Abstract
Background
Methods
Results
Figures and Tables
Table 1
Clinical characteristics of patients with scrub typhus, according to treatment with or without mechanical ventilation

Values are presented as mean±standard deviation or number (%).
*Student's t test. †p<0.05. ‡The total number of comorbidities may be more than 70, because the parameters are overlapped.
ICU: intensive care unit; COPD: chronic obstructive pulmonary disease; PF: the ratio of arterial oxygen partial pressure to fractional inspired oxygen; APACHE: Acute Physiology and Chronic Health Evaluation; SOFA: Sequential Organ Failure Assessment.
Table 2
Laboratory features of patients with scrub typhus, according to treatment with or without mechanical ventilation

Table 3
Factors associated with mechanical ventilation in patients with scrub typhus: results of univariate and multivariate logistic regression analysis
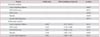
Table 4
Mean±standard deviation days in hospital, in intensive care unit, and on doxycycline therapy for patients with scrub typhus, according to treatment with or without mechanical ventilation

*p<0.05. Student's t test.
ICU: intensive care unit; Doxycycline therapyTotal: period of doxycycline therapy during hospitalization; Doxycycline therapyPre-ICU: period of doxycycline therapy before admitting to ICU; Doxycycline therapyPre-MV: period of doxycycline therapy before mechanical ventilation.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download