one patient complained chest tightness after taking ofloxacin, one patient experienced febrile sensation after taking levofloxacin, and two patients experienced arthralgia after taking levofloxacin. However, all of them were improved after withdrawal FQN.
The treatment success rate in the FQN group was 78.3% and was not different compared with that of the non-FQN group (78.4%) (Table 8). The relapse rate was also similar between the two groups (4.0% vs. 1.8%, respectively). The TB-related mortality of all subjects was very low (four patients, 0.4%) and similar between the two groups (data not shown). Among 136 patients who had DST results, the treatment success rate in MDR-TB patients was 80.0% and relapse did not occur within a median follow-up duration of 36 months (Table 9). Among INH-resistant group, about half of them (13/25) was treated with FQN during their anti-TB treatment period (nine patients for drug resistance, four patients for adverse events). The duration of treatment was longer in the patients treated with FQN (median, 315 days) compared with non-FQN group (median, 271 days), but with no statistical significance (p=0.167, data not shown). All patients were treated successfully regardless of FQN use, except one case which was transfer out. The treatment success rate was not different between FQN classes (p=0.993, data not shown). Among the FQN group, 14 patients had additional DST result (including seven relapse cases). Except one patient, all of them showed same DST results. Only one patient had changed DST result. He showed INH and EMB resistant TB initially. He was treated with levofloxacin-containing regimen for 9 months and relapsed after 5 months from end of treatment. Followed DST showed pre-extensively resistant tuberculosis pattern (resistant to INH, RFP, EMB, ofloxacin, levofloxacin, and moxifloxacin).
In this study, we showed the current status of FQN use in the treatment of TB in one tertiary referral center cohort in Korea. The frequency of FQN use was high in patients with TB, regardless of their drug-resistance status. Although FQNs are being used with increasing frequency, there have been no available data that what percentage of patients diagnosed with TB are treated with FQNs during their treatment period. Our study findings showed that the frequency of FQN use in TB patients was quite high, at about 23%. However, this percentage may depend on many factors, such as drug availability, cost, and concomitant medical conditions so that these data may not be representative of the general population in Korea. According to IMS Health data in Korea, FQNs accounted for about 10% of all antibiotics sales. Our hospital is a tertiary referral center that takes care of a high proportion of complicated cases. These findings may result in the high frequency of FQN use in TB patients.
It is well known that MDR-TB is a major reason for using FQNs26. However, our current results showed that the most common reason for FQN use was as a substitute drug to treat adverse events associated with standard TB medications (52.7%). There were not much data about the reason for prescribing FQNs to treating TB. In a study by Marra et al.10 about evaluating safety of levofloxacin-containing regimen, they showed that intolerance to standard anti-TB medication (82.0%) was the most common indication for prescribing levofloxacin. Other study by Codecasa et al.11 about evaluating tolerability of long-term moxifloxacin, they also showed that intolerance was major indication for using moxifloxacin. Although standard TB medications are highly effective in managing TB, they can lead to many adverse events, including hepatotoxicity and allergic reactions234. FQNs have less adverse reactions than first-line drugs and are therefore frequently used when patients have hepatic dysfunction or anti-TB drug induced hepatotoxicity8101112. The World Health Organization has recommended that patients with renal dysfunction need drug level monitoring of EMB while receiving the standard regimen. However, the EMB blood level monitoring was not setup yet in Korea, and many clinicians select FQNs instead of EMB in patients with chronic renal failure and concurrent TB. These factors are considered as a cause that the intolerance to standard TB medication was major reason for selecting FQNs as well as the resistance. However, further studies are needed to define the optimal FQN-containing combination regimen and the duration of the regimen for the treatment of TB.
In our present study, although the median duration of FQN use was quite long (275 days in the total patients group and 531 days in the MDR-TB patients group), its use was largely well tolerated. According to the findings of a study by Marra et al.10, the incidence of adverse events of the levofloxacin-containing regimen was 29% and the most common adverse events were gastrointestinal problems (56.7%). In earlier studies, it was also reported that moxifloxacin was well tolerable111627. Our present results showed that the risk of total adverse events was 22.6%, that the risk of possible FQN-related adverse events was 9.3% (21 patients), and that the risk of FQN-related adverse events was 2.2%. Moreover, all of our patients with possible FQN-related adverse events improved after withdrawal of FQN.
Faced with the increasing frequency of FQN use for other infection, a major concern in patients with newly diagnosed TB is the development of FQN-resistance282930. Despite the relatively high frequency of FQN use, FQN resistance had remained stationary at low levels for a long period of time in our hospital31. Although, we did not evaluate the history of previous FQN exposure, the rate of ofloxacin-resistance in our present cohort (15 patients, 3.4%) was similar to that of previous reports. Another important concern in patients treated with FQN-containing regimen is development of acquired FQN-resistance. In our present study, among 226 patients treated with FQN, one patient showed acquired FQN-resistance. Although, it is hard to say that FQN use is a risk factor of acquired FQN-resistance from our study results, caution still seems warranted in concerning about the development of FQN-resistance and delays in diagnosing TB.
The treatment success rate was about 80% in the FQN group, similar to that of the non-FQN group. Similarly, several studies reported that the treatment success was not different from that of the standard anti-TB regimen10. However, in our study, about half of patients receiving FQN had standard anti-TB medications before the administration of FQN because the major reason for FQN use was adverse events from previous anti-TB drugs. The antecedent standard anti-TB treatment might be improved the treatment outcome.
This study had several limitations. First, although it was performed in a large university-affiliated hospital, the results were not representative of the general population in Korea. However, this is the first report on the current status of FQN use for treatment of TB in Korea, which makes the results meaningful and relevant. Second, we limited the study period to just 2009. Therefore, the frequency of FQN use might be underestimated. Although extended study period-based studies are needed to confirm these findings, our study period was reasonable in terms of evaluating the efficacy and safety of long-term use of FQNs. Another limitation was its retrospective design. Actually, there were no exact policies about FQN use in TB patients. Therefore, using FQNs for treating TB such as decision on change of regimen, choice for different FQNs and treatment period with FQNs totally depends on physician's preference.
In conclusion, in Korea, a country with an intermediate burden of TB, FQNs have been frequently used as a substitute for adverse event-related drugs when treating TB, and also for the treatment of MDR-TB. Patients treated with FQNs show compatible treatment success rates without serious adverse events. Given these results, FQN is an invaluable drug for the treatment of TB and appears to be a promising and effective anti-TB drug.
Figures and Tables
Table 1
Clinical characteristics of 953 patients notified as tuberculosis in 2009

Table 2
Class of fluoroquinolones used for 226 patients with tuberculosis

Table 3
Types of adverse events during standard regimen requiring change to fluoroquinolones
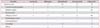
Table 4
Fluoroquinolone use according to the drug resistant pattern

Table 5
Clinical characteristics in 136 patients treated with fluoroquinolone according to the drug resistance pattern

Table 6
Adverse events after fluoroquinolone treatment of 226 tuberculosis patients

Table 7
Adverse events of moxifloxacin or levofloxacin containing regimen

Table 8
Treatment outcomes in 953 patients with tuberculosis

Table 9
Treatment outcomes in 136 tuberculosis patients treated with fluoroquinolone-containing regimens

Notes
Conflicts of Interest This study was supported by Daichi Sankyo Korea, a drug company that markets Cravit (levofloxacin). However, the study protocol was mainly designed by the principal investigator (Tae Sun Shim), and the first author (Bo Hyoung Kang), who performed the majority of the data analysis, did not know the support by Daichi Sankyo Korea. Therefore, there was no influence on conducting study, interpretation of results, and writing this article. All other authors report no competing interests.
References
1. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003; 167:603–662.
2. Steele MA, Burk RF, DesPrez RM. Toxic hepatitis with isoniazid and rifampin: a meta-analysis. Chest. 1991; 99:465–471.
3. Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003; 167:1472–1477.
4. Forget EJ, Menzies D. Adverse reactions to first-line antituberculosis drugs. Expert Opin Drug Saf. 2006; 5:231–249.
5. Jacobs MR. Fluoroquinolones as chemotherapeutics against mycobacterial infections. Curr Pharm Des. 2004; 10:3213–3220.
6. Migliori GB, Lange C, Girardi E, Centis R, Besozzi G, Kliiman K, et al. Fluoroquinolones: are they essential to treat multidrug-resistant tuberculosis? Eur Respir J. 2008; 31:904–905.
7. Falzon D, Jaramillo E, Schunemann HJ, Arentz M, Bauer M, Bayona J, et al. WHO guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Eur Respir J. 2011; 38:516–528.
8. Saigal S, Agarwal SR, Nandeesh HP, Sarin SK. Safety of an ofloxacin-based antitubercular regimen for the treatment of tuberculosis in patients with underlying chronic liver disease: a preliminary report. J Gastroenterol Hepatol. 2001; 16:1028–1032.
9. Yew WW, Chau CH, Wong PC, Lee J, Wong CF, Cheung SW, et al. Ciprofloxacin in the management of pulmonary tuberculosis in the face of hepatic dysfunction. Drugs Exp Clin Res. 1995; 21:79–83.
10. Marra F, Marra CA, Moadebi S, Shi P, Elwood RK, Stark G, et al. Levofloxacin treatment of active tuberculosis and the risk of adverse events. Chest. 2005; 128:1406–1413.
11. Codecasa LR, Ferrara G, Ferrarese M, Morandi MA, Penati V, Lacchini C, et al. Long-term moxifloxacin in complicated tuberculosis patients with adverse reactions or resistance to first line drugs. Respir Med. 2006; 100:1566–1572.
12. Roberts CH, Smith C, Breen R, Gadhok R, Murphy M, Aryee A, et al. Hepatotoxicity in the treatment of tuberculosis using moxifloxacin-containing regimens. Int J Tuberc Lung Dis. 2011; 15:1275–1276.
13. Carroll MW, Lee M, Cai Y, Hallahan CW, Shaw PA, Min JH, et al. Frequency of adverse reactions to first- and second-line anti-tuberculosis chemotherapy in a Korean cohort. Int J Tuberc Lung Dis. 2012; 16:961–966.
14. Fung SL, Yan SW, Chau CH, Yew WW. Tolerance of moxifloxacin-containing regimens in the treatment of tuberculosis. Int J Tuberc Lung Dis. 2012; 16:282–283.
15. Yoon HE, Jeon YJ, Chung HW, Shin SJ, Hwang HS, Lee SJ, et al. Safety and efficacy of a quinolone-based regimen for treatment of tuberculosis in renal transplant recipients. Transplant Proc. 2012; 44:730–733.
16. Pranger AD, van Altena R, Aarnoutse RE, van Soolingen D, Uges DR, Kosterink JG, et al. Evaluation of moxifloxacin for the treatment of tuberculosis: 3 years of experience. Eur Respir J. 2011; 38:888–894.
17. Klemens SP, Sharpe CA, Rogge MC, Cynamon MH. Activity of levofloxacin in a murine model of tuberculosis. Antimicrob Agents Chemother. 1994; 38:1476–1479.
18. Tortoli E, Dionisio D, Fabbri C. Evaluation of moxifloxacin activity in vitro against Mycobacterium tuberculosis, including resistant and multidrug-resistant strains. J Chemother. 2004; 16:334–336.
19. Conde MB, Efron A, Loredo C, De Souza GR, Graca NP, Cezar MC, et al. Moxifloxacin versus ethambutol in the initial treatment of tuberculosis: a double-blind, randomised, controlled phase II trial. Lancet. 2009; 373:1183–1189.
20. Rustomjee R, Lienhardt C, Kanyok T, Davies GR, Levin J, Mthiyane T, et al. A Phase II study of the sterilising activities of ofloxacin, gatifloxacin and moxifloxacin in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2008; 12:128–138.
21. Burman WJ, Goldberg S, Johnson JL, Muzanye G, Engle M, Mosher AW, et al. Moxifloxacin versus ethambutol in the first 2 months of treatment for pulmonary tuberculosis. Am J Respir Crit Care Med. 2006; 174:331–338.
22. Nuermberger EL, Yoshimatsu T, Tyagi S, Williams K, Rosenthal I, O'Brien RJ, et al. Moxifloxacin-containing regimens of reduced duration produce a stable cure in murine tuberculosis. Am J Respir Crit Care Med. 2004; 170:1131–1134.
23. Nuermberger EL, Yoshimatsu T, Tyagi S, O'Brien RJ, Vernon AN, Chaisson RE, et al. Moxifloxacin-containing regimen greatly reduces time to culture conversion in murine tuberculosis. Am J Respir Crit Care Med. 2004; 169:421–426.
24. Ginsburg AS, Grosset JH, Bishai WR. Fluoroquinolones, tuberculosis, and resistance. Lancet Infect Dis. 2003; 3:432–442.
25. Berning SE. The role of fluoroquinolones in tuberculosis today. Drugs. 2001; 61:9–18.
26. World Health Organization. WHO guidelines approved by the Guidelines Review Committee. Treatment of tuberculosis: guidelines. Geneva: World Health Organization;2010.
27. Valerio G, Bracciale P, Manisco V, Quitadamo M, Legari G, Bellanova S. Long-term tolerance and effectiveness of moxifloxacin therapy for tuberculosis: preliminary results. J Chemother. 2003; 15:66–70.
28. Ginsburg AS, Hooper N, Parrish N, Dooley KE, Dorman SE, Booth J, et al. Fluoroquinolone resistance in patients with newly diagnosed tuberculosis. Clin Infect Dis. 2003; 37:1448–1452.
29. Tsukamura M, Nakamura E, Yoshii S, Amano H. Therapeutic effect of a new antibacterial substance ofloxacin (DL8280) on pulmonary tuberculosis. Am Rev Respir Dis. 1985; 131:352–356.
30. Chen TC, Lu PL, Lin CY, Lin WR, Chen YH. Fluoroquinolones are associated with delayed treatment and resistance in tuberculosis: a systematic review and meta-analysis. Int J Infect Dis. 2011; 15:e211–e216.
31. Park IN, Hong SB, Oh YM, Lim CM, Lee SD, Lew WJ, et al. Impact of short-term exposure to fluoroquinolones on ofloxacin resistance in HIV-negative patients with tuberculosis. Int J Tuberc Lung Dis. 2007; 11:319–324.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download