Abstract
Background
Methods
Results
Conclusion
Figures and Tables
Figure 1
(A, B) Subgroup analysis showed that overall survival (OS) was significantly longer in younger than in older patients with limited disease (LD) (p=0.003), but did not differ with age in extensive disease (ED) (p=0.279).

Figure 2
(A, B) Subgroup analysis showed that progression-free survival (PFS) was similar in all patients with limited disease (LD) (p=0.336) and extensive disease (ED) (p=0.727).

Table 1
Baseline characteristics

Values are presented as number (%).
*Using Fisher exact test.
LD: limited disease; ED: extensive disease; BMI: body mass index; ECOG PS: Eastern Cooperative Oncology Group performance status; PY: pack years; DM: diabetes mellitus; HF: heart failure: CRF: chronic renal failure; LC: liver cirrhosis; CVA: cerebrovascular disease; TB: tuberculosis; CTx: chemotherapy; EP: etoposide-cisplatin; EC: etoposide-carboplatin; RT: radiotherapy; CCRT: concurrent chemoradiotherapy; PCI: prophylactic cranial irradiation.
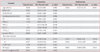
Table 2
Baseline characteristics (limited disease small cell lung cancer)

Values are presented as number (%).
*Using Fisher exact test.
BMI: body mass index; ECOG PS: Eastern Cooperative Oncology Group performance status; PY: pack years; DM: diabetes mellitus; HF: heart failure: CRF: chronic renal failure; LC: liver cirrhosis; CVA: cerebrovascular disease; TB: tuberculosis; CTx: chemotherapy; EP: etoposide-cisplatin; EC: etoposide-carboplatin; RT: radiotherapy; CCRT: concurrent chemoradiotherapy; PCI: prophylactic cranial irradiation.
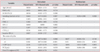
Table 3
Baseline characteristics (extensive disease small cell lung cancer)

*Using Fisher exact test.
BMI: body mass index; ECOG PS: Eastern Cooperative Oncology Group performance status; PY: pack years; DM: diabetes mellitus; HF: heart failure: CRF: chronic renal failure; LC: liver cirrhosis; CVA: cerebrovascular disease; TB: tuberculosis; CTx: chemotherapy; EP: etoposide-cisplatin; EC: etoposide-carboplatin; RT: radiotherapy; CCRT: concurrent chemoradiotherapy; PCI: prophylactic cranial irradiation.
Table 4
Univariate and multivariate analyses of factors associated with OS in patients with limited disease
OS: overall survival; BMI: body mass index; ECOG PS: Eastern Cooperative Oncology Group performance status; Ex: stop smoking now; PY: pack years; DM: diabetes mellitus; HF: heart failure; LC: liver cirrhosis; CVA: cerebrovascular disease; TB: tuberculosis; CCRT: concurrent chemoradiotherapy; PCI: prophylactic cranial irradiation; CTx: chemotherapy; EP: etoposide-carboplatin.
Table 5
Univariate and multivariate analyses of factors associated with PFS in patients with LD
progression-free survival; LD: limited disease; BMI: body mass index; ECOG PS: Eastern Cooperative Oncology Group performance status; Ex: stop smoking now; PY: pack years; DM: diabetes mellitus; HF: heart failure; LC: liver cirrhosis; CVA: cerebrovascular disease; TB: tuberculosis; CCRT: concurrent chemoradiotherapy; PCI: prophylactic cranial irradiation; CTx: chemotherapy; EP: etoposide-carboplatin.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download