Abstract
Drug-resistant tuberculosis (TB) is still a major threat worldwide. However, recent scientific advances in diagnostic and therapeutic tools have improved the management of drug-resistant TB. The development of rapid molecular testing methods allows for the early detection of drug resistance and prompt initiation of an appropriate treatment. In addition, there has been growing supportive evidence for shorter treatment regimens in multidrug-resistant TB; and for the first time in over 50 years, new anti-TB drugs have been developed. The World Health Organization has recently revised their guidelines, primarily based on evidence from a meta-analysis of individual patient data (n=9,153) derived from 32 observational studies, and outlined the recommended combination and correct use of available anti-TB drugs. This review summarizes the updated guidelines with a focus on the medical management of drug-resistant TB.
The prevalence of tuberculosis (TB) has decreased markedly in Korea since the establishment of the National Tuberculosis Control Program in 1962. However, in recent years, the rate of decrease has slowed1 and multidrug-resistant TB (MDR-TB) has emerged as a significant threat to public health. The proportion of MDR-TB among new cases of TB increased from 1.6% in 1994 to 2.7% in 20042. In addition, according to data from the 2008 Health Insurance Review and Assessment Service, 4.6% of patients (n=2,472) were MDR-TB3. Of these cases, 2.9% were new cases of TB while 9.3% were patients with prior TB treatment history.
Treatment of MDR-TB, compared to drug-sensitive TB, is more difficult given the higher cost, longer treatment period, and more adverse events. Meta-analysis data indicate that the MDR-TB treatment success rate is about 62% worldwide45. In Korea, the treatment success rate varies depending on the study site and ranges from 37.1% to 66.0%6789101112. However, the largest retrospective multicenter cohort study in Korea (n=1,407 MDR-TB patients) showed a treatment success rate of 45.3% and a default rate of 32.3%10.
Recently, the World Health Organization (WHO) revised the MDR-TB management guidelines1314. The revisions incorporate advancements in the diagnosis of drug-resistant TB and the development of new anti-TB drugs. The recommendations are primarily based on evidence from a meta-analysis of individual MDR-TB patient data (n=9,153) from 32 observational studies15. Although few prospective randomized trials have been conducted to support the new recommendations, these guidelines were based on the best evidence available to date. In 2014, the Korean guidelines regarding MDR-TB management were updated in accordance with the WHO guidelines16. This review summarizes the WHO and Korean guidelines for the medical management for drug-resistant TB.
For decades, the laboratory diagnosis of drug-resistant TB has depended on phenotypic, culture-based methods. Diagnostic delays are a major disadvantage of these methods and could result in ineffective treatment, poor outcomes, and the spread of drug-resistant TB. Although other phenotypic methods (e.g., the microscopic observation drug susceptibility assay and the thin layer agar technique) have shortened the delay17, their use is still limited.
With advances in rapid molecular technologies, drug-resistant TB can be diagnosed by a using a molecular (genotypic) or conventional (phenotypic) drug susceptibility test (DST). The new molecular tests significantly reduce diagnostic delays allowing for the prompt initiation of MDR-TB treatment. The WHO endorsed two line probe assays (LPAs) in 200818, the INNO-LiPA Rif.TB (Fujirebio, Ghent, Belgium) and the GenoType MTBDRplus (Hain Lifescience GmbH, Nehren, Germany), and the Xpert MTB/RIF system (Cepheid, Sunnyvale, CA, USA) in 201019. The WHO currently recommends using rapid DSTs over conventional testing or no testing at the time of TB diagnosis1314. Recently several molecular assays for the detection of rifampicin resistance have been developed. In Korea, new commercial molecular assays, REBA MTB-Rifa (YD Diagnostics, Yongin, Korea)2021 and AdvanSureMDR-TB GenoBlot assay (LG Life Sciences, Seoul, Korea)22, are currently available.
In 2013, the WHO revised the case definition of TB and drug-resistant TB in order to incorporate advances in the new molecular DSTs23. "A bacteriologically confirmed case" is now defined as a biologic specimen that is positive by molecular methods as well as smear or culture methods. "Rifampicin resistance" was newly introduced and could be detected using phenotypic or genotypic methods. The revised definitions of drug-resistant TB are included in Table 1.
The WHO recommended against labeling TB cases as "totally drug-resistant" or "extremely drug-resistant" given the concerns about the reliability and reproducibility of DSTs for many anti-TB drugs and insufficient evidence regarding the impact of such results on treatment outcomes. The term "resistance beyond extensively drug-resistant TB (XDR-TB)" is preferred24. Patients with additional resistance beyond XDR-TB showed poorer outcomes25.
WHO-recommended molecular testing methods have a high sensitivity and specificity for the detection of rifampicin resistance. A negative result generally excludes rifampicin resistance and no further confirmatory test is required. However, although a positive result is a reliable indicator for MDR-TB, a false positive is also possible. Molecular methods have a positive predictive value for MDR-TB of only about 60% when the prevalence of rifampicin resistance is 3% (the proportion of MDR-TB among new TB cases in Korea)2627.
When a molecular method detects rifampicin resistance, further treatment or testing depends on the patient's risk of MDR-TB. For patients with a high risk of MDR-TB, an MDR-TB treatment regimen should be initiated. For patients with a low risk of MDR-TB, further confirmatory tests (such as a phenotypic DST, LPA, or sequencing) are required prior to initiation of treatment142829.
The choice of drugs should be based on the DST pattern; however, when interpreting the results, the possibility of resistance amplification should be considered given that conventional DSTs often take several months, i.e., the results do not reflect the bacterial population at the time of regimen design. If a particular drug was included in a failing or an ineffective regimen for over a month while waiting DST result, acquisition of additional resistance to that drug should be considered. The WHO recently emphasized monitoring for possible amplification of rifampicin resistance during treatment, using the Xpert MTB/RIF14. The feasibility and effectiveness of this approach are to be verified by further studies. However, it should be kept in mind that the risk of amplification to MDR is high in the treatment of polyresistant TB and close monitoring is necessary.
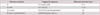
The WHO-suggested regimens for mono- and poly-resistant TB are shown in Table 214. Rifampicin resistance is a reliable indicator of MDR-TB. For patients who are diagnosed with rifampicin resistance using Xpert MTB/RIF, they should be managed in the same way as MDR-TB. Justification of adding isoniazid to the MDR regimen depends on drug resistance data of each country. In Korea, rifampicin monoresistance is rare; therefore, routine addition of isoniazid to the MDR regimen is not recommended16. Isoniazid can be added to the regimen until DST results to isoniazid are available, but it should not be counted as an effective drug.
Early MDR-TB detection and the prompt initiation of an effective treatment regimen are important factors for successful outcomes. The benefits of rapid DSTs for patient and public health include better prognosis, prevention of further drug resistance, and a reduction in the spread of drug-resistant strains.
The results of DSTs are essential for designing the appropriate treatment regimen. However, DSTs for drugs such as ethambutol, streptomycin, and those in group 4 and 5 do not have high reproducibility or reliability. Therefore, the DST results should be interpreted along with a detailed clinical history. If a patient has used a drug as part of a failing regimen for over a month, the strain should be considered "probably resistant," even if the results of the DST indicated susceptibility.
Fluoroquinolones and injectable drugs are two groups of second-line core drugs with potent bactericidal activity. Other second-line drugs are accompanying drugs that are responsible for protecting the core drugs against resistance. To build a MDR-TB treatment regimen, begin with two core drugs (a fluoroquinolone and an injectable drug) and then add oral second-line drugs in the following order: ethionamide or protionamide, cycloserine, and p-aminosalicylic acid (PAS)142829. If the preceding drugs are not sufficient to make a regimen, group 1 and then group 5 drugs could also be added.
The recent WHO guidelines have changed the priority of first-line drugs14. Although first-line drugs were previously given the highest priority for inclusion in treatment regimens (if the strain showed susceptibility to the drugs)3031, the meta-analysis have shown only a slight benefit or no benefit for successful outcomes15. Similarly, group 5 drugs showed no association with successful outcomes. Based on such clinical evidence, first-line drugs and group 5 drugs may be included in a regimen but should not to be considered as active drugs.
The optimal number of drugs required to cure MDR-TB is not known. The meta-analysis showed that the use of at least four active drugs in the intensive phase and three active drugs in the continuation phase was likely to be effective15. There was no evidence to support the use of more than four second-line drugs in patients with extensive disease. Increasing the number of second-line drugs is permissible if the effectiveness of some drugs is uncertain. As opposed to this recommendation, several retrospective cohort studies showed that an aggressive regimen of at least 5 likely effective drugs during the intensive phase was associated with a reduced risk of treatment failure, death or relapse 323334.
Based on clinical evidence from the meta-analysis, the intensive phase of treatment should consist of at least pyrazinamide, a fluoroquinolone, an injectable drug, protionamide (or ethionamide), and cycloserine (or PAS if cycloserine cannot be used).
There have been controversies concerning the optimal duration for injectable drug use and total treatment. The American Thoracic Society guidelines from 2003 recommended a maximum cumulative streptomycin dose of 120 g (due to its cumulative toxic effects) but did not mention any other injectable drugs35. The WHO had suggested the time following sputum conversion in the recommendation of treatment duration. In 1997, the WHO recommended a minimum intensive phase of 3 months or until after culture conversion36. The 2006 and 2008 WHO guidelines recommended an intensive phase of at least 6 months or at least 4 months after culture conversion3031. However, in the 2011 and 2014 guidelines, the time for the intensive phase was increased to a minimum of 8 months and bacteriological conversion was not considered1314. This recommendation was based on clinical evidence from the meta-analysis, which did not determine the optimal time following culture conversion15. Therefore, the injectable drugs are recommended to use for at least eight months, but the duration can be modified based upon severity of disease, prior therapy, drug resistance patterns, response to therapy, and timing of sputum conversion.
Currently, the WHO recommends a total treatment duration of 20 months for patients who had no previous MDR-TB treatment. Patients who have had previous treatment for MDR-TB may need longer treatment. The duration may be modified depending on bacteriological status and other indicators of treatment progress.
A non-randomized study conducted in Bangladesh reported very promising results with a 9-month regimen37, and a randomized controlled trial is ongoing to test a shorter regimen38. However, until sufficient evidence is available, a shorter treatment regimen is not recommended as a standard. In addition, treatment with new drugs, such as bedaquiline39 and delamanid40, may allow for shorter MDR-TB therapy; however, optimization studies of these drugs are needed.
One of the major changes in the revised WHO guidelines is how to include ethambutol and pyrazinamide in the MDR regimen. In the previous guidelines, ethambutol and pyraziamide were recommended as the first option in the drug selection (as part of four active drugs) if susceptibility was shown3031. However, in the meta-analysis, pyrazinamide showed only a slightly added benefit and ethambutol was associated with a marginal but statistically significant reduction in the likelihood of cure15. Therefore, based on clinical evidence, ethambutol and pyrazinamide may be included in MDR-TB treatment regimens but should not be considered active drugs.
Pyrazinamide has poor bactericidal activity, but it has potent sterilizing activity that contributes to a shorter treatment duration. Given its promising potential, pyrazinamide is routinely added to MDR-TB treatment regimens if susceptibility is documented or unknown29. Although the WHO has recently recommended routine use of pyrazinamide even if the strain shows resistance14, this recommendation should be verified by further studies. A recent retrospective study showed that the WHO-recommended regimen in which pyrazinamide was not likely effective was associated with higher mortality rates41.
Pyrazinamide can be used for the entire treatment or at least for the intensive phase. Pyrazinamide is generally used with companion rifampicin for the treatment of susceptible TB. Given that rifampicin also has a potent sterilizing action, pyrazinamide is recommended to be used during the first 2 months of treatment only. While rifampicin is no longer active in MDR-TB treatment, pyrazinamide may continue working after the first few months of treatment42. In addition, many MDR-TB patients have chronically inflamed lungs, which theoretically produce the acidic environment where pyrazinamide is active14.
In contrast, ethambutol is not routinely added to MDR-TB treatment regimens. Although ethambutol can be added in the regimen, it is never considered an active drug, even if the strain shows susceptibility14.
Among the injectable drugs, there is currently no strong evidence to indicate which drugs are superior in terms of efficacy or adverse effects. The meta-analysis did not show any injectable to be superior to any other15. Therefore, the choice of injectable drug depends on the availability and resistance in each country. In Korea, capreomycin is not readily available and amikacin is usually injected intravenously; thus, kanamycin is the recommended first choice of injectable drugs16.
In contrast, streptomycin is not recommended because of high rates of resistance in patients with MDR-TB. However, streptomycin should be considered in cases where the strain is resistant to all other second-line injectable drugs given that there is little cross-resistance between streptomycin and the other injectable drugs14.
Fluoroquinolones, especially later-generation fluoroquinolones, have been shown to be significantly associated with cure15. Consequently, fluoroquinolones should always be used in MDR-TB treatment. Moxifloxacin or levofloxacin is preferred while ciprofloxacin and ofloxacin are not recommended given their weaker efficacy. The dosage recommendation for levofloxacin is 750-1,000 mg/day. Although moxifloxacin has better in vitro activity against TB compared to levofloxacin, a recent randomized trial conducted in Korea revealed that moxifloxacin and levofloxacin have comparable efficacy in terms of 3-month culture conversion rates and adverse events43. The WHO recommends, despite lack of evidence, the use of moxifloxacin even if levofloxacin (or ofloxacin) resistance is documented because there is no complete cross-resistance between these fluoroquinolones14.
In the 2008 WHO guidelines31, there was no preference among group 4 drugs. However, in the meta-analysis, ethionamide demonstrated a stronger association with successful outcome than cycloserine or PAS15. Furthermore, cycloserine demonstrated a stronger association than PAS; therefore, ethionamide or protionamide is preferred followed by cycloserine and, subsequently, PAS.
Group 5 drugs did not show an association with successful outcomes in the meta-analysis15; however, linezolid and high-dose isoniazid could not be analyzed due to the small number of cases. Therefore, group 5 drugs may be used if drugs from groups 2-4 are not likely to be effective; however, group 5 drugs are not included among active drugs. A recent meta-analysis showed that only linezolid was independently associated with favorable outcomes in the treatment of XDR-TB or fluoroquinolone-resistant MDR-TB45. There is renewed interest in the efficacy of clofazimine. A randomized controlled trial in China showed that clofazimine accelerated sputum culture conversion and improved treatment success rates in the treatment of MDR-TB46.
There are few evidences regarding the drug selection sequence in group 5 drugs. Many experts agreed that linezolid is the first option and clofazimine and meropenem/clavulanic acid may be more effective than clarithromycin or amoxicillin/clavulanic acid28. Recently, bedaquiline and delamanid have been listed in group 5 as well14.
The principles of XDR-TB management are similar to those of MDR-TB management. However, the design of a treatment regimen for XDR-TB is more complex and referral to an expert is strongly recommended. Although, DST for ethambutol, pyrazinamide, and second-line TB drugs do not have high reproducibility or reliability, it appears to provide clinically useful information to guide selection of treatment regimens for MDR and XDR TB47. Any drug that the isolate is susceptible to from group 1 and any remaining available drugs from groups 3 or 4 are added to the regimen. Group 5 drugs are often required to make a regimen as well.
The optimal number of drugs and the duration of treatment are still uncertain. In a meta-analysis conducted by Falzon et al.48, treatment success was highest if at least six drugs were used in the intensive phase and four in the continuation phase. The odds of success were maximized when the duration of the intensive phase was 6.6-9.0 months and the total duration of treatment was 20.1-25.0 months. These results suggest that the optimal treatment of XDR-TB patients requires a similar duration but more drugs than treatment for non-XDR MDR-TB.
The use of later-generation fluoroquinolones, such as moxifloxacin, significantly improved treatment outcomes of XDR-TB even when a DST demonstrated resistance to a representative fluoroquinolone49. Linezolid may also represent a valuable drug to treat cases of XDR-TB5051. New drugs, such as bedaquiline5253 and delamanid54, and new combination regimen55 are expected to enhance the cure rate of XDR-TB. Adjunctive surgery should be considered in localized disease cases and rigorous respiratory infection control measures are also important.
A rapid diagnosis of drug resistance and the subsequent initiation of an appropriate treatment are crucial in the management of drug-resistant TB. Using current recommendations, drug-resistant TB can largely be cured with the right combination and use of available anti-TB drugs. However, controlled trials are needed to improve the quality of existing evidence. In addition, further studies for optimization of new drugs and shorter treatment regimens for MDR-TB are needed.
Figures and Tables
Table 1
Definitions of drug-resistance23
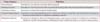
Table 2
Suggested regimens for mono and polyresistant TB14
References
1. Park YK, Park YS, Na KI, Cho EH, Shin SS, Kim HJ. Increased tuberculosis burden due to demographic transition in Korea from 2001 to 2010. Tuberc Respir Dis. 2013; 74:104–110.
2. Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, et al. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007; 11:571–576.
3. Park YS, Hong SJ, Boo YK, Hwang ES, Kim HJ, Cho SH, et al. The national status of tuberculosis using nationwide medical records survey of patients with tuberculosis in Korea. Tuberc Respir Dis. 2012; 73:48–55.
4. Johnston JC, Shahidi NC, Sadatsafavi M, Fitzgerald JM. Treatment outcomes of multidrug-resistant tuberculosis: a systematic review and meta-analysis. PLoS One. 2009; 4:e6914.
5. Orenstein EW, Basu S, Shah NS, Andrews JR, Friedland GH, Moll AP, et al. Treatment outcomes among patients with multidrug-resistant tuberculosis: systematic review and meta-analysis. Lancet Infect Dis. 2009; 9:153–161.
6. Kim HJ, Hong YP, Kim SJ, Lew WJ, Lee EG. Ambulatory treatment of multidrug-resistant pulmonary tuberculosis patients at a chest clinic. Int J Tuberc Lung Dis. 2001; 5:1129–1136.
7. Park SK, Lee WC, Lee DH, Mitnick CD, Han L, Seung KJ. Self-administered, standardized regimens for multidrug-resistant tuberculosis in South Korea. Int J Tuberc Lung Dis. 2004; 8:361–368.
8. Kim HR, Hwang SS, Kim HJ, Lee SM, Yoo CG, Kim YW, et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007; 45:1290–1295.
9. Kwon YS, Kim YH, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Treatment outcomes for HIV-uninfected patients with multidrug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 2008; 47:496–502.
10. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008; 178:1075–1082.
11. Park JK, Koh WJ, Kim DK, Kim EK, Kim YI, Kim HJ, et al. Treatment outcomes and prognostic factors in patients with multidrug-resistant tuberculosis in Korean private hospitals. Tuberc Respir Dis. 2010; 69:95–102.
12. Jeon DS, Shin DO, Park SK, Seo JE, Seo HS, Cho YS, et al. Treatment outcome and mortality among patients with multidrug-resistant tuberculosis in tuberculosis hospitals of the public sector. J Korean Med Sci. 2011; 26:33–41.
13. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Geneva: World Health Organization;2011.
14. World Health Organization. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: World Health Organization;2014.
15. Ahuja SD, Ashkin D, Avendano M, Banerjee R, Bauer M, Bayona JN, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: an individual patient data meta-analysis of 9,153 patients. PLoS Med. 2012; 9:e1001300.
16. Joint Committee for the Revision of Korean Guidelines for Tuberculosis. Korean Centers for Disease Control and Prevention. Korean guidelines for tuberculosis. 2nd ed. Seoul and Cheongwon: Joint Committee for the Revision of Korean Guidelines for Tuberculosis;Korean Centers for Disease Control and Prevention;2014.
17. Minion J, Leung E, Menzies D, Pai M. Microscopic-observation drug susceptibility and thin layer agar assays for the detection of drug resistant tuberculosis: a systematic review and meta-analysis. Lancet Infect Dis. 2010; 10:688–698.
18. World Health Organization. Policy statement. Molecular line probe assay for rapid screening of patients at risk of multidrug-resistant tuberculosis (MDR-TB). Geneva: World Health Organization;2008.
19. World Health Organization. Policy statement. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF system. Geneva: World Health Organization;2011.
20. Bang H, Park S, Hwang J, Jin H, Cho E, Kim DY, et al. Improved rapid molecular diagnosis of multidrug-resistant tuberculosis using a new reverse hybridization assay, REBA MTB-MDR. J Med Microbiol. 2011; 60:1447–1454.
21. Cho E, Shamputa IC, Kwak HK, Lee J, Lee M, Hwang S, et al. Utility of the REBA MTB-Rifa(R) assay for rapid detection of rifampicin resistant Mycobacterium tuberculosis. BMC Infect Dis. 2013; 13:478.
22. Moon HW, Hur M, Kim JY, Yun YM. Comparison of three molecular assays for the detection of rifampin resistance in Mycobacterium tuberculosis. J Clin Lab Anal. 2015; 29:142–145.
23. World Health Organization. Definitions and reporting framework for tuberculosis: 2013 revision. Geneva: World Health Organization;2013.
24. Calligaro GL, Moodley L, Symons G, Dheda K. The medical and surgical treatment of drug-resistant tuberculosis. J Thorac Dis. 2014; 6:186–195.
25. Migliori GB, Sotgiu G, Gandhi NR, Falzon D, DeRiemer K, Centis R, et al. Drug resistance beyond extensively drug-resistant tuberculosis: individual patient data meta-analysis. Eur Respir J. 2013; 42:169–179.
26. Weyer K, Mirzayev F, Migliori GB, Van Gemert W, D'Ambrosio L, Zignol M, et al. Rapid molecular TB diagnosis: evidence, policy making and global implementation of Xpert MTB/RIF. Eur Respir J. 2013; 42:252–271.
27. Arentz M, Sorensen B, Horne DJ, Walson JL. Systematic review of the performance of rapid rifampicin resistance testing for drug-resistant tuberculosis. PLoS One. 2013; 8:e76533.
28. Lange C, Abubakar I, Alffenaar JW, Bothamley G, Caminero JA, Carvalho AC, et al. Management of patients with multidrug-resistant/extensively drug-resistant tuberculosis in Europe: a TBNET consensus statement. Eur Respir J. 2014; 44:23–63.
29. Partners In Health. The PIH guide to the medical management of multidrug-resistant tuberculosis. 2nd ed. Boston: Partners In Health;2014.
30. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: World Health Organization;2006.
31. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. Geneva: World Health Organization;2008.
32. Mitnick CD, Franke MF, Rich ML, Alcantara Viru FA, Appleton SC, Atwood SS, et al. Aggressive regimens for multidrug-resistant tuberculosis decrease all-cause mortality. PLoS One. 2013; 8:e58664.
33. Franke MF, Appleton SC, Mitnick CD, Furin JJ, Bayona J, Chalco K, et al. Aggressive regimens for multidrug-resistant tuberculosis reduce recurrence. Clin Infect Dis. 2013; 56:770–776.
34. Velasquez GE, Becerra MC, Gelmanova IY, Pasechnikov AD, Yedilbayev A, Shin SS, et al. Improving outcomes for multidrug-resistant tuberculosis: aggressive regimens prevent treatment failure and death. Clin Infect Dis. 2014; 59:9–15.
35. Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003; 167:603–662.
36. World Health Organization. Treatment of tuberculosis: guidelines for national programmes. 2nd ed. Geneva: World Health Organization;1997.
37. Van Deun A, Maug AK, Salim MA, Das PK, Sarker MR, Daru P, et al. Short, highly effective, and inexpensive standardized treatment of multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2010; 182:684–692.
38. Nunn AJ, Rusen ID, Van Deun A, Torrea G, Phillips PP, Chiang CY, et al. Evaluation of a standardized treatment regimen of anti-tuberculosis drugs for patients with multi-drug-resistant tuberculosis (STREAM): study protocol for a randomized controlled trial. Trials. 2014; 15:353.
39. Diacon AH, Pym A, Grobusch M, Patientia R, Rustomjee R, Page-Shipp L, et al. The diarylquinoline TMC207 for multidrug-resistant tuberculosis. N Engl J Med. 2009; 360:2397–2405.
40. Gler MT, Skripconoka V, Sanchez-Garavito E, Xiao H, Cabrera-Rivero JL, Vargas-Vasquez DE, et al. Delamanid for multidrug-resistant pulmonary tuberculosis. N Engl J Med. 2012; 366:2151–2160.
41. Franke MF, Becerra MC, Tierney DB, Rich ML, Bonilla C, Bayona J, et al. Counting pyrazinamide in regimens for multidrug-resistant tuberculosis. Ann Am Thorac Soc. 2015; 12:674–679.
42. Caminero JA, Sotgiu G, Zumla A, Migliori GB. Best drug treatment for multidrug-resistant and extensively drug-resistant tuberculosis. Lancet Infect Dis. 2010; 10:621–629.
43. Koh WJ, Lee SH, Kang YA, Lee CH, Choi JC, Lee JH, et al. Comparison of levofloxacin versus moxifloxacin for multidrug-resistant tuberculosis. Am J Respir Crit Care Med. 2013; 188:858–864.
44. Larsen MH, Vilcheze C, Kremer L, Besra GS, Parsons L, Salfinger M, et al. Overexpression of inhA, but not kasA, confers resistance to isoniazid and ethionamide in Mycobacterium smegmatis, M. bovis BCG and M. tuberculosis. Mol Microbiol. 2002; 46:453–466.
45. Chang KC, Yew WW, Tam CM, Leung CC. WHO group 5 drugs and difficult multidrug-resistant tuberculosis: a systematic review with cohort analysis and meta-analysis. Antimicrob Agents Chemother. 2013; 57:4097–4104.
46. Tang S, Yao L, Hao X, Liu Y, Zeng L, Liu G, et al. Clofazimine for the treatment of multidrug-resistant tuberculosis: prospective, multicenter, randomized controlled study in china. Clin Infect Dis. 2015; 60:1361–1367.
47. Bastos ML, Hussain H, Weyer K, Garcia-Garcia L, Leimane V, Leung CC, et al. Treatment outcomes of patients with multidrug-resistant and extensively drug-resistant tuberculosis according to drug susceptibility testing to first- and second-line drugs: an individual patient data meta-analysis. Clin Infect Dis. 2014; 59:1364–1374.
48. Falzon D, Gandhi N, Migliori GB, Sotgiu G, Cox HS, Holtz TH, et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur Respir J. 2013; 42:156–168.
49. Jacobson KR, Tierney DB, Jeon CY, Mitnick CD, Murray MB. Treatment outcomes among patients with extensively drug-resistant tuberculosis: systematic review and meta-analysis. Clin Infect Dis. 2010; 51:6–14.
50. Lee M, Lee J, Carroll MW, Choi H, Min S, Song T, et al. Linezolid for treatment of chronic extensively drug-resistant tuberculosis. N Engl J Med. 2012; 367:1508–1518.
51. Tang S, Yao L, Hao X, Zhang X, Liu G, Liu X, et al. Efficacy, safety and tolerability of linezolid for the treatment of XDR-TB: a study in China. Eur Respir J. 2015; 45:161–170.
52. Diacon AH, Pym A, Grobusch MP, de los Rios JM, Gotuzzo E, Vasilyeva I, et al. Multidrug-resistant tuberculosis and culture conversion with bedaquiline. N Engl J Med. 2014; 371:723–732.
53. Guglielmetti L, Le Du D, Jachym M, Henry B, Martin D, Caumes E, et al. Compassionate use of bedaquiline for the treatment of multidrug-resistant and extensively drug-resistant tuberculosis: interim analysis of a French cohort. Clin Infect Dis. 2015; 60:188–194.
54. Skripconoka V, Danilovits M, Pehme L, Tomson T, Skenders G, Kummik T, et al. Delamanid improves outcomes and reduces mortality in multidrug-resistant tuberculosis. Eur Respir J. 2013; 41:1393–1400.
55. Diacon AH, Dawson R, von Groote-Bidlingmaier F, Symons G, Venter A, Donald PR, et al. 14-day bactericidal activity of PA-824, bedaquiline, pyrazinamide, and moxifloxacin combinations: a randomised trial. Lancet. 2012; 380:986–993.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download