Abstract
Lung cancer causes the most cancer deaths in Korea. Although the smoking rate has begun to decrease, the prevalence of lung cancer is still increasing. We reviewed the national lung cancer registry data and the data published about lung cancer in Korea. In 2012, the crude incidence rate of lung cancer was 43.9 per 100,000. The age-standardized mortality rate of lung cancer was 19.8 per 100,000. The 5-year relative survival rate for lung cancer was 11.3% from 1993 to 1995 and increased to 21.9% in the period from 2008 to 2012. Lung cancer occurring in never-smokers was estimated to increase in Korea. Adenocarcinoma is steadily increasing in both women and men and has replaced squamous cell carcinoma as the most common type of lung cancer in Korea. In patients with adenocarcinoma, the frequency of EGFR mutations was 43% (range, 20%–56%), while that of the EMK4-ALK gene was less than 5%.
Cancer has been the leading cause of death in Korea since 1983; and in 2013, it was the second leading cause of death after cardiovascular disease worldwide. Lung cancer is the most common cause of cancer death worldwide, both in developing and developed countries. In 2013, the estimated global lung cancer incidence was 1.8 million and the estimated number of fatal cases was 1.6 million1. The annual 2012 report of cancer statistics from the Korea Central Cancer Registry (KCCR) estimated that lung cancer was the most commonly diagnosed cancer among men >60 years old and women >70 years old2. Although the smoking rate in Korea recently began to decrease, the prevalence of lung cancer is still increasing and is expected to rise for the next 10–20 years3. This is due to the lag time between smoking exposure and its long-term consequences and because the Korean population aging (the fraction of the population ≥65 of age was 6.1% in 1996 and 12.7% in 2014)45.
Interest in lung cancer in patients without a smoking history has increased. Moreover, several reports found that the number of lung cancer in never-smokers is increasing67. Recently, a Korean study showed that among 5,456 cases with lung cancer in a community cancer center the proportion of never-smokers increased from 19.1% in 2004–2008 to 25.4% in 2009–20128. Lung cancer occurring in never-smokers (LCINS) is now regarded as a distinct disease entity; clinical and epidemiologic studies identified biologic and genetic differences between smoking-associated lung cancer and LCINS79. Never-smoker East Asian females have a tendency to develop adenocarcinoma, and these patients exhibit higher treatment response rates to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors10.
To estimate the lung cancer cases, including the pathologic type of cancer, data from the KCCR, a hospital-based nationwide cancer registry initiated by Korean Ministry of Health and Welfare in 1980, were used2. Lung cancer specific death data were acquired from Statistics Korea as were as population and smoking rate data11. In this review, we summarized current epidemiologic trends of lung cancer in Korea to provide background and contextual information about lung cancer that is important for management guidelines.
According to the KCCR, in 2012, 22,118 new lung cancer cases were diagnosed in Korea (men, 69.5%; women, 30.5%), accounting for 9.9% of all newly diagnosed cancer cases and ranked fourth by incidence2. The crude incidence rate was 43.9 per 100,000. The age-standardized lung cancer incidence rate age-adjusted to the Korean standard population (Korean age-standardized incidence rate, KASIR) was 27.9 per 100,000 in 2012 and the age-standardized lung cancer incidence rate adjusted to the world population (world age-standardized incidence rate, WASIR) was 27.4 per 100,0002. The cumulative incidence rate was 1.2% among patients 0 to 64 years of age and 3.4% among patients aged 0 to 74 years2. The third most commonly diagnosed cancer among Korean men was lung cancer. In men, the crude incidence rate was 61.0 per 100,000, whereas the KASIR was 45.0 per 100,000. In women, the crude incidence rate was 26.8 per 100,000, whereas the KASIR was 15.3 per 100,0002. Globally, occurrence of lung cancer between 0 and 79 years of age was higher in men than women (1 in 18 men and 1 in 51 women)1. In 2013, the global lung cancer WASIR in men was 45.17 per 100,000 and 16.15 per 100,000 in women1. The mean lung cancer KASIR in large cities or urban areas was lower than in local provinces or rural areas in Korea (27.9 vs. 29.5 per 100,000, p=0.039). This difference was more obvious in men (43.9 vs. 49.3 per 100,000, p<0.0001)2. The regional lung cancer KASIR of men was highest in Sejong City (51.4/100,000), and in North Gyeongsang (50.2/100,000) and South Gyeongsang Provinces (50.8/100,000). The regional lung cancer KASIR of women was highest in Ulsan (17.6/100,000), Daegu (17.5/100,000), and Jeju Province (17.4/100,000)2.
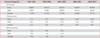
Table 1 shows Korean lung cancer incidence and prevalence rates by age in 20122. Both men and women 65–79 years old had the highest absolute incidence. Among men, the lung cancer KASIR was comparatively low before 49 years of age, then increased significantly with age, and reached its maximum at 80–84 years of age among men and in women over 85 years of age. The age-specific incidence rate of lung cancer was higher among men than in women, with the exception of those younger than 40 years. The 5-year prevalence was determined by surviving patients who had been diagnosed with lung cancer during the previous 5 years. The 5-year prevalence also increased markedly after 45 years of age and peaked in the 75–79 year age group2. Among new incident cases in 2012, stages were classified by Surveillance Epidemiology and End Results (SEER) program stage: localized only (invasive tumor confined to site of origin), regional extension (direct, ipsilateral lymph node[s] or both), and distant (site[s] or node[s])12. Distant metastasis stage cases comprised 41.1% of incident cases, regional extension cases comprised 25.8%, localized stage cases comprised 21.7% and unknown stage cases comprised 11.4%2.
Figure 1 shows trends of lung cancer incidence in Korea between 1999 and 2012. Overall crude incidences for both sexes increased (28.0/100,000 in 1993, 43.9/100,000 in 2012). However, overall KASIR showed plateau with smooth peaked in 2005 then slowly decreased (28.9/100,000 in 1993, 27.9/100,000 on 2012). The peak of the lung cancer epidemic related to tobacco has already passed among men in Korea as well as other developed nations and KASIRs are now decreasing (annual percentage change, –0.9%; p<0.05). In contrast, the KASIR for women has been rising slowly (annual percentage change, 1.7%; p<0.05).
Tracheal, bronchial, and lung (TBL) cancer is estimated to have a high incidence rate globally and in developing countries ranks as the second highest cancer incidence rate. In developed countries, on the other hands, it ranks third1. Between 1990 and 2013, the lung cancer WASIR for both sexes decreased by 6% (from 31.12/100,000 to 29.36/100,000), by 14% in developed countries (from 43.81/100,000 to 37.74/100,000) but increased by 9% in developing countries (from 23.04/100,000 to 25.18/100,000). TBL cancer is now ranked as the second most common cancer in men worldwide with a WASIR of 45.17 per 100,000 in 2013. It was the most common cancer in men in 1990 (WASIR, 50.80/100,000). Between 1990 and 2013, in developed countries, WASIR in men decreased by 26.36%, but in developing countries, it increased by 12.17%1. TBL cancer was the third most frequent cancer in women in 2013 (WASIR, 16.15/100,000). It had been the fifth most common in women in 1990 (WASIR, 15.36/100,000).
Figure 2 shows the temporal trends of lung cancer histologic types in Korea. Adenocarcinoma is steadily increasing among women as well as men and replaced squamous cell carcinoma as the most common type of lung cancer in Korea. This trend resembles those previously reported from developed countries (Europe, North America, and Japan) and recent trends in Asian countries, such as China131415. The emergence of adenocarcinoma predominance has become a worldwide lung cancer trend. This shift in lung cancer histologic type has been hypothesized to be caused by several factors13. First, the changes in cigarette compositions (lower tar and lower nicotine) and filter cause smokers to inhale deeper to be satisfied16, which allowed smoke to distribute more peripherally in the lung1317. Moreover, in cigarettes, polycyclic aromatic hydrocarbons, which is one of the squamous cell carcinogens, has decreased but N-nitrosamines, which might induce adenocarcinoma, increased1318. Another hypothesis is that adenocarcinoma requires a longer lag time to produce a tobacco related epidemiologic peak than does squamous cell carcinoma or small cell carcinoma. In the Nurses' Health Study (NHS) cohort in the United States, the risk of small cell and squamous cell carcinoma increased more rapidly with increasing smoking duration than did adenocarcinoma19. However, adenocarcinoma is more common in never-smokers. Especially in Asia, most female lung cancer patients are never-smokers and their histologic type is adenocarcinoma18. Moreover, cases of LCINS in Asia (Hong Kong, Singapore, Japan, and Korea) are diagnosed at an earlier age than cases of lung cancer in smokers1820. These findings have not been reproduced in European studies and never smoking patients with non-small cell lung cancer (NSCLC) in the United States were consistently older than ever-smoking patients1820. These findings suggest that other unidentified etiologic factors might be related to the development of LCINS.
In 2014, the age-standardized mortality rate (ASMR) of overall cancer in Korea was 155.3 per 100,000 for males and 69.1 per 100,000 for females. Cancer has been the leading cause of death in Korea since 1983. The proportion of deaths from cancer has steadily increased, accounting for 28.6% of the total deaths in 201411. Moreover, lung cancer was the most common cause of cancer death, based on absolute cases, globally as well as in developing and the developed regions1. In Korea, lung cancer has also been the leading cause of cancer death since 1999 and in 2014 was estimated to cause 17,440 deaths and account for 22.8% of all cancer deaths (crude mortality rate: both sexes, 34.4/105; men, 50.4/105; women, 18.3/105)1121. However, since 2002, the ASMR due to lung cancer has decreased slightly in both males and females in Korea21. The lung cancer ASMR in the Korean population was 23.3 per 100,000 in 2014 (men, 41.4/105; women, 10.5/105)11. Figure 3 shows the trends in annual lung cancer mortality rates in Korea. Lung cancer mortality among men reflects historical changes in cigarette smoking rates. In Korea, ASMRs differed significantly by region, the 5-year mean ASMR was higher in local provinces or rural areas than in large cities or urban areas (44.2/105 vs. 28.3/105, p<0.0001)11.
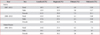
Age-standardized 5-year net survival from lung cancer was typically low, in the 10%–20% range, for most geographical areas, in both developed and developing countries22. In Korean men, lung cancer had the second worst 5-year survival rate after pancreatic cancer and among women, had the third worst rate after pancreatic cancer and liver cancer during 1993–20122. However, in the 1995–2009 global surveillance study of cancer survival, 5-year lung cancer survival in most nations had improved, up to 10%22. Table 2 shows an increasing trend for relative survival rate of lung cancer in Korea2. The overall 5-year relative survival rate for lung cancer during the period of 1993 to 1995 was 11.3% and increased to 21.9% during period of 2008 to 2012; in women survival improved more markedly (from 14.2% to 28.2%)221.
Stage at diagnosis accounts for the greatest variation in prognosis, but patients characteristics are also associated with poorer survival; these include being older, male gender, African American in the United States and low socioeconomic status23. Table 3 shows 5-year relative survival of lung cancer by SEER summary stage in Korea and the United Staes. Survival rates vary markedly by the stage at diagnosis224. Large multi-center, cooperative studies provide consistent evidence for a survival advantage in women25. The 2005 Korean Lung Cancer Registry Study also showed that sex is an independent risk factor for lung cancer prognosis (male; hazard ratio [HR], 1.37; 95% confidence interval [CI], 1.20–1.58; p<0.001)3. It was postulated that decreased DNA repair capacity in women might be responsible for the increased response rate and toxicity with platinum agents26. Lung cancer patients of Asian ethnicity survived longer than whites in several large epidemiologic studies27. A retrospective, population based analysis of NSCLC in US Koreans and Caucasians showed that Korean ethnicity is an independent favorable factor not only in the pre-epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI) era but also in the post–EGFR-TKI era (1998–2001; HR, 0.889; p=0.0013 and 2002–2005; HR, 0.795; p<0.0001)20. In another study, based on multivariate analyses, among 2,140 NSCLC patients within the United States, Asian American ethnicity was a favorable prognostic factor for overall survival (Asian American vs. non-Asian; HR, 0.861; 95% CI, 0.808–0.918; p<0.0001), among smokers (Asian American vs. non-Asian; HR, 0.867; 95% CI, 0.807–0.931; p<0.0001), and among never-smokers (Asian American vs. non-Asian; HR, 0.841; 95% CI, 0.728–0.971; p<0.0180)28. The reasons for the more favorable prognosis in Asians are incompletely understood, but one contributory factor is differences in tumor characteristics. For example, in Asians the prevalence of EGFR mutations in lung tumors is much higher than in whites23. Another explanation is population related pharmacogenomics. A study that analyzed results from three phase III trials suggested a 3- to 5-month overall survival improvement in Japanese NSCLC patients relative to US patients who received carboplatin and paclitaxel as first-line treatment. Differences in the allelic distribution of genes involved in paclitaxel disposition or DNA repair were observed29.
Smoking is the most important risk factor for lung cancer. In Korea, the prevalence of smoking in males has passed its peak. The age standardized smoking prevalence in Korean men was 63.4% in 1998 and steadily decreased to 38.1% by 2013. Among women, there were no obvious changes in smoking prevalence in the 21st century and it had plateaued at approximately 5%11. The age standardized lung cancer incidence and mortality rates among men declined after the mid-2000s and are starting to plateau for women; this may reflect previous trends in smoking prevalence2. In a prospective cohort study, among Korean men >40 years old, the relative risks of smokers, compared with nonsmokers, for the development of small cell, squamous cell lung carcinoma, and adenocarcinoma were estimated as 21.7-fold, 11.7-fold, and 2.1-fold, respectively30. A recent meta-analysis showed a relationship between smoking and lung cancer risk, clearly seen for ever smoking (relative risk, 5.50; 95% CI, 5.07–5.96), current smoking (relative risk, 8.43; 95% CI, 7.63–9.31), and ex-smoking (relative risk, 4.30; 95% CI, 3.93–4.71)31. Moreover, smoking status is well demonstrated to be one of the prognostic factors for advanced NSCLC32. Regarding specific histologic types, a retrospective clinical study from Japan showed that smoking increased mortality by a HR of 1.34 (95% CI, 1.15–1.55) in adenocarcinoma, but only by 0.99 (95% CI, 0.75–1.31) in nonadenocarcinoma33.
Recently, lung cancer in patients without a history of tobacco smoking has gained attention and the distinct entity, LCINS, has been introduced34. Many studies reported differences between smoking associated lung cancer and LCINS in clinical features and also in biological and genetic characteristics (LCINS was associated with Asian ethnicity, female gender and adenocarcinoma)34. This is especially relevant to developed Asian countries, such as Korea and Japan. The World Health Organization estimates that among lung cancer cases worldwide, 25% were never-smokers35. However, the proportion of LCINS cases varies widely and its temporal trend has not been well studied and is debated.7 In et al.3 showed that among 8,788 Korean patients (female, 24.2%) diagnosed in 2005, among the men, 87.3% were current or former smokers and among the women 79.7% had no history of smoking. In this current review, we could assume an increase of LCINS in Korea during the last decade based on the fact that crude lung cancer incidence among women is increasing steadily (1.8-fold during 1999–2012), whereas the smoking rate in women remains very low (5%) in Korea. The etiology of LCINS remains uncertain although several possible risk factors have been suggested, including environmental tobacco smoke (ETS), occupational carcinogens exposure, cooking fume exposure, oncogenic virus, pre-existing lung diseases, diet, and estrogen3436.
The relation between lung cancer and passive smoking has been well demonstrated. In a 1997 meta-analysis of passive smoking that categorized lifelong non-smokers according to whether the spouse currently smoked or had never smoked, Hackshaw et al.37 observed an odds ratio (OR) of 1.26 (95% CI, 1.07–1.47) and significant dose-response relationships between the lung cancer risk and both the quantity of cigarettes smoked by the partner and the exposure duration. In addition, Zhong et al.38 showed in their meta-analysis that the lung cancer relative risk of never-smoker women who were exposed to their husbands' smoking was 1.20 (95% CI, 1.12–1.29). However, the effect of second-hand smoking on the specific histological types has not been well studied and is debated34. Interestingly, in epidemiologic studies of whites with NSCLC in the United States and Europe, cases of LCINS have been consistently older than lung cancer patients with a smoking history3940. However, in studies conducted in Asian countries, including Korea, LCINS cases were younger at diagnosis. Toh et al.41 reported that in Singapore the mean age at diagnosis was 62 years in never-smokers (compared to ex-smokers, 72, and current smokers, 67). Kawaguchi et al.42 studied 4,954 Japanese patients with lung cancer and showed that younger patients (<59 years old) with lung cancer were more frequently never-smokers. In a retrospective comparative study of Korean and United States whites with NSCLC, Korean never-smokers were significantly younger than Korean ever-smokers (61 years vs. 63 years, p<0.0001), whereas white never-smokers were significantly older than white ever-smokers (75 years vs. 70 years, p<0.0001)20. The dose response relationship between ETS and lung cancer risk observed in studies of Western populations is biologically plausible; ETS requires more time to progress to cancer than direct smoking. However, the opposite results found in studies of Asian populations might suggest that carcinogenic etiologies and pathogenesis mechanisms of LCINS differ in Asians and whites35. Moreover, as mentioned in this review, the smoking rate among men has already decreased in the past 10 years, but the crude incidence of lung cancer in women is still increasing. This trend in women is not explained by second-hand smoke.
Globally, ambient air pollution is the most widespread environmental carcinogen. Exposure to fuel combustion for heating, cooking, power generation, motor vehicles and industrial processes is ubiquitous43. Several studies in Europe demonstrated that lung cancer risks were increased by exposure to certain atmospheric components by 1%–3.6% and were higher, by as much as 5%–7%, in never-smokers3544. In 2010, approximately 223,000 deaths from lung cancer worldwide were attributed to air pollution43. A recent Japanese prospective cohort study of 63,520 participant analyzed 10-year average concentrations of particulate matter less than 2.5 µm in aerodynamic diameter (PM2.5), SO2, and NO2. The hazard ratios for lung cancer mortality associated with a 10-unit increase in the above three exposures were 1.24, 1.26, and 1.17, respectively45. Hwang et al.46 demonstrated that long-term exposure to PM10 in Korean metropolitan cities was significantly associated with female lung cancer incidence; mortality and incidence were increased by 27% and 65%, respectively, at the highest PM10 category (>70 µg/m3) compared to the referent category (<50 µg/m3). A study that analyzed Korean medical insurance corporation and air quality data of the areas where lung cancer patients and controls lived showed that ozone and carbon monoxide increased the risk of lung cancer by 2.04 and 1.46, respectively47.
Combustion is a ubiquitous cause of environmental air toxin exposures and emissions of a wide range of species. In more developed countries, motor vehicle emissions play an important role in exposure to air pollution. In developing countries, household use of biomass and coal are a continuing source of concern, along with increasing exposures to automobile emissions as vehicle fleets increase43. Many studies have shown that women exposed to coal smoke have an elevated lung cancer risk in China. The results of a meta-analysis indicate that the relative risk for lung cancer from exposure to coal smoke in women over 30 years of age is 1.94 (95% CI, 1.09–3.47)48. The biomass primarily includes wood, animal waste (dung), leaves and grass. In a European multicenter study, Lissowska et al.49 demonstrated a 20%–30% adjusted increased risk of lung cancer among people who burned wood, but not coal, for cooking or heating compared with people who never used these fuels.
Cooking oil fume is another possible risk factor, as demonstrated in several studies in China where high temperature cooking using oil is combined with poor kitchen ventilation. Zhao et al.50, reported that exposure to cooking oil fumes conferred an increased risk for lung cancer (OR, 2.12; 95% CI, 1.81–2.47) in the women without a smoking history, based on a meta-analysis. In additions, a dose-response relationship between cooking fumes exposures and lung cancer was demonstrated among Chinese women who were nonsmokers51, and poor home kitchen ventilation was associated with an increased lung cancer risk in this Chinese study52.
Recent studies demonstrated that inflammation may play an important role in cancer pathogenesis5354. Pulmonary conditions, such as chronic bronchitis and emphysema, tuberculosis, and pneumonia, are the major causes of lung tissue inflammatory processes54. The pooled analysis from studies conducted in Europe and Canada showed that chronic bronchitis (in men; OR, 1.33) and emphysema (in men; OR, 1.50) were positively associated with lung cancer, after accounting for other respiratory diseases and smoking. Recent pneumonia (2 years or less before lung cancer) conferred a 3.31-fold risk for lung cancer for men. Tuberculosis diagnosed 2–4 years prior conferred an increase risk of lung cancer, an OR of 3.26 for men and an OR of 5.06 for women55. Recent evidence indicates that lung cancer occurred in approximately one in every 10 patients with idiopathic pulmonary fibrosis (IPF) with a prevalence ranging from 4.3% to 13% and that IPF alone is an independent risk factor for lung cancer56. Moreover, in Korea, Kwak et al.57 demonstrated that combined pulmonary fibrosis and emphysema conferred a higher risk than did emphysema alone (adjusted HR, 4.62; 95% CI, 1.58–13.55). We previously reported that squamous cell carcinomas are the most common histologic type in the setting of IPF in Korea and IPF was an independent poor prognostic factor for survival among surgically treated lung cancer patients58.
Recently, molecularly targeted therapies have improved treatment for patients whose tumors have somatic driver oncogenes, such as mutant EGFR or trans-located anaplastic lymphoma kinase (ALK), rearranged during transfection (RET), or ROS159. To select patients who will have an appropriate therapeutic response, molecular testing is a routine, clinically important tool60. In our previous study, EGFR gene mutations were identified in 29% of patients with non-squamous NSCLC by direct sequencing. EGFR mutations were significantly more frequent in non-smokers or light smokers than in heavy smokers (44.8% vs. 10.9%, p<0.001) and in females than in males (41.8% vs. 19.4%, p=0.007)61. Jang et al.62 also demonstrated that EGFR mutations were present in 24% (25/104) of patients with adenocarcinoma by direct sequencing. However, recent studies demonstrated that pyrosequencing and peptide nucleic acid clamping are more sensitive than direct sequencing for detecting EGFR mutations6364. Using these advanced technique, EGFR mutation among patients with pulmonary adenocarcinoma in Korea increased up to 51%–52%64. Interestingly, a single center study of EGFR mutations in Korean NSCLCs showed a 51.3% positive rate (196/382) by direct sequencing. In this study, the specimens tested were usually surgically resected samples (77%), which could provide sufficient tumor cell content65. A recent systematic, worldwide review of the frequency of EGFR mutation in patients with adenocarcinoma confirmed a higher mutation rate in Asia-Pacific countries (overall, 47%) than in Europe (15%), North America (22%), the Indian subcontinent (26%), and Oceania (12%). In most geographic regions, this mutation was higher in women compared with men and in never-smokers compared with ever-smokers60. Although this review could not consider sensitivity differences among testing methods, the Korean-specific overall EGFR frequency in patients with adenocarcinoma was 43% (1,248/2,884; range, 20%–56%) among 17 Korean studies60.
Echinoderm microtubule-associated protein-like 4 (EML4)-ALK fusion gene leads to expression of a chimeric tyrosine kinase, which has potent oncogenic activity. Lung cancer patients with this fusion gene had a dramatic favorable treatment response to ALK inhibitors (such as crizotinib)66. Several studies have reported that ALK-positive patients are younger, have never smoked and predominately have adenocarcinomas6667. The prevalence of ALK positive is approximately 4%–5% of all NSCLC patients in both Caucasian and Asian populations6869. Koivunen et al.70 observed a 3% positive rate of EMK4-ALK fusion gene among Korean (6/167) and Caucasian (2/136) patients, and all the positive patients had adenocarcinoma. Recent data from a single center in Korea showed that 10.4% (46/440) of patients with adenocarcinoma had the EML4-ALK fusion gene67. Novel fusions of the RET gene have been identified in 1%–2% of patients with NSCLC71. Yoo et al.72 showed that RET fusion genes occur in 1.9% (3/156) of surgically treated NSCLC patients in Korea.
Recently, genome-wide association studies have identified three chromosomal loci, 5p15, 6p21, and 15q25, as being associated with lung cancer risk in European and American populations73. Korean population based studies also confirmed the association between single nucleotide polymorphisms in the 5p15 and 15q25 chromosomal regions and lung cancer risk73. Ahn et al.74 demonstrated that the 18p11.22 region is a novel NSCLC susceptibility locus in Korean never-smokers.
Although the smoking rate has been declining for a decade, lung cancer prevalence is still increasing in Korea. The burden of lung cancer is expected to grow due to aging of the Korean population and the increasing incidence of lung cancer in never-smokers, especially among women. To reduce smoking rates and air pollution, more active interventions should be implemented. Further research is needed about the causes and carcinogenesis of lung cancer in never-smokers.
Figures and Tables
Figure 1
Trends in crude rates and age-standardized lung cancer incidence rates in the Korean population from 1999 to 2012. (A) Overall. (B) Men. (C) Women. Source: Annual report of cancer statistics in Korea in 2012 (Korea Central Cancer Registry, 2015)2.
Figure 2
Trends in histological type of lung cancer and age-standardized smoking rates in Korea. (A) Overall. (B) Men. (C) Women. Source: Annual report of cancer statistics in Korea in 2012 (Korea Central Cancer Registry, 2015)2; Korean Statistical Information Service (Statistics Korea, 2015)11.
Figure 3
Mortality trends for lung cancer in the Korean population. (A) Number of deaths. (B) Crude mortality rates. (C) Age-standardized mortality rates. Source: Korean Statistical Information Service (Statistics Korea, 2015)11.
Table 1
Number of lung cancer cases, incidence rates, and prevalence rates by age group in Korea in 2012
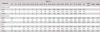
Source: Annual report of cancer statistics in Korea in 2012 (Korea Central Cancer Registry, 2015)2.
Crude rate: rate per 100,000 people; KASIR: age-standardized rate in the Korean population (1/105); WASIR: age-standardized rate in the world population (1/105); incidence case: number of cases; incidence rate: rate per 100,000 people; 5YPR: 5-year prevalence rate per 100,000 people.
Table 2
Trends in 5-year and 10-year relative survival (%) of lung cancer patients by sex and time period, 1993–2012
Source: Annual report of cancer statistics in Korea in 2012 (Korea Central Cancer Registry, 2015)2.
Table 3
Trends in 5-year relative survival (%) of lung cancer by Surveillance Epidemiology and End Results (SEER) stage in Korea and the United States
References
1. Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. The global burden of cancer 2013. JAMA Oncol. 2015; 1:505–527.
2. Korea Central Cancer Registry. Annual report of cancer statistics in Korea in 2012 [Internet]. Goyang: National Cancer Information Center;2015. cited 2015 Mar 31. Available from: http://www.cancer.go.kr/.
3. In KH, Kwon YS, Oh IJ, Kim KS, Jung MH, Lee KH, et al. Lung cancer patients who are asymptomatic at diagnosis show favorable prognosis: a Korean Lung Cancer Registry Study. Lung Cancer. 2009; 64:232–237.
4. Park JH, Lee KS, Choi KS. Burden of cancer in Korea during 2000-2020. Cancer Epidemiol. 2013; 37:353–359.
5. World DataBank. World development indicators [Internet]. Washington, DC: The World Bank Group;2015. cited 2015 Nov 11. Available from: http://databank.worldbank.org/ddp/home.dohttp://databank.worldbank.org/ddp/home.do.
6. Planchard D, Besse B. Lung cancer in never-smokers. Eur Respir J. 2015; 45:1214–1217.
7. Wakelee HA, Chang ET, Gomez SL, Keegan TH, Feskanich D, Clarke CA, et al. Lung cancer incidence in never smokers. J Clin Oncol. 2007; 25:472–478.
8. Kang H, Park CW, Kim W, Song SY, Na KJ, Jeong JU, et al. Never-smoker lung cancer is increasing. J Lung Cancer. 2012; 11:89–93.
9. Couraud S, Souquet PJ, Paris C, Do P, Doubre H, Pichon E, et al. BioCAST/IFCT-1002: epidemiological and molecular features of lung cancer in never-smokers. Eur Respir J. 2015; 45:1403–1414.
10. Ha SY, Choi SJ, Cho JH, Choi HJ, Lee J, Jung K, et al. Lung cancer in never-smoker Asian females is driven by oncogenic mutations, most often involving EGFR. Oncotarget. 2015; 6:5465–5474.
11. Korean Statistical Information Service. Statistics Korea [Internet]. Daejeon: Statistics Korea;2015. cited 2015 Sep 23. Available from: http://kosis.kr/.
12. Gloeckler Ries LA, Reichman ME, Lewis DR, Hankey BF, Edwards BK. Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program. Oncologist. 2003; 8:541–552.
13. Lortet-Tieulent J, Soerjomataram I, Ferlay J, Rutherford M, Weiderpass E, Bray F. International trends in lung cancer incidence by histological subtype: adenocarcinoma stabilizing in men but still increasing in women. Lung Cancer. 2014; 84:13–22.
14. Zhou C. Lung cancer molecular epidemiology in China: recent trends. Transl Lung Cancer Res. 2014; 3:270–279.
15. Toyoda Y, Nakayama T, Ioka A, Tsukuma H. Trends in lung cancer incidence by histological type in Osaka, Japan. Jpn J Clin Oncol. 2008; 38:534–539.
16. Gray N. The consequences of the unregulated cigarette. Tob Control. 2006; 15:405–408.
17. Marugame T, Sobue T, Nakayama T, Suzuki T, Kuniyoshi H, Sunagawa K, et al. Filter cigarette smoking and lung cancer risk: a hospital-based case: control study in Japan. Br J Cancer. 2004; 90:646–651.
18. Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and prevention. Clin Chest Med. 2011; 32:605–644.
19. Kenfield SA, Wei EK, Stampfer MJ, Rosner BA, Colditz GA. Comparison of aspects of smoking among the four histological types of lung cancer. Tob Control. 2008; 17:198–204.
20. Ahn MJ, Lee J, Park YH, Ahn JS, Ziogas A, Zell JA, et al. Korean ethnicity as compared with white ethnicity is an independent favorable prognostic factor for overall survival in non-small cell lung cancer before and after the oral epidermal growth factor receptor tyrosine kinase inhibitor era. J Thorac Oncol. 2010; 5:1185–1196.
21. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–141.
22. Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang XS, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015; 385:977–1010.
23. Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143:5 Suppl. e1S–e29S.
24. Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, et al. SEER cancer statistics review, 1975-2012. Bethesda: National Cancer Institute;2015.
25. Donington JS, Colson YL. Sex and gender differences in non-small cell lung cancer. Semin Thorac Cardiovasc Surg. 2011; 23:137–145.
26. Wang LE, Yin M, Dong Q, Stewart DJ, Merriman KW, Amos CI, et al. DNA repair capacity in peripheral lymphocytes predicts survival of patients with non-small-cell lung cancer treated with first-line platinum-based chemotherapy. J Clin Oncol. 2011; 29:4121–4128.
27. Soo RA, Loh M, Mok TS, Ou SH, Cho BC, Yeo WL, et al. Ethnic differences in survival outcome in patients with advanced stage non-small cell lung cancer: results of a meta-analysis of randomized controlled trials. J Thorac Oncol. 2011; 6:1030–1038.
28. Ou SH, Ziogas A, Zell JA. Asian ethnicity is a favorable prognostic factor for overall survival in non-small cell lung cancer (NSCLC) and is independent of smoking status. J Thorac Oncol. 2009; 4:1083–1093.
29. Gandara DR, Kawaguchi T, Crowley J, Moon J, Furuse K, Kawahara M, et al. Japanese-US common-arm analysis of paclitaxel plus carboplatin in advanced non-small-cell lung cancer: a model for assessing population-related pharmacogenomics. J Clin Oncol. 2009; 27:3540–3546.
30. Yun YH, Lim MK, Jung KW, Bae JM, Park SM, Shin SA, et al. Relative and absolute risks of cigarette smoking on major histologic types of lung cancer in Korean men. Cancer Epidemiol Biomarkers Prev. 2005; 14:2125–2130.
31. Lee PN, Forey BA, Coombs KJ. Systematic review with meta-analysis of the epidemiological evidence in the 1900s relating smoking to lung cancer. BMC Cancer. 2012; 12:385.
32. Janjigian YY, McDonnell K, Kris MG, Shen R, Sima CS, Bach PB, et al. Pack-years of cigarette smoking as a prognostic factor in patients with stage IIIB/IV nonsmall cell lung cancer. Cancer. 2010; 116:670–675.
33. Kogure Y, Ando M, Saka H, Chiba Y, Yamamoto N, Asami K, et al. Histology and smoking status predict survival of patients with advanced non-small-cell lung cancer. Results of West Japan Oncology Group (WJOG) Study 3906L. J Thorac Oncol. 2013; 8:753–758.
34. Yano T, Haro A, Shikada Y, Maruyama R, Maehara Y. Non-small cell lung cancer in never smokers as a representative 'non-smoking-associated lung cancer': epidemiology and clinical features. Int J Clin Oncol. 2011; 16:287–293.
35. Couraud S, Zalcman G, Milleron B, Morin F, Souquet PJ. Lung cancer in never smokers: a review. Eur J Cancer. 2012; 48:1299–1311.
36. Bae JM. Modifiable risk factors of lung cancer in neversmoker women. Epidemiol Health. 2015; Oct. 29. [Epub]. DOI: 10.4178/epih/e2015047.
37. Hackshaw AK, Law MR, Wald NJ. The accumulated evidence on lung cancer and environmental tobacco smoke. BMJ. 1997; 315:980–988.
38. Zhong L, Goldberg MS, Parent ME, Hanley JA. Exposure to environmental tobacco smoke and the risk of lung cancer: a meta-analysis. Lung Cancer. 2000; 27:3–18.
39. Nordquist LT, Simon GR, Cantor A, Alberts WM, Bepler G. Improved survival in never-smokers vs current smokers with primary adenocarcinoma of the lung. Chest. 2004; 126:347–351.
40. Quoix E, Monnet I, Scheid P, Hamadouche A, Chouaid C, Massard G, et al. Management and outcome of French elderly patients with lung cancer: an IFCT survey. Rev Mal Respir. 2010; 27:421–430.
41. Toh CK, Gao F, Lim WT, Leong SS, Fong KW, Yap SP, et al. Never-smokers with lung cancer: epidemiologic evidence of a distinct disease entity. J Clin Oncol. 2006; 24:2245–2251.
42. Kawaguchi T, Takada M, Kubo A, Matsumura A, Fukai S, Tamura A, et al. Gender, histology, and time of diagnosis are important factors for prognosis: analysis of 1499 never-smokers with advanced non-small cell lung cancer in Japan. J Thorac Oncol. 2010; 5:1011–1017.
43. Straif K, Cohen A, Samet J. Air pollution and cancer [Internet]. Lyon: International Agency for Research on Cancer;2013. cited 2015 Nov 11. Available from: http://www.iarc.fr/en/publications/books/sp161/AirPollutionandCancer161.pdf.
44. Gallus S, Negri E, Boffetta P, McLaughlin JK, Bosetti C, La Vecchia C. European studies on long-term exposure to ambient particulate matter and lung cancer. Eur J Cancer Prev. 2008; 17:191–194.
45. Katanoda K, Sobue T, Satoh H, Tajima K, Suzuki T, Nakatsuka H, et al. An association between long-term exposure to ambient air pollution and mortality from lung cancer and respiratory diseases in Japan. J Epidemiol. 2011; 21:132–143.
46. Hwang SS, Lee JH, Jung GW, Lim JH, Kwon HJ. Spatial analysis of air pollution and lung cancer incidence and mortality in 7 metropolitan cities in Korea. J Prev Med Public Health. 2007; 40:233–238.
47. Sung JH, Cho SH, Kang DH, Yoo KY. Lung cancer, chronic obstructive pulmonary disease and air pollution. Korean J Prev Med. 1997; 30:585–598.
48. Desai MA, Mehta S, Smith KR. Indoor smoke from solid fuels: assessing the environmental burden of disease at national and local levels [Internet]. Geneva: World Health Organization;2004. cited 2015 Nov 11. Available from: http://www.who.int/quantifying_ehimpacts/publications/en/Indoorsmoke.pdf.
49. Lissowska J, Bardin-Mikolajczak A, Fletcher T, Zaridze D, Szeszenia-Dabrowska N, Rudnai P, et al. Lung cancer and indoor pollution from heating and cooking with solid fuels: the IARC international multicentre case-control study in Eastern/Central Europe and the United Kingdom. Am J Epidemiol. 2005; 162:326–333.
50. Zhao Y, Wang S, Aunan K, Seip HM, Hao J. Air pollution and lung cancer risks in China: a meta-analysis. Sci Total Environ. 2006; 366:500–513.
51. Yu IT, Chiu YL, Au JS, Wong TW, Tang JL. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Res. 2006; 66:4961–4967.
52. Kim C, Gao YT, Xiang YB, Barone-Adesi F, Zhang Y, Hosgood HD, et al. Home kitchen ventilation, cooking fuels, and lung cancer risk in a prospective cohort of never smoking women in Shanghai, China. Int J Cancer. 2015; 136:632–638.
53. Peek RM Jr, Mohla S, DuBois RN. Inflammation in the genesis and perpetuation of cancer: summary and recommendations from a national cancer institute-sponsored meeting. Cancer Res. 2005; 65:8583–8586.
54. Brenner DR, Boffetta P, Duell EJ, Bickeboller H, Rosenberger A, McCormack V, et al. Previous lung diseases and lung cancer risk: a pooled analysis from the International Lung Cancer Consortium. Am J Epidemiol. 2012; 176:573–585.
55. Denholm R, Schuz J, Straif K, Stucker I, Jockel KH, Brenner DR, et al. Is previous respiratory disease a risk factor for lung cancer? Am J Respir Crit Care Med. 2014; 190:549–559.
56. Antoniou KM, Tomassetti S, Tsitoura E, Vancheri C. Idiopathic pulmonary fibrosis and lung cancer: a clinical and pathogenesis update. Curr Opin Pulm Med. 2015; 21:626–633.
57. Kwak N, Park CM, Lee J, Park YS, Lee SM, Yim JJ, et al. Lung cancer risk among patients with combined pulmonary fibrosis and emphysema. Respir Med. 2014; 108:524–530.
58. Lee T, Park JY, Lee HY, Cho YJ, Yoon HI, Lee JH, et al. Lung cancer in patients with idiopathic pulmonary fibrosis: clinical characteristics and impact on survival. Respir Med. 2014; 108:1549–1555.
59. Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014; 511:543–550.
60. Midha A, Dearden S, McCormack R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: a systematic review and global map by ethnicity (mutMapII). Am J Cancer Res. 2015; 5:2892–2911.
61. Park JY, Jang SH, Kim HJ, Park YB, Kwon JH, Song HH, et al. Predicting the treatment response using a direct sequencing method for EGFR in non-squamous, non-small cell lung cancer. Korean J Med. 2011; 81:611–622.
62. Jang TW, Oak CH, Chang HK, Suo SJ, Jung MH. EGFR and KRAS mutations in patients with adenocarcinoma of the lung. Korean J Intern Med. 2009; 24:48–54.
63. Kim HJ, Lee KY, Kim YC, Kim KS, Lee SY, Jang TW, et al. Detection and comparison of peptide nucleic acid-mediated real-time polymerase chain reaction clamping and direct gene sequencing for epidermal growth factor receptor mutations in patients with non-small cell lung cancer. Lung Cancer. 2012; 75:321–325.
64. Min KW, Kim WS, Jang SJ, Choi YD, Chang S, Jung SH, et al. Comparison of EGFR mutation detection between the tissue and cytology using direct sequencing, pyrosequencing and peptide nucleic acid clamping in lung adenocarcinoma: Korean multicentre study. QJM. 2016; 109:167–173.
65. Sun PL, Seol H, Lee HJ, Yoo SB, Kim H, Xu X, et al. High incidence of EGFR mutations in Korean men smokers with no intratumoral heterogeneity of lung adenocarcinomas: correlation with histologic subtypes, EGFR/TTF-1 expressions, and clinical features. J Thorac Oncol. 2012; 7:323–330.
66. Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009; 27:4247–4253.
67. Kang HJ, Lim HJ, Park JS, Cho YJ, Yoon HI, Chung JH, et al. Comparison of clinical characteristics between patients with ALK-positive and EGFR-positive lung adenocarcinoma. Respir Med. 2014; 108:388–394.
68. Chia PL, Mitchell P, Dobrovic A, John T. Prevalence and natural history of ALK positive non-small-cell lung cancer and the clinical impact of targeted therapy with ALK inhibitors. Clin Epidemiol. 2014; 6:423–432.
69. Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007; 448:561–566.
70. Koivunen JP, Mermel C, Zejnullahu K, Murphy C, Lifshits E, Holmes AJ, et al. EML4-ALK fusion gene and efficacy of an ALK kinase inhibitor in lung cancer. Clin Cancer Res. 2008; 14:4275–4283.
71. Gainor JF, Shaw AT. Novel targets in non-small cell lung cancer: ROS1 and RET fusions. Oncologist. 2013; 18:865–875.
72. Yoo SS, Jin G, Jung HJ, Hong MJ, Choi JE, Jeon HS, et al. RET fusion genes in Korean non-small cell lung cancer. J Korean Med Sci. 2013; 28:1555–1558.
73. Bae EY, Lee SY, Kang BK, Lee EJ, Choi YY, Kang HG, et al. Replication of results of genome-wide association studies on lung cancer susceptibility loci in a Korean population. Respirology. 2012; 17:699–706.
74. Ahn MJ, Won HH, Lee J, Lee ST, Sun JM, Park YH, et al. The 18p11.22 locus is associated with never smoker non-small cell lung cancer susceptibility in Korean populations. Hum Genet. 2012; 131:365–372.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download