Abstract
Cough is one of the most common symptom of many respiratory diseases. The Korean Academy of Tuberculosis and Respiratory Diseases organized cough guideline committee and cough guideline was developed by this committee. The purpose of this guideline is to help clinicians to diagnose correctly and treat efficiently patients with cough. In this article, we have stated recommendation and summary of Korean cough guideline. We also provided algorithm for acute, subacute, and chronic cough. For chronic cough, upper airway cough syndrome (UACS), cough variant asthma (CVA), and gastroesophageal reflux disease (GERD) should be considered. If UACS is suspicious, first generation anti-histamine and nasal decongestant can be used empirically. In CVA, inhaled corticosteroid is recommended in order to improve cough. In GERD, proton pump inhibitor is recommended in order to improve cough. Chronic bronchitis, bronchiectasis, bronchiolitis, lung cancer, aspiration, angiotensin converting enzyme inhibitor, habit, psychogenic cough, interstitial lung disease, environmental and occupational factor, tuberculosis, obstructive sleep apnea, peritoneal dialysis, and idiopathic cough can be also considered as cause of chronic cough. Level of evidence for treatment is mostly low. Thus, in this guideline, many recommendations are based on expert opinion. Further study regarding treatment for cough is mandatory.
Cough is one of the most common symptom of many respiratory diseases. Although cough guidelines from various countries are available, there has been no Korean cough guideline. The Korean Academy of Tuberculosis and Respiratory Diseases organized cough guideline committee at March 2013. From March 2013 to October 2014, cough guideline was developed by the members of this committee. The purpose of this guideline is to help clinicians to diagnose correctly and treat efficiently patients with cough. The content of this guideline is confined to adult patients only. This guideline is developed based on evidence. The committee developed key questions and searched evidence in three medical databases, Medline, Embase, Cochrane library and also in three Korean journals, Tuberculosis and Respiratory Diseases, Korean Journal of Medicine, and Allergy, Asthma & Respiratory Disease. The level of evidence was evaluated by the Grading of Recommendations Assessment, Development and Evaluation approach1. The strength of recommendation was assigned by formal voting rules from expert committee. The Korean cough guideline is written in Korean and published October 2014. In this article, we have stated recommendation and summary of Korean cough guideline.
- Beta-2 agonist should not be used to improved cough symptom (evidence, low; recommendation, strong).
- Considering adverse effect of antibiotics, empirical therapy of antibiotics can be considered only in patients with purulent sputum (evidence, high; recommendation, weak).
- Acute cough can be early symptom of serious diseases such as acute exacerbation of interstitial lung disease (ILD), congestive heart failure, tuberculosis (TB), endobronchial neoplasm, or foreign body aspiration. Thus, these diseases should be included in the differential diagnosis of acute cough (Figures 1, 2).
- Considering prevalence of TB in Korea, chest X-ray should be checked in patients with acute cough whose duration is more than 2 weeks.
- Chest X-ray can be checked in acute cough patients with old age, since symptoms of serious diseases may be non-specific in them.
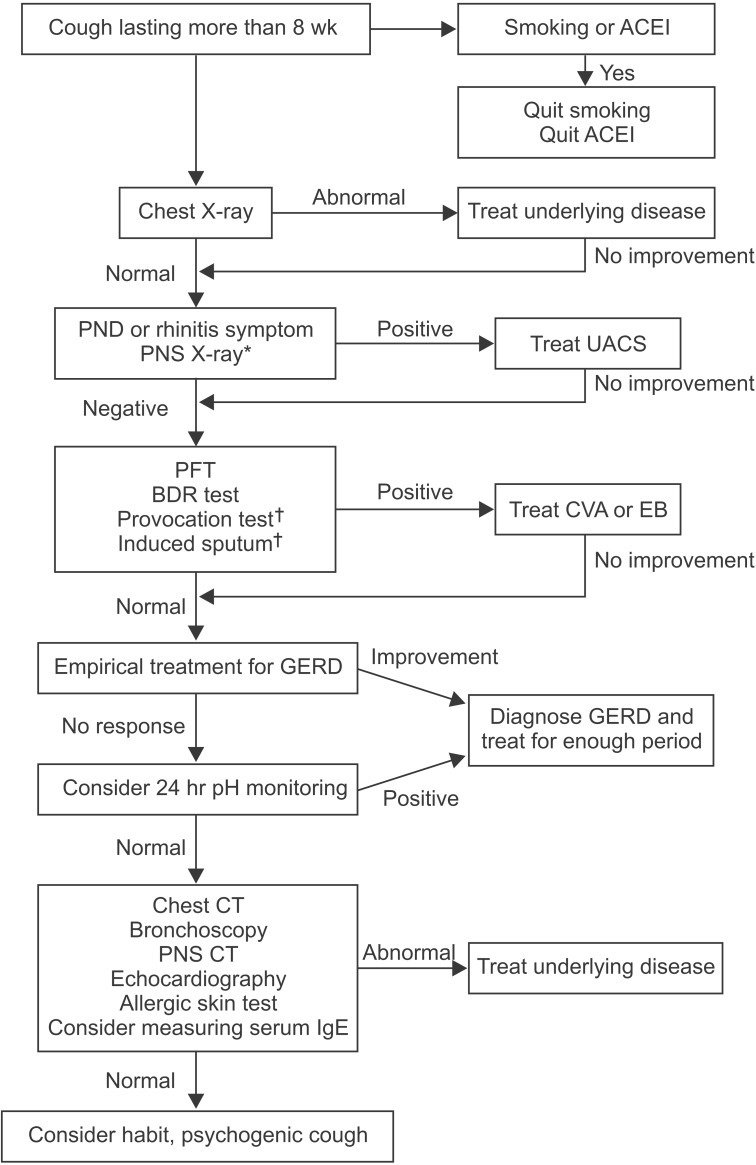
- Chronic cough is defined as a cough lasting more than 8 weeks.
- History including smoking, accompanying symptom, and medication is helpful for differential diagnosis and should be taken first and enough.
- Test for upper airway cough syndrome (UACS), cough variant asthma (CVA), and gastroesophageal reflux disease (GERD) should be performed (Figure 3).
- In UACS, intranasal steroid can be considered in order to improve cough (evidence, very low; recommendation, weak).
- In UACS, oral anti-histamine is recommended to improve cough (evidence, very low; recommendation, strong).
- In UACS, using nasal decongestant only is not recommended to improve cough (evidence, expert opinion; recommendation, strong).
- In UACS, intranasal anti-histamine is not considered to improve cough (evidence, very low; recommendation, weak).
- In UACS, antibiotics is not recommended to improve cough (evidence, expert opinion; recommendation, strong).
- UACS is syndrome of which various upper airway disease cause cough.
- UACS is diagnosed based on symptom, physical examination, radiologic finding, and response to empirical treatment.
- If UACS is diagnosed, adequate treatment should be initiated.
- If UACS is suspicious, first generation anti-histamine and nasal decongestant can be used empirically.
- In chronic bronchitis (CB) with normal lung function, smoking cessation is recommended in order to improve cough (evidence, expert opinion; recommendation, strong).
- In CB with normal lung function, mucoactive agent can be considered in order to improve cough (evidence, expert opinion; recommendation, weak).
- Treatment for CB with decreased lung function should follow chronic obstructive pulmonary disease guideline.
- CB is the most common cause of cough in smokers.
- Mucoactive agent is effective on improvement of cough in CB with decreased lung function22.
- When bronchiectasis is suspicious, high resolution computed tomography (HRCT) is needed even if chest X-ray is normal26.
- In diffuse panbronchiolitis, low-dose macrolide antibiotic is recommended in order to improve cough (evidence, expert opinion; recommendation, strong).
- Bronchiolitis should be preferentially considered when there are irreversible airflow obstruction, suspicion of small airway disease in HRCT, and purulent sputum in patients with cough31.
- Chest X-ray should be performed in case of risk factor for lung cancer or metastatic lung cancer.
- Bronchoscopy should be performed when suspicious of endobronchial invasion by tumor even if chest X-ray is normal32.
- In lung cancer, the reason of cough may not come from cancer. Thus, further evaluation is needed.
- In lung cancer, cough should be managed actively since it can affect quality of life and prognosis33.
- In lung cancer, stepwise treatment based on mechanism of drug should be considered in order to control cough34.
- Oropharyngeal dysphagia and aspiration should be checked in case of cough being developed when eating or swallowing food35.
- Habit, psychogenic cough is unconsciously persistent cough without underlying disease. It can be considered when there is no obvious reason for cough or cough does not respond to conventional therapy38.
- Habit, psychogenic cough is developed mostly during pediatrics and adolescent. When developed in adult, it may accompany with psychological problem3940.
- Habit, psychogenic cough is characterized by aggravation during emotional stress and social activity and disappearance during sleep.
- Habit, psychogenic cough can be diagnosed only if other causes are ruled out38.
- Environmental and occupational factors can evoke cough in itself, or can aggravate cough due to other causes. Thus, consideration for environmental and occupational factors is mandatory.
- Detailed history taking of exposure and occupation is important to find environmental and occupational factors.
- Narcotic central antitussive: morphine, codeine
- Nonopioid central antitussive: dextromethorphan, levopropoxyphene
- Peripheral antitussive: benzonatate, benproperine, theobromine
- Etc.: amitriptyline, baclofen, gabapentin
Mucoactive agent can be classified as expectorants, mucoregulatory agents, mucolytics, and mucokinetics5354
- Expectorants: hypertonic saline, iodinated glycerol, domiodol, guaifenesin, ion channel modifiers
- Mucoregulatory agents: carbocysteine, anticholinergics, glucocorticoid, macrolide antibiotics
- Mucolytics
- Mucokinetics: inhaled SABA, methylxanthine, surfactant, ambroxol, acebrophylline
References
1. Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A, et al. Going from evidence to recommendations. BMJ. 2008; 336:1049–1051. PMID: 18467413.

2. Madison JM, Irwin RS. Pharmacotherapy of chronic cough in adults. Expert Opin Pharmacother. 2003; 4:1039–1048. PMID: 12831332.

3. Gaffey MJ, Kaiser DL, Hayden FG. Ineffectiveness of oral terfenadine in natural colds: evidence against histamine as a mediator of common cold symptoms. Pediatr Infect Dis J. 1988; 7:223–228. PMID: 2895909.
4. Berkowitz RB, Connell JT, Dietz AJ, Greenstein SM, Tinkelman DG. The effectiveness of the nonsedating antihistamine loratadine plus pseudoephedrine in the symptomatic management of the common cold. Ann Allergy. 1989; 63:336–339. PMID: 2529799.
5. Gwaltney JM Jr, Phillips CD, Miller RD, Riker DK. Computed tomographic study of the common cold. N Engl J Med. 1994; 330:25–30. PMID: 8259141.

6. Puhakka T, Makela MJ, Alanen A, Kallio T, Korsoff L, Arstila P, et al. Sinusitis in the common cold. J Allergy Clin Immunol. 1998; 102:403–408. PMID: 9768580.

7. Pratter MR, Brightling CE, Boulet LP, Irwin RS. An empiric integrative approach to the management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129(1 Suppl):222S–231S. PMID: 16428715.
8. Asthma Workgroup of Chinese Society of Respiratory Diseases (CSRD). Chinese Medical Association. The Chinese national guidelines on diagnosis and management of cough (December 2010). Chin Med J (Engl). 2011; 124:3207–3219. PMID: 22088510.
9. McGarvey LP. Cough. 6: which investigations are most useful in the diagnosis of chronic cough? Thorax. 2004; 59:342–346. PMID: 15047960.
10. Morice AH, McGarvey L, Pavord I. British Thoracic Society Cough Guideline Group. Recommendations for the management of cough in adults. Thorax. 2006; 61(Suppl 1):i1–i24. PMID: 16936230.

11. Gibson PG, Dolovich J, Denburg J, Ramsdale EH, Hargreave FE. Chronic cough: eosinophilic bronchitis without asthma. Lancet. 1989; 1:1346–1348. PMID: 2567371.

12. Brightling CE, Ward R, Goh KL, Wardlaw AJ, Pavord ID. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999; 160:406–410. PMID: 10430705.

13. Richter JE, Castell DO. Drugs, foods, and other substances in the cause and treatment of reflux esophagitis. Med Clin North Am. 1981; 65:1223–1234. PMID: 7035766.

14. Vitale GC, Cheadle WG, Patel B, Sadek SA, Michel ME, Cuschieri A. The effect of alcohol on nocturnal gastroesophageal reflux. JAMA. 1987; 258:2077–2079. PMID: 3656623.

15. Clark CS, Kraus BB, Sinclair J, Castell DO. Gastroesophageal reflux induced by exercise in healthy volunteers. JAMA. 1989; 261:3599–3601. PMID: 2724505.

16. Fraser-Moodie CA, Norton B, Gornall C, Magnago S, Weale AR, Holmes GK. Weight loss has an independent beneficial effect on symptoms of gastro-oesophageal reflux in patients who are overweight. Scand J Gastroenterol. 1999; 34:337–340. PMID: 10365891.
17. Mathus-Vliegen LM, Tytgat GN. Twenty-four-hour pH measurements in morbid obesity: effects of massive overweight, weight loss and gastric distension. Eur J Gastroenterol Hepatol. 1996; 8:635–640. PMID: 8853250.
18. Bardin P, Kanniess F, Gauvreau G, Bredenbroker D, Rabe KF. Roflumilast for asthma: efficacy findings in mechanism of action studies. Pulm Pharmacol Ther. 2015; 8. 19. [Epub]. DOI: 10.1016/j.pupt.2015.08.006.

19. Stanciu C, Bennett JR. Effects of posture on gastro-oesophageal reflux. Digestion. 1977; 15:104–109. PMID: 14044.

20. Kanner RE, Connett JE, Williams DE, Buist AS. Effects of randomized assignment to a smoking cessation intervention and changes in smoking habits on respiratory symptoms in smokers with early chronic obstructive pulmonary disease: the Lung Health Study. Am J Med. 1999; 106:410–416. PMID: 10225243.

21. Wynder EL, Kaufman PL, Lesser RL. A short-term follow-up study on ex-cigarette smokers: with special emphasis on persistent cough and weight gain. Am Rev Respir Dis. 1967; 96:645–655. PMID: 6051202.
22. Cazzola M, Floriani I, Page CP. The therapeutic efficacy of erdosteine in the treatment of chronic obstructive bronchitis: a meta-analysis of individual patient data. Pulm Pharmacol Ther. 2010; 23:135–144. PMID: 19854285.

23. Klock LE, Miller TD, Morris AH, Watanabe S, Dickman M. A comparative study of atropine sulfate and isoproterenol hydrochloride in chronic bronchitis. Am Rev Respir Dis. 1975; 112:371–376. PMID: 1099948.
24. Ram FS, Jones PW, Castro AA, De Brito JA, Atallah AN, Lacasse Y, et al. Oral theophylline for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2002; (4):CD003902. PMID: 12519617.

25. Calverley P, Pauwels R, Vestbo J, Jones P, Pride N, Gulsvik A, et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003; 361:449–456. PMID: 12583942.

26. McGuinness G, Naidich DP. CT of airways disease and bronchiectasis. Radiol Clin North Am. 2002; 40:1–19. PMID: 11813813.

27. Wong C, Jayaram L, Karalus N, Eaton T, Tong C, Hockey H, et al. Azithromycin for prevention of exacerbations in noncystic fibrosis bronchiectasis (EMBRACE): a randomised, double-blind, placebo-controlled trial. Lancet. 2012; 380:660–667. PMID: 22901887.

28. Altenburg J, de Graaff CS, Stienstra Y, Sloos JH, van Haren EH, Koppers RJ, et al. Effect of azithromycin maintenance treatment on infectious exacerbations among patients with noncystic fibrosis bronchiectasis: the BAT randomized controlled trial. JAMA. 2013; 309:1251–1259. PMID: 23532241.
29. Serisier DJ, Martin ML, McGuckin MA, Lourie R, Chen AC, Brain B, et al. Effect of long-term, low-dose erythromycin on pulmonary exacerbations among patients with non-cystic fibrosis bronchiectasis: the BLESS randomized controlled trial. JAMA. 2013; 309:1260–1267. PMID: 23532242.
30. Evans DJ, Bara AI, Greenstone M. Prolonged antibiotics for purulent bronchiectasis in children and adults. Cochrane Database Syst Rev. 2007; (2):CD001392. PMID: 17443506.

31. Brown KK. Chronic cough due to nonbronchiectatic suppurative airway disease (bronchiolitis): ACCP evidence-based clinical practice guidelines. Chest. 2006; 129(1 Suppl):132S–137S. PMID: 16428702.
32. Shure D. Radiographically occult endobronchial obstruction in bronchogenic carcinoma. Am J Med. 1991; 91:19–22. PMID: 1858825.

33. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010; 363:733–742. PMID: 20818875.

34. Molassiotis A, Smith JA, Bennett MI, Blackhall F, Taylor D, Zavery B, et al. Clinical expert guidelines for the management of cough in lung cancer: report of a UK task group on cough. Cough. 2010; 6:9. PMID: 20925935.

35. Robbins J, Coyle J, Rosenbek J, Roecker E, Wood J. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999; 14:228–232. PMID: 10467048.

36. Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy: a review of the literature and pathophysiology. Ann Intern Med. 1992; 117:234–242. PMID: 1616218.
37. Lacourciere Y, Brunner H, Irwin R, Karlberg BE, Ramsay LE, Snavely DB, et al. Effects of modulators of the renin-angiotensin-aldosterone system on cough. Losartan Cough Study Group. J Hypertens. 1994; 12:1387–1393. PMID: 7706699.
38. Weinberger M. The habit cough syndrome and its variations. Lung. 2012; 190:45–53. PMID: 21842256.

39. Kravitz H, Gomberg RM, Burnstine RC, Hagler S, Korach A. Psychogenic cough tic in children and adolescents: nine case histories illustrate the need for re-evaluation of this common but frequently unrecognized problem. Clin Pediatr (Phila). 1969; 8:580–583. PMID: 5344422.
40. Gay M, Blager F, Bartsch K, Emery CF, Rosenstiel-Gross AK, Spears J. Psychogenic habit cough: review and case reports. J Clin Psychiatry. 1987; 48:483–486. PMID: 3320033.
41. Lavigne JV, Davis AT, Fauber R. Behavioral management of psychogenic cough: alternative to the "bedsheet" and other aversive techniques. Pediatrics. 1991; 87:532–537. PMID: 2011431.

43. Sundar KM, Daly SE, Pearce MJ, Alward WT. Chronic cough and obstructive sleep apnea in a community-based pulmonary practice. Cough. 2010; 6:2. PMID: 20398333.

44. Birring SS, Ing AJ, Chan K, Cossa G, Matos S, Morgan MD, et al. Obstructive sleep apnoea: a cause of chronic cough. Cough. 2007; 3:7. PMID: 17605822.

47. Min F, Tarlo SM, Bargman J, Poonai N, Richardson R, Oreopoulos D. Prevalence and causes of cough in chronic dialysis patients: a comparison between hemodialysis and peritoneal dialysis patients. Adv Perit Dial. 2000; 16:129–133. PMID: 11045277.
48. Twardowski ZJ, Khanna R, Nolph KD, Scalamogna A, Metzler MH, Schneider TW, et al. Intraabdominal pressures during natural activities in patients treated with continuous ambulatory peritoneal dialysis. Nephron. 1986; 44:129–135. PMID: 3774076.

49. Ekim M, Tumer N, Bakkaloglu S. Tuberculosis in children undergoing continuous ambulatory peritoneal dialysis. Pediatr Nephrol. 1999; 13:577–579. PMID: 10460504.

50. Pratter MR. Unexplained (idiopathic) cough: ACCP evidencebased clinical practice guidelines. Chest. 2006; 129:220S–221S. PMID: 16428714.
51. Gibson PG, Ryan NM. Cough pharmacotherapy: current and future status. Expert Opin Pharmacother. 2011; 12:1745–1755. PMID: 21524236.

52. Bolser DC. Mechanisms of action of central and peripheral antitussive drugs. Pulm Pharmacol. 1996; 9:357–364. PMID: 9232675.

53. Balsamo R, Lanata L, Egan CG. Mucoactive drugs. Eur Respir Rev. 2010; 19:127–133. PMID: 20956181.

54. Rubin BK. Mucolytics, expectorants, and mucokinetic medications. Respir Care. 2007; 52:859–865. PMID: 17594730.
Figure 1
Algorithm for evaluation of acute cough. *If symptom maintains, follow algorithm for subacute and chronic cough evaluation. †May consider empirical therapy when evaluation is not possible. PNS: paranasal sinus; PFT: pulmonary function test; BDR: bronchodilator response; CT: computed tomography.
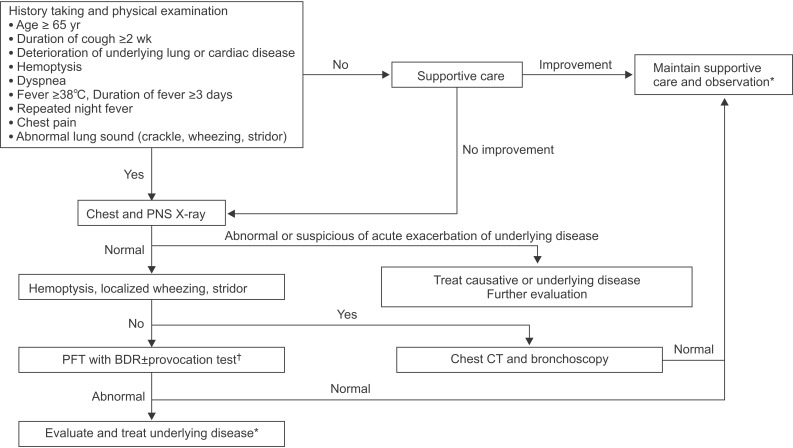
Figure 2
Algorithm for evaluation of subacute cough. *When clinical manifestations are suspicious of Bordetella pertussis or Mycoplasma infection, evaluation and treatment can be performed to these pathogens.
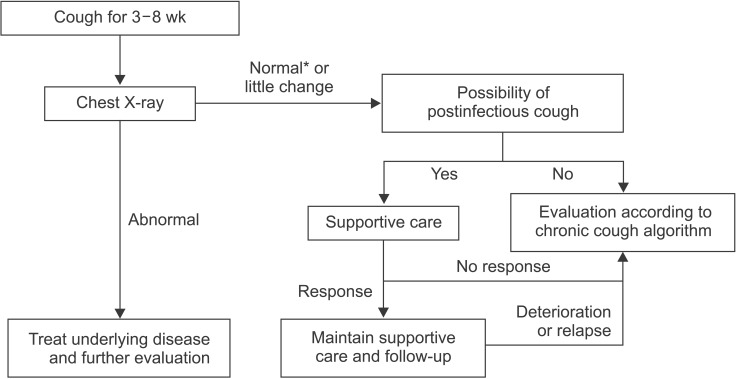
Figure 3
Algorithm for evaluation of chronic cough. *When clinical manifestation is suspicious for UACS, empirical treatment can be tried even if PNS X-ray is normal. †Empirical treatment can be considered when evaluation is not feasible. ACEI: angiotensin converting enzyme inhibitor; PND: postnasal drip; PNS: paranasal sinus; UACS: upper airway cough syndrome; PFT: pulmonary function test; BDR: bronchodilator response; CVA: cough variant asthma; EB: eosinophilic bronchitis; GERD: gastroesophageal reflux disease; CT: computed tomography.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download