Abstract
Cryptogenic organizing pneumonia (COP) is an inflammatory lung disease involving the distal bronchioles, respiratory bronchioles, bronchiolar ducts, and alveolae. The etiology is usually unknown; however, there are several known causes and associated systemic diseases. Corticosteroid therapy is the best treatment option and the prognosis of COP is good, with recovery in up to 80% of patients. We described a patient with in-operable hepatocellular carcinoma (HCC) undergoing chemoembolization with doxorubicin in a drug-eluting bead (DEB). COP developed in the patient after chemoembolization but resolved spontaneously in several months.
Cryptogenic organizing pneumonia (COP) is a syndrome of pulmonary inflammation with pathologic findings of growing granulation tissue in the bronchioles and alveolae. COP can be idiopathic or secondary to many different etiologies including infection, drugs, rheumatologic disease, myeloid disease and radiotherapy. Based on reported cases worldwide, the most common cause of COP is idiopathic1. It occurs equally in males and females. The clinical course is known to be diverse. According to a study of 45 COP patients in Korea, the disease was idiopathic in 35 patients, and secondary in 10 patients2. The average age of onset is 50 years, with a wide range of onset from 12 to 93 years old. Fifty percent to 70% of patients experience subacute respiratory distress over a period of 3-6 months. Fifty percent of patients suffer from fever and general myalgia and more than 80% of patients have end-inspiratory crackle on both lung fields. However, stridor, wheezing and hemoptysis are rare3. Observation is sufficient for cases with light clinical symptoms and mild pulmonary functional deterioration with minimum changes in radiology studies. However, when aggravated, corticosteroid therapy should be considered depending on the clinical course over several months. Even though the therapeutic response is high and, 80% of patients are generally cured successfully, some fail to recover with a mortality rate of 5%. In cases with low response to corticosteroid, immunosuppressives, such as cyclophosphamide and immunomodulating agents, such as macrolide, may be considered as a second line therapy3.
Transcatheter arterial embolization (TACE) is widely used for palliative treatment of hepatocellular carcinoma (HCC). Recently, a new treatment method called drug-eluting bead (DEB), which continuously releases doxorubicin when delivered in the hepatic artery, has been employed.
Despite various reported cases of drug induced COP, there has only been one case of COP induced by doxorubicin migration though a hepatic artery shunt after TACE4. That case was not in Korea. We report the first case of a patient in Korea who developed COP after TACE.
A 75-year-old visited our hospital on February 14, 2014 for dyspnea and dry cough, which had developed over the last 3 weeks. In his past medical history, he had visited our hospital with dyspepsia in November 7, 2013 and was diagnosed with hepatic cellular carcinoma. His abdominal scan revealed a 13 cm mass in the central portion and another mass in the fourth segment of the liver. Two courses of TACE with DEB were employed for the treatment of HCC in November and December of 2013. In January of 2014, a follow-up abdominal computed tomography (CT) was performed and emphysema was found in both lower lungs.
On admission, he had a blood pressure of 113/78 mm Hg, pulse rate of 98 beats per minute, respiratory rate of 18 breaths per minute, and body temperature of 36.6℃. He suffered from severe respiratory distress and a dry cough. Crackles on both lung fields observed on auscultation. An abdominal exam showed no significant abnormality. The laboratory test showed the following: white blood cell count, 8,400/mm3 (neutrophil segment, 77.6%); hemoglobin, 12.0 g/dL; platelet count, 137,000/mm3, erythrocyte sedimentation rate, 83 mm/hr; and C-reactive protein, 22.62 mg/dL. Arterial blood gas analysis on room air yielded the following results: pH, 7.43; partial pressure of oxygen (PaO2), 74.5 mm Hg; partial pressure of carbon dioxide (PaCO2), 35.6 mm Hg; and bicarbonate, 23.3 mEq/L. Other parameters are as follows: total protein, 6.9 g/dL; albumin, 3.1 g/dL; aspartate aminotransferase, 53 IU/L, aspartate transaminase, 25 IU/L, total bilirubin 1.22 mg/dL; lactic dehydrogenase, 443 IU/L; activated partial thromboplastin time, 45.8 seconds; and prothrombin time, 15.1 seconds (international normalized ratio, 1.19).
No significant abnormality was found in his sputum smear, sputum and blood culture. A chest CT scan on admission showed an abnormality of ground glass opacity and fibrosis with mild pleuritic effusion (Figure 1B). A pulmonary function test confirmed the presence of severe restrictive lung defects and gas exchange impairment. Forced vital capacity (FVC) was 1.66 L (40% of predictive normal value), forced expiratory volume in 1 second (FEV1) was 1.61 L (56% of predictive normal value), FEV1/FVC was 97%, and diffusing capacity for carbon monoxide was 8.1 mL/mm Hg/min (41% predictive normal value). Analysis of bronchoalveolar lavage (BAL) fluid resulted in the following: cell count 8×103/mL with 6% of neutrophil, 3% of lymphocyte, 87% of histiocyte, and 4% of mesothelial cell. A lymphocyte subset analysis of BAL fluid conducted using flow cytometry revealed 84% T cells, 42.3% CD4+ cells, 43.8% CD8+ cells, a CD4/CD8 ratio of 0.97.
Despite the administration of empirical antibiotics for 13 days to address the possibility of infectious, the lung lesions on chest X-ray became aggravated. On the fourth hospital day, a bronchoscopy was performed and only fibrotic stenosis was found on the superior segment of the right lower lobe. An acid-fast bacillis smear as well as bacterial and fungal culture from a bronchial washing specimen showed negative results. On the eighth day, a wedge lung resection with a thoracoscopy was performed for the purpose of diagnosis. The pathology was compatible with organizing pneumonia with intraluminal organizing fibrosis in distal airspaces (alveolar ducts, bronchiloles). However, there were no granulomas, necrosis, or vasculitis found (Figure 2).
The symptoms were alleviated by 14th day and the patient was discharged. No steroid treatment was attempted because the out-patient based follow-up examinations showed an improvement in the pneumonia. A chest CT scan was performed 4 months after discharge and revealed resolving pneumonia.
TACE is widely performed to extend life expectancy for HCC patients. DEB is a novel treatment method designed to continuously release doxorubicin when administrated via the hepatic artery5.
Postembolization syndrome is the most common complication characterized by transient abdominal pain, fever and hepatotoxicity and occurs in 60% to 80% of patients who have received TACE. Fortunately, it resolves within a few days. Injury to the normal hepatic parenchymal tissue or cancer cell necrosis is attributed as the cause of the syndrome6. Other possible severe complications are liver abscess, sepsis, acute liver failure, upper gastrointestinal hemorrhage, and biloma. It is rare for a pulmonary related complication of thrombosis to occur as a result of the arteriovenous shunt invading the portal vein or the hepatic vein7.
Due to its nonspecific clinical features and diverse etiologies, differential diagnosis is not straightforward in most cases. In this case, COP developed after TACE. The diagnosis was supported by the fact that antibiotic treatment was administered to no avail, negative results were observed in the microorganism tests including cultures, and the patient had no drug history.
A high-resolution computed tomography performed at the diagnosis did not show a definite active lung parenchymal lesion. However, gradually aggravating dyspnea developed 2 months after receiving two courses of TACE. Chest CT scan revealed multifocal patchy consolidation, ground glass opacity, and fibrotic bands in both peripheral lung areas (Figure 1). In addition, positron emission tomography-computed tomography (PET-CT) was performed the day after the first TACE treatment and showed ground-glass opacity patch lesions in the right lower lung. This was presumed to be from dye smeared in through the shunt, which might have caused interstitial pneumonitis in the future (Figure 3).
Doxorubicin in DEB is an anthracycline antibiotic and a cytotoxic agent used for the treatment of cancer. Among many possible side effects, it is known to cause cardiac toxicity. In 10% of patients, it causes congestive heart failure as the total dose reaches approximately 450 to 550 milligrams per square meter8. Although many cytotoxic medications, especially bleomycin and cyclophosphamide, may induce acute lung toxicity, doxorubicin has not been reported to cause pulmonary complications. There is documented evidence of radiation recall acute inflammation reactions with the use of medications including anticancer agents on an area previously exposed to radiation in breast cancer patients treated with radiotherapy9. Doxorubincin was the suspected cause of those symptoms. However, the patient in our study did not have a history of radiotherapy. We observed a lesion that we suspect was caused by the arteriovenous shunt during the procedure (Figure 4), and embolization was performed closer to the shunt. As shown in Figure 3, the PET-CT, which was performed on the day after the first TACE procedure, showed abnormal changes on both lower lobes indicating doxorubicin induced pulmonary toxicity smeared in to the pulmonary vascular system through the shunt.
Doxorubicin related pulmonary toxicity is not common, yet it has been reported to cause acute lung injury, acute respiratory distress syndrome, COP, and pulmonary fibrosis4. Even though standardized treatment guidelines have not been developed, proper oxygen delivery, care using a ventilator if required, and the empirical use of corticosteroids depending on the severity of the pulmonary injury may easily restore doxorubicin induced pulmonary complications10. There was a report that steroids can be used to resolve symptoms and pulmonary complications4. When symptoms are not severe as in this case, conservative treatment and observation over time may be adequate for treatment11. The decision of whether or not to initiate steroid therapy should be carefully made depending on each patient's disease status.
COP is known to have an indolent nature and a relatively good prognosis. If untreated, it becomes aggravated over several weeks but spontaneous remission may occur. Corticosteroids are generally effective resulting in rapid improvement of clinical symptoms and significant sequelae appearing on chest X-rays. The effective therapeutic dose has not been determined. Frequent relapse, due to premature lowering or discontinuation of corticosteroids, may prolong the treatment period. As mentioned above, the therapeutic dose for treatment has not been set. Empirically, methylprednisolone is started at 0.75-1.5 mg/kg/day and is reduced over several weeks. The treatment is expected to run for 3 to 6 months, but may be extended for up to 1 year in some cases. Relapse is fairly common and occurs in 13% to 58% of patients depending on the severity of the patient's underlying disease and treatment period. A consensus on corticosteroid therapy has not yet been established. It is appropriate to use corticosteroid therapy with a minimum dose and maintain if for as short a period of time as possible. However, the duration of the treatment must belong enough to prevent recurrence of the disease. The patient should be monitored on an ongoing basis for adverse effects related to the treatment.
TACE is a widely used palliative therapy for HCC, but it is known to cause various complications. COP is a rare complication. The purpose of this report is to share the first case of post-TACE COP in Korea.
Figures and Tables
 | Figure 1(A) Initial computed tomography (CT) scan upon diagnosis in November 2013. (B) Follow-up CT scan after two courses of transcatheter arterial embolization (TACE) with symptom of dyspnea. (C) Follow-up CT scan 4 months after discharge. No active lung lesion was observed before TACE as indicated (A). After TACE, multifocal patchy consolidation, ground glass appearance, and fibrotic bands appeared on both peripheral lung fields as indicated (B). (C) An improvement in the lung lesions over time. |
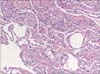 | Figure 2Patchy distribution of organizing pneumonia with preserved lung architecture was observed (H&E stain, ×400). |
References
1. Cazzato S, Zompatori M, Baruzzi G, Schiattone ML, Burzi M, Rossi A, et al. Bronchiolitis obliterans-organizing pneumonia: an Italian experience. Respir Med. 2000; 94:702–708.
2. Chang J, Han J, Kim DW, Lee I, Lee KY, Jung S, et al. Bronchiolitis obliterans organizing pneumonia: clinicopathologic review of a series of 45 Korean patients including rapidly progressive form. J Korean Med Sci. 2002; 17:179–186.
3. Epler GR. Bronchiolitis obliterans organizing pneumonia, 25 years: a variety of causes, but what are the treatment options? Expert Rev Respir Med. 2011; 5:353–361.
4. Aladdin M, Ilyas M. Chemoembolization of hepatocellular carcinoma with drug-eluting beads complicated by interstitial pneumonitis. Semin Intervent Radiol. 2011; 28:218–221.
5. Sacco R, Bargellini I, Bertini M, Bozzi E, Romano A, Petruzzi P, et al. Conventional versus doxorubicin-eluting bead transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2011; 22:1545–1552.
6. Shin SW. The current practice of transarterial chemoembolization for the treatment of hepatocellular carcinoma. Korean J Radiol. 2009; 10:425–434.
7. Xia J, Ren Z, Ye S, Sharma D, Lin Z, Gan Y, et al. Study of severe and rare complications of transarterial chemoembolization (TACE) for liver cancer. Eur J Radiol. 2006; 59:407–412.
8. Ryu JH. Chemotherapy-induced pulmonary toxicity in lung cancer patients. J Thorac Oncol. 2010; 5:1313–1314.
9. Jacobs C, Slade M, Lavery B. Doxorubicin and BOOP. A possible near fatal association. Clin Oncol (R Coll Radiol). 2002; 14:262.
10. Stover DE, Milite F, Zakowski M. A newly recognized syndrome: radiation-related bronchiolitis obliterans and organizing pneumonia. A case report and literature review. Respiration. 2001; 68:540–544.
11. Ogo E, Komaki R, Fujimoto K, Uchida M, Abe T, Nakamura K, et al. A survey of radiation-induced bronchiolitis obliterans organizing pneumonia syndrome after breast-conserving therapy in Japan. Int J Radiat Oncol Biol Phys. 2008; 71:123–131.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download