Abstract
Malignant melanoma occurs most frequently on the skin. However, it can also arise in other organs and tissues of the body. Primary pulmonary malignant melanoma is a very rare non-epithelial neoplasm accounting for 0.01% of all primary pulmonary tumors. The treatment of choice is surgical resection of the tumor with an oncologically adequate margin as in lobectomy or pneumonectomy. The prognosis of this condition is rather poor. Based on previous data, its 5-year survival is at least 10%. Here, we report a case of an 82-year-old woman whose primary pulmonary melanoma was detected incidentally.
Malignant melanoma is a tumor arising from pigment-producing cells in the deeper layers of the skin. It accounts for 1.5% of all reported cancers. It occurs most frequently on the skin, but also occurs in other organs and tissues of the body. However, melanoma of the lung without evidence of extrapulmonary disease, i.e., primary pulmonary melanoma, is very rare1.
Here, we report the case of an 82-year-old woman in whom primary pulmonary melanoma was detected incidentally. We describe this unusual case and review the relevant literature.
A solitary mass was detected incidentally in the right lower lobe of the lung in an 82-year-old woman. The results of physical examinations and laboratory tests were within normal limits. Chest computed tomography (CT) showed a heterogeneous enhancing mass lesion of approximately 8 cm in the right lower lobe of the lung (Figure 1). Bronchoscopic examination showed a black-pigmented mass in the posterobasal segment of the right lower lobe, and biopsy was performed (Figure 2). Histopathological examination of the biopsy specimen showed melanoma cells containing melanin granules and "nesting" of melanoma cells just beneath the bronchial epithelium. The melanoma cells were round or spindle shaped, with melanin pigmentation, and these cells were positive for human melanoma black 45 (HMB-45) and vimentin and focally positive for antibodies to S-100 protein (Figure 3). Accordingly, the patient was diagnosed with malignant melanoma.
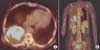
To exclude the possibility of metastasis, an extensive examination was carried out. Positron emission tomography/CT showed a hypermetabolic lesion (standardized uptake value, 14.5) in the right lower lobe of the lung, with no evidence of metastatic disease (Figure 4). The patient had no history of skin lesions, and did not have any skin, ear, or ocular lesions. Gastrointestinal endoscopy, colonoscopy, and gynecological examinations were performed, and no possible primary tumor was detected. The final diagnosis was primary pulmonary melanoma. The patient refused to undergo treatment because of old age and poor general health.
Malignant melanoma mainly occurs on the skin, but has also been described at other mucosal sites and organs, including the paranasal sinuses, oral cavity, esophagus, larynx, vagina, anorectal region, and liver23. Primary pulmonary malignant melanoma is a very rare non-epithelial neoplasm, accounting for 0.01% of all primary pulmonary tumors4. The mean age at diagnosis is 57 years (range, 41-82 years). It is frequently endobronchial and manifests with symptoms of cough, hemoptysis, pneumonia, lobar collapse, or atelectasis. In 30% of cases, primary pulmonary malignant melanoma is an incidental finding on chest radiography2.
The exact pathogenesis of pulmonary malignant melanoma remains controversial. Some likely explanations for the occurrence of pulmonary melanoma are as follows5: (1) migration of benign melanocytes during embryogenesis; (2) the presence of melanocytes and melanocytic proliferation in the larynx and esophagus; (3) a common embryological origin of the larynx, esophagus, and lungs, suggesting possible migration of melanocytes; (4) spontaneous regression of previous skin lesions; and (5) melanogenic metaplasia in the submucosa.
The most important consideration is the exclusion of the metastatic origin of the tumor, because according to some reports, skin melanomas may spontaneously disappear without any trace after they have already metastasized6. A recent comprehensive systemic review of the existing literature showed that the incidence of malignant melanoma with an unknown primary site is estimated to be 3.2%7. The final diagnosis of a primary pulmonary malignant melanoma is established based on clinical, radiological, and pathological findings. Therefore, Allen and Drash8 proposed the following diagnostic criteria for primary pulmonary malignant melanoma9: (1) no history suggestive of a previous melanoma; (2) no demonstrable melanoma in any other organ at the time of surgery; (3) a solitary tumor in the surgical specimen from the lung; (4) tumor morphology compatible with that of a primary tumor; (5) no evidence at autopsy of a primary melanoma elsewhere; (6) obvious melanoma cells confirmed by immunohistochemical staining for S-100 and HMB-45, and possibly by electron microscopy; (7) evidence of junctional change; (8) "nesting" of cells beneath the bronchial epithelium; and (9) invasion of the intact bronchial epithelium by melanoma cells. Our patient had a solitary mass and fulfilled the diagnostic criteria. Moreover, pathological examination showed "nesting" of melanoma cells just beneath the bronchial epithelium, a suggested histopathological criterion for primary pulmonary melanoma. Therefore, she was finally diagnosed as having primary malignant melanoma according to the proposed criteria.
The treatment of choice is surgical resection of the tumor with an oncologically adequate margin, as is lobectomy or pneumonectomy. Some studies have shown that patients undergoing surgical resection have a better prognosis than those treated non-surgically10. In inoperable cases, chemotherapy with dacarbazine and immunotherapy with interleukin-2 or interferon are also considered. The prognosis of this condition is rather poor, but existing data are not sufficient to draw a definitive conclusion. Based on previous data, 5-year survival is at least 10%2. In addition, follow-ups were inadequate in 15% of the patients who were still alive when the case reports were published.
In conclusion, although rare, primary pulmonary malignant melanoma should be considered in the differential diagnosis of primary bronchial tumors of the lung as an extremely rare possibility.
Figures and Tables
 | Figure 1(A, B) Chest computed tomography showing a heterogeneous enhancing mass of 8 cm containing an inner low attenuating portion in the right lower lobe. |
 | Figure 2Bronchoscopy showing a black-pigmented mass in the posterobasal segment of the right lower lobe. |
 | Figure 3(A) Histopathological examination of the biopsy specimen showing melanoma cells containing melanin granules (H&E stain, ×200). (B) Histopathological features of "nesting" of melanoma cells just beneath the bronchial epithelium (H&E stain, ×400). (C) The melanoma cells are round or spindle shaped with melanin pigmentation and positive for human melanoma black 45 (×200). |
References
1. Scolyer RA, Bishop JF, Thompson JF. Primary melanoma of the lung. In : Raghavan D, Brecher ML, Johnson DH, Meropol NJ, Moots PL, Rose PG, editors. Textbook of uncommon cancer. 3rd ed. Chichester: John Wiley & Sons Ltd;2006. p. 293–298.
2. Ost D, Joseph C, Sogoloff H, Menezes G. Primary pulmonary melanoma: case report and literature review. Mayo Clin Proc. 1999; 74:62–66.
3. Gong L, Li YH, Zhao JY, Wang XX, Zhu SJ, Zhang W. Primary malignant melanoma of the liver: a case report. World J Gastroenterol. 2008; 14:4968–4971.
4. Dountsis A, Zisis C, Karagianni E, Dahabreh J. Primary malignant melanoma of the lung: a case report. World J Surg Oncol. 2003; 1:26.
5. Jennings TA, Axiotis CA, Kress Y, Carter D. Primary malignant melanoma of the lower respiratory tract: report of a case and literature review. Am J Clin Pathol. 1990; 94:649–655.
6. Smith JL Jr, Stehlin JS Jr. Spontaneous regression of primary malignant melanomas with regional metastases. Cancer. 1965; 18:1399–1415.
7. Kamposioras K, Pentheroudakis G, Pectasides D, Pavlidis N. Malignant melanoma of unknown primary site. To make the long story short A systematic review of the literature. Crit Rev Oncol Hematol. 2011; 78:112–126.
8. Allen MS Jr, Drash EC. Primary melanoma of the lung. Cancer. 1968; 21:154–159.
9. Jensen OA, Egedorf J. Primary malignant melanoma of the lung. Scand J Respir Dis. 1967; 48:127–135.
10. Seitelman E, Donenfeld P, Kay K, Takabe K, Andaz S, Fox S. Successful treatment of primary pulmonary melanoma. J Thorac Dis. 2011; 3:207–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download