Abstract
Occupational lung diseases are caused by several toxic substances including heavy metals; however, the exact pathologic mechanisms remain unknown. In the workplace, dental technicians are often exposed to heavy metals such as cobalt, nickel, or beryllium and occasionally develop occupational lung diseases. We described a case of occupational lung disease in a patient who was employed as a dental technician for over a decade. A 31-year-old, non-smoking woman presented with productive cough and shortness of breath of several weeks duration. Chest computed tomography revealed a large number of scattered, bilateral small pulmonary nodules throughout the lung field, and multiple mediastinal lymph nodes enlargement. Percutaneous needle biopsy showed multifocal small granulomas with foreign body type giant cells suggestive of heavy metals inhalation. The patient's condition improved on simple avoidance strategy for several months. This case highlighted the importance of proper workplace safety.
There are many occupational lung diseases related to various toxic substances1, and respiratory system is a major route of occupational diseases2. Heavy metals, such as cobalt, nickel, or beryllium are one of the most common substances that is found in occupational lung diseases.
Common occupational lung diseases include pneumoconiosis, occupational asthma, lung granulomatosis, hypersensitivity pneumonitis, silicosis, asbestosis, contact dermatitis, and sick building syndrome1234567.
Various types of pneumoconioses have been reported in dental technicians18, which are named according to the related toxic materials such as silicosis, asbestosis, hard metal disease, and the so-called dental technician's pneumoconiosis, in which Cr-Co-Mo alloys could play a role1. Dental technicians are, indeed, exposed to various dusts and other forms of chemicals when polishing and grinding prosthetics and during casting operations1. And, these occupational exposure can be different from person to person according to the working conditions and used materials4.
Therefore, dental technicians should be aware of the risk of occupational lung diseases37 and also should be educated about proper protection and proper environment of workplace347. Once occupational lung diseases are suggested, they should visit hospital for confirmative diagnosis and proper management.
Because early radiologic findings of occupational lung diseases are non-specific, differential diagnosis might be very difficult without discrete occupational history and specific pathologic findings. Diagnosis of occupational lung disease should be based on the physician's suspicion, and the mineralogic studies, which had found that bronchoalveolar lavage and/or lung biopsies can be used to confirmative diagnosis of occupational lung disease1.
A 31-year-old, non-smoking woman presented with multiple symptoms, including productive cough, shortness of breath, and purulent sputum without fever or weight loss, and reported that she had been experiencing the symptoms for approximately 1 month. The patient's medical history included diagnosis of rheumatoid arthritis 5 years prior to this visit at another hospital, where she was treated with non-steroidal anti-inflammatory drugs (prednisolone had been excluded). A year later, the patient developed cough and hemoptysis that persisted for several months, and sputum culture results were positive for Mycobacterium tuberculosis. Therefore, the patient was diagnosed with pulmonary tuberculosis (TB) of the right lower lobe and received treatment with anti-TB medication for 9 months. There were no other significant events in her medical history.
As part of our physical examination, pulmonary auscultation during inspiration, we found out that breathing sound deceased lightly with mild end-inspiratory crackles at both lower lung fields. No other significant abnormalities were noted during physical examination. Laboratory tests results were as below: white blood count was 7,900/mm3, eosinophil count was 3.8% (300/mm3), hemoglobin level was 11.7 g/dL, and C-reactive protein level was 0.42 mg/dL. Sputum smear for acid-fast bacilli and bacterial culture of sputum were both negative.
Chest radiography revealed bronchial thickening in the right lower lobe and bilateral hilar lymph nodes enlargement, possibly due to pneumonia or recurrent TB. For inspection of the hilar lymph nodes enlargement, the patient underwent computed tomography (CT). The chest CT revealed a large number of small, scattered, bilateral pulmonary nodules throughout the lung field. A number of bilateral hilar and mediastinal lymph nodes enlargements were also observed. Based on these findings, the patient was suspected to have miliary TB with lymphadenopathies or sarcoidosis (Figure 1A).
The patient's pulmonary function test results showed a forced expiratory volume in 1 second (FEV1) of 2.94 L (103% of predicted value), forced vital capacity (FVC) of 3.26 L (99% of predicted value), FEV1/FVC of 90.2%, and diffusing lung capacity for carbon monoxide by alveolar volume of 74%. No other abnormal findings besides a slight decrease in diffusing capacity were noted.
Angiotensin converting enzyme level in serum was 62 U/L (normal range, 12-68 U/L).
To assist our differential diagnosis, we opted to perform a lung tissue biopsy, using fine needle aspiration biopsy (FNAB). Histologically, the biopsied tissue showed relatively well-preserved lung parenchyme except for multifocal non-caseating granulomas (Figure 2), and we assumed that they were located in the miliary nodules which were observed on the chest CT. These non-caseating granulomas contained a number of multinucleated foreign body type giant cells (Figure 2B), which appeared to have ingested metal debris (Figure 2C), forming needle-shaped particles, suspected as inorganic substances (Figure 2D). We assumed that granuloma formation was the progression of inflammation caused by inhalation of inorganic substances such as heavy metals. Therefore, we concluded that these non-caseating granulomas were associated with occupational exposure.
We then questioned the patient regarding her employment history and the work place environment. The patient revealed she had been employed as a dental technician for over 10 years, and did not usually wear protective equipments such as mask or glasses. In workplace, as dental technician, patient worked with polished and grinded prosthetics and casting operations. During the work, patient might be exposed and inhalated heavy metal such as cobalt, nickel, or beryllium. Since CT had revealed a large number of tiny pulmonary nodules throughout the lung fields, which are not common findings in advanced cases of pneumoconiosis (e.g., in miners and glass factory workers), we presumed that these nodules were the result of acute and sub-acute inflammatory responses linked to occupational exposure. As acute response, we treated patient with simple avoidance therapy and education without any medication. We educated the patient regarding risk management in the workplace, and advised her to wear a dust mask and avoid any situation where dust could be present.
The patient was hospitalized for a week to facilitate further examination and stabilization. During the admission period, the patient discontinued all employment-related activity and following avoidance strategy, her symptoms much improved. After discharge, outpatient observation and periodic examinations were conducted. After 3 months later, the patient's symptoms such as shortness of breath, productive cough, and purulent sputum expectoration had nearly disappeared. Follow-up chest CT confirmed that the size and number of nodules had significantly decreased, and that the consolidations had much improved (Figure 1B). The size of enlarged hilar lymph nodes and number of other enlarged mediastinal lymph nodes had also significantly decreased.
Dental technicians are at high risk of occupational lung diseases179, because they are frequently exposed to dust, chemical substances, toxic materials, and heavy metals used in the construction of dental prostheses and orthodontic appliances19. From those occupational lung diseases, the incidence of pneumoconiosis in dental technicians are higher than expected. And, the prevalence of pneumoconiosis in dental technician are from 9.8% to 24.2% in several reports3510. During construction of dental appliances or dental procedures, various toxic solvents and non-organic gases can be released into the air, leading to occupational lung disease11. The addition of metal alloys, ceramics, acrylates, as well as finishing, grinding, and casting, may all increase the amount of heavy metals released.
Differential diagnosis based on clinical manifestations including subjective symptoms and radiological findings could be almost impossible due to their lack of specificity at earlier stage. In our case, the patient had experienced respiratory symptoms for one month, and various diseases were suspected based on her radiography and CT results, including infectious and non-infectious diseases. To reach a definitive diagnosis, we ran various laboratory tests and sputum culture to rule out various causes of infection.
As one study has reported that alveolar lavage and/or biopsy could be helpful in the diagnosis of similar conditions1, pathologic study might be necessary for exact diagnosis especially at early stage. For the confirmative diagnosis, we compared the usefulness and safety of FNAB and video-assisted thoracoscopy (VATS) for adequate pathologic confirmation, and chose FNAB in left upper lobe with the consideration of patient's comfort and potential risk of VATS.
Based on the results of biopsy, we confirmed that the pulmonary nodules contained granulomatous inflammation including foreign bodies (Figure 1). Finally, considering the patient's occupational history, we reached our final diagnosis of pulmonary granulomatosis, caused by occupational exposure and inhalation of heavy metals and inorganic dust8911. The pathologic findings were different from TB which shows granulomas with caseous necrosis including Langhans' giant cells. Although it is similar to sarcoidosis having non-caseating granulomas, inorganic substances within giant cells are specific for foreign body granulomatosis by inorganic dust inhalation, common in dental technicians.
To protect dental technicians, several preventative measures should be taken to reduce the incidence of occupational lung disease. Firstly, metal alloys that do not contain nickel or beryllium should be chosen to construct dental prosthesis4. Secondly, local proper ventilation systems must be constructed to prevent respiratory and dermal exposure to airborne contaminants, and adequate general ventilation and enclosure systems must be provided458. Thirdly, eating, drinking, and smoking should all be prohibited in the workplace, as these activities can increase the technician's exposure to toxic materials412. And lastly, dental technicians should be educated regarding workplace safety, early detection techniques, and the importance of proper personal protective equipments4.
As we have reported in this case, both education and avoidance therapy are important in the prevention and treatment of workers with occupational lung disease. Proper management can lead to improvement in the patient's symptoms, even after the disease has already occurred. Since these diseases cause non-specific respiratory symptoms, we should evaluate more detailed working conditions including working hours, workplace environmental conditions, length of employment, and additionally we asked whether the patient takes the appropriate preventative measures during the working process9. A first level of treatment should consist of avoidance and prevention, and a second level of treatment should include the addition of symptomatic management. Together, these steps can stop the progression of disease, and potentially reverse existing pulmonary lesions.
In this case, the condition of the patient was improved in symptoms even during the admission period without exposure to the working environment. After 3 months of avoidance treatment, follow-up chest CT showed that both hilar and mediastinal lymph nodes enlargement and multiple small nodules were disappeared.
In Korea, this report is the first case report of pulmonary granulomatosis occurred in dental technicians until now. When considering the relatively high incidence of pneumoconiosis in dental technicians from other reports, there could be many undetected cases of occupational lung disease due to lack of suspicion even in Korea. Also, with the development of more efficient ventilating systems and adequate precaution in the working place worldwide in the recent decades, thus the risk of occupational lung disease might be decreasing in the dental technicians.
In conclusion, the probability of occupational lung disease should be considered in dental technicians, especially in the case with chronic respiratory symptoms even before definitive radiologic abnormalities are noted. Detailed occupational history including the extent of exposure and the presence of adequate preventive management is the most important first step before the confirmative diagnostic procedure which could cause potential patients' discomfort and complications. And, even after diffuse radiologic abnormalities are found, avoidance treatment might improve symptoms and possibly, radiologic extent of the disease might as well.
Figures and Tables
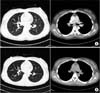 | Figure 1Chest computed tomography (CT) on admission (A) and at 3 months after suitable precaution (B). (A) Chest CT on admission showed multiple small nodules in both lower lung fields. Both hilar and mediastinal lymph nodes enlargement are also seen. (B) After 3 months, multiple small nodules are reduced in size and number. Enlargement of both-hilar and mediastinal lymph nodes are absent. |
 | Figure 2Histologically, the lung biopsy reveals multifocal small and discrete non-caseating epithelioid granulomas containing foreign body-type giant cells. (A) Multifocal granulomas shown in a low power field (H&E stain, ×100). (B) Representative non-caseating epithelioid granulomas containing giant cells engulfing foreign bodies in a high power field (H&E stain, ×400). (C) Typical granuloma containing giant cells engulfing refractile foreign bodies (arrow) (H&E stain, ×400). (D) Typical granulomas containing foreign body-type giant cells engulfing refractile foreign bodies (arrow), which are conspicuous under polarized light microscopy (H&E stain, ×200). |
References
1. Brancaleone P, Weynand B, De Vuyst P, Stanescu D, Pieters T. Lung granulomatosis in a dental technician. Am J Ind Med. 1998; 34:628–631.
2. Park SY, Kim HR, Song J. Workers' compensation for occupational respiratory diseases. J Korean Med Sci. 2014; 29:Suppl. S47–S51.
3. Ozdemir Dogan D, Ozdemir AK, Polat NT, Dal U, Gumus C, Akkurt I. Prevalence of respiratory abnormalities and pneumoconiosis in dental laboratory technicians. Tuberk Toraks. 2010; 58:135–141.
4. Torbica N, Krstev S. World at work: dental laboratory technicians. Occup Environ Med. 2006; 63:145–148.
5. Froudarakis ME, Voloudaki A, Bouros D, Drakonakis G, Hatzakis K, Siafakas NM. Pneumoconiosis among Cretan dental technicians. Respiration. 1999; 66:338–342.
6. Thorette C, Grigoriu B, Canut E, Sobaszek A, Tonnel AB, Tillie-Leblond I. Pulmonary disease in dental laboratory technicians. Rev Mal Respir. 2006; 23:Suppl 2. 4S7–4S16.
7. Abakay A, Atilgan S, Abakay O, Atalay Y, Guven S, Yaman F, et al. Frequency of respiratory function disorders among dental laboratory technicians working under conditions of high dust concentration. Eur Rev Med Pharmacol Sci. 2013; 17:809–814.
8. Kartaloglu Z, Ilvan A, Aydilek R, Cerrahoglu K, Tahaoglu K, Baloglu H, et al. Dental technician's pneumoconiosis: mineralogical analysis of two cases. Yonsei Med J. 2003; 44:169–173.
9. Cimrin A, Komus N, Karaman C, Tertemiz KC. Pneumoconiosis and work-related health complaints in Turkish dental laboratory workers. Tuberk Toraks. 2009; 57:282–288.
10. Choudat D. Occupational lung diseases among dental technicians. Tuber Lung Dis. 1994; 75:99–104.
11. Choudat D, Triem S, Weill B, Vicrey C, Ameille J, Brochard P, et al. Respiratory symptoms, lung function, and pneumoconiosis among self employed dental technicians. Br J Ind Med. 1993; 50:443–449.
12. Hu SW, Lin YY, Wu TC, Hong CC, Chan CC, Lung SC. Workplace air quality and lung function among dental laboratory technicians. Am J Ind Med. 2006; 49:85–92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download