This article has been corrected. See "Erratum: Spontaneous Pulmonary Hematoma with No Underlying Causes: A Case Report" in Volume 79 on page 104.
Abstract
A 57-year-old male patient was admitted to our center because of a cystic mass on the lower portion of the right major fissure that was found incidentally by chest X-ray. He did not have a history of trauma or anticoagulant use. The lesion was removed by video-assisted thoracoscopic surgery. Pathological examination revealed an organizing pulmonary hematoma without any complications, and a follow-up chest X-ray after 1 year showed no recurrence.
Pulmonary hematomas are collections of blood within the alveolar and interstitial spaces1. Usually, they are resolved within two to four weeks. However, if secondary infection accompanies a hematoma, it can progress into an abscess requiring drainage2.
Non-penetrating injury of the thorax, by either direct blunt trauma or indirect forces, is generally known to be the major cause of pulmonary hematoma. There have been a few reports of spontaneous pulmonary hematoma as a complication of anticoagulant therapy or a rare complication of subclavian vein catheterization34. One study reported a total of 38 cases of pulmonary hematoma, and all of these cases occurred after thoracic injury5. To the best of our knowledge, no case of pulmonary hematoma has manifested without any underlying causes. Here, we report a case of spontaneous pulmonary hematoma where the patient did not have any identifiable underlying causes. Pulmonary hematoma was finally diagnosed after histopathological review of the surgically removed mass.
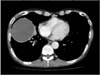
A 57-year-old male patient was admitted to our center because of a cystic mass in the right upper lung field that was discovered incidentally by chest X-ray during a routine health checkup. He was a current smoker with more than 30 pack years of cigarette exposure. He had been diagnosed with chronic obstructive pulmonary disease (COPD) 20 years previously and had been using an inhaled corticosteroid and bronchodilator. The patient has been working at the convenience store, and had no history of trauma or use of any anticoagulants. He had no chest pain, fever, cough, or sputum. There were no other episodes of hemoptysis. His physical examination showed decreased lung sounds in both lung fields without wheezes or crackles. There was no palpable lymph node enlargement. Routine laboratory studies including a platelet count and coagulation profiles yielded normal results, except a slightly increased C-reactive protein (CRP) level (7.13 mg/dL). Pulmonary function tests showed a severe obstructive pattern, the forced expiratory volume in 1 second (FEV1) was 1.38 L (36% of predicted volume); the forced vital capacity (FVC) was 4.08 L (85% of predicted capacity); and the ratio of FEV1 to FVC was 34%. The diffusing capacity was 15.7 mL/mm Hg/min (61% of predictive capacity). Several sputum analyses were negative for malignancy, bacterial infection, and tuberculosis. There was no evidence of human immunodeficiency virus infection. Chest X-ray showed a clearly defined homogeneous round opacity without calcification in the right lower lung field (Figure 1). Computed tomography (CT) scanning of the chest revealed a huge round cystic mass across the upper and lower lobes of the right lung, which measured 9×7.9 cm at its maximum diameter (Figure 2).
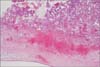
Single port video-assisted thoracoscopic surgery approach using 5-mm scope through a 3.0 cm skin incision was performed under general anesthesia and one lung intubation. After dissection of the pleural adhesions present, a thick yellowish cystic mass with a well-defined margin of 9×8×8 cm in size was found along the major fissure between the right upper and lower lobes (Figure 3). Fine needle aspiration collected a dark brownish colored viscous fluid. The mass was resected completely. Pathological examination revealed a large amount of dense fibrous tissue with blood clots, compatible with pulmonary hematoma (Figure 4), with no evidence of malignant cell infiltration. After postoperative care, the patient was discharged without any complications. A follow-up chest X-ray after 2 months showed no recurrence, and there was no evidence of recurrence 1 year after the follow-up period.
Trauma is known to be the leading cause of pulmonary hematoma, and spontaneous cases are rare56. Anticoagulation therapy, thrombocytopenia, and congenital disorders such as Ehlers-Danlos syndrome have been reported to be causes of spontaneous pulmonary hematoma, but the number of cases is extremely small3478. In the current case, pulmonary hematoma developed without any preexisting causes. To the best of our knowledge, this is the first case of a spontaneous pulmonary hematoma with no underlying conditions.
Generally, pulmonary hematoma is understood to occur by vessel rupture and consequent hemorrhage into the lung parenchyma due to physical trauma to the chest79. Several researchers have proposed another pathological mechanism of hematoma, which involves its occurrence in preexisting cysts via angionecrosis and erosion of the cystic wall410.
We suppose that these pathomechanisms may be applicable to explain the formation of pulmonary hematoma in present case. As the patient had underlying COPD, the elevation of CRP levels detected suggests the possibility of infection leading to necrosis of the walls of preexisting emphysematous bullae and angionecrosis although bullae were not prominent in the area surrounding the hematoma upon CT. Alternatively, as though the patients did not aware, a minor trauma to the chest may be the leading cause of pulmonary hematoma through blood vessels rupture.
While the incidence of hematoma is low, it can be difficult to differentiate malignancy from hematoma in imaging results. When a pulmonary cystic mass is observed, clinicians should be aware of the possibility of a hematoma, even if no underlying symptoms exist.
Figures and Tables
Figure 1
Chest X-rays shows a well-defined round homogenous opacity in the right lower lung field. RPA: posterior anterior view.

Figure 2
Chest computed tomography scanning reveals a 9.0×7.9-cm-sized well-defined cystic mass in the upper and lower lobes of the right lung.
Acknowledgements
The authors thank Professor Gyu Rak Chon for critical review of the manuscript and image evaluation.
References
1. Trinkle JK, Richardson JD, Franz JL, Grover FL, Arom KV, Holmstrom FM. Management of flail chest without mechanical ventilation. Ann Thorac Surg. 1975; 19:355–363.
2. Mathai M, Byrd RP Jr, Roy TM. The posttraumatic pulmonary mass. J Tenn Med Assoc. 1996; 89:41–42.
3. Chakraborty AK, Dreisin RB. Pulmonary hematoma secondary to anticoagulant therapy. Ann Intern Med. 1982; 96:67–69.
4. Kaira K, Takei Y, Matsuura M, Saito R. Pulmonary hematoma resulting from anticoagulant therapy. AJR Am J Roentgenol. 2003; 180:1740.
5. Specht EE. Pulmonary hematoma. Am J Dis Child. 1966; 111:559–563.
6. Williams JR. The vanishing lung tumor: pulmonary hematoma. Am J Roentgenol Radium Ther Nucl Med. 1959; 81:296–302.
7. Luna MA, Leary WV, Jing BS. Pulmonary hematoma associated with thrombocytopenia. Chest. 1970; 57:487–489.
8. Matsushita A, Takayanagi N, Ishiguro T, Harasawa K, Tsuchiya N, Yoneda K, et al. A case of Ehlers-Danlos syndrome suspected from pulmonary hematoma due to disruption of the lung. Nihon Kokyuki Gakkai Zasshi. 2009; 47:704–710.
9. Joynt GH, Jaffe F. Solitary pulmonary hematoma. J Thorac Cardiovasc Surg. 1962; 43:291–302.
10. Jay SJ, Johanson WG Jr. Massive intrapulmonary hemorrhage: an uncommon complication of bullous emphysema. Am Rev Respir Dis. 1974; 110:497–501.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download