Abstract
Empyema necessitatis is a rare complication of an empyema. Although the incidence is thought to be decreased in the post-antibiotic era, immunocompromised patients such as patients with chronic kidney disease on dialysis are still at a higher risk. A 56-year-old woman on peritoneal dialysis presented with an enlarging mass on the right anterior chest wall. The chest computed tomography scan revealed an empyema necessitatis and the histopathologic findings revealed a granulomatous inflammation with caseation necrosis. The patient was treated with anti-tuberculous medication.
Empyema necessitatis is an abscess on the thoracic wall by extension of purulent pleural liquid through adjacent tissues1. Tuberculous empyema necessitatis is a rare complication of tuberculosis. However, immunocompromised patients such as patients with chronic kidney disease on dialysis are at a higher risk1,2.
Herein, we present a case of tuberculous empyema necessitatis in a patient with chronic kidney disease on peritoneal dialysis.
A 56-year-old woman presented with an enlarging soft mass on right anterior chest wall with pain lasting for 2 months. There were no symptoms of fever, dyspnea, or cough. She denied recent chest trauma or exposure to tuberculosis. She was diagnosed with chronic kidney disease seven years ago and has been on peritoneal dialysis for four years. Her medical history was remarkable of hypertension, diabetes mellitus and hypothyroidism on medication. Vital signs on admission were blood pressure 134/68 mm Hg, temperature 36.9℃, pulse rate 95 beats per minute, and respiratory rate 20 breaths per minute. Physical examination revealed a pink erythematous, cold, soft, tender, subcutaneous mass of 6×3 cm on the right chest wall between the fifth and seventh ribs (Figure 1).
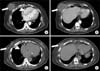
Laboratory values revealed a white blood cell count of 17,270/mm3 with 89.8% neutrophils. Hemoglobin was 7.2 g/dL and platelets were 416,000/mm3. Blood urea nitrogen was 47.7 mg/dL, creatinine was 8.15 mg/dL, sodium was 133 mEq/L and potassium was 3.7 mEq/L. Liver function tests were within normal limits and C-reactive protein was 72.4 mg/L. Chest X-ray revealed pleural thickening in the right lung (Figure 2). Computed tomography (CT) scan of the chest revealed calcified pleural thickening with loculated fluid collection in the right lower anterior hemithorax suggestive of empyema, with multiple cystic extrapleural masses in the right anterior chest wall consistent with empyema necessitatis (Figure 3).
Fine needle aspiration biopsy (FNAB) was performed for diagnosis. The mass was filled with pus-like materials and histopathologic findings revealed granulomatous inflammation with caseation necrosis (Figure 4). Polymerase chain reaction for Mycobacterium tuberculosis was positive.
The patient was diagnosed with tuberculous empyema with tuberculous empyema necessitatis. An anti-tuberculous medication was started (with dose adjustment for chronic kidney disease; isoniazid 400 mg per day, rifampin 600 mg per day, pyrazinamide 1,500 mg 3 times per week, ethambutol 800 mg three times per week). No surgical intervention was made to the chest wall. After 5 months, CT scan revealed reduced size of the multiple cystic extrapleural masses (Figure 3) and anti-tuberculous medication was continued.
Empyema necessitatis is a collection of inflammatory tissue that usually extends directly from the pleural cavity into the thoracic wall, forming a mass in the extrapleural soft tissues of the chest1. It is characterized by the extension of suppuration from the pleural space, typically through the thoracic wall, forming subcutaneous abscess. Clinically, patients show symptoms of enlarging, tender, erythematous mass, cough, chest pain and dyspnea3. The most common site is the anterior chest wall between the midclavicular and anterior axillary line and between the second and sixth intercostal spaces4. Less commonly, it can involve the bronchus, vertebral column, diaphragm, breast, mediastinum, retroperitoneum, esophagus, pericardium, flank or groin5. It was first described in 1640 by Baillon, who reported a woman with left sided pulsating tumor associated with pleurisy. The most common etiology is Mycobacterium tuberculosis and cases of Actinomycosis species, Streptococcus pneumonia, Staphylococcus aureus, Blastomycosis species, and neoplasms have been reported. Three reports have reviewed cases of empyema necessitatis. In 1940, Sindel4 reviewed 115 cases. Mycobacterium tuberculosis was the most common etiology with 84 (73%) cases. In 2004, Freeman et al.5 reviewed 26 cases from 1966 to 2004 and 13 (50%) cases was caused by Mycobacterium tuberculosis. Recently, in 2010, Llamas-Velasco et al.3 reviewed 20 cases from 2004 and Mycobacterium tuberculosis was less common (7 cases, 35%) than the previous reports but still the most common infectious agent. There were no data concerning the prevalence of chronic kidney disease or patients on dialysis in these reports.
Empyema necessitatis is thought as an unusual complication of empyema with decreasing incidence, while most of its patients were described in the preantibiotic era. However, immunocompromised patients including patients with chronic kidney disease on dialysis are at a higher risk of empyema necessitatis1,2. Cellular and humoral immunity are both reduced in patients with chronic kidney disease on dialysis and risk of tuberculosis infection is 6.9- to 62.5-fold higher than the general population6. Additionally, extra pulmonary involvements are more frequent than isolated pulmonary disease in these patients, leading to delayed diagnosis7.
Mortality is significantly decreasing with antibiotic therapy, from 66% in the preantibiotic era to less than 5% nowadays3,4. Mortality from recent cases were also associated with reduced immune defence such as old age8, neoplastic9, or cystic fibrosis10. Although there has been no recent case of mortality reported with patients on dialysis, higher mortality is expected.
The differential diagnosis of empyema necessitatis includes neoplasms, Wegener's granulomatosis, sarcoidosis, infective endocarditis and septic embolization11. CT scan and biopsy are important for accurate diagnosis. CT is helpful in detection and characterization of empyema necessitatis while tissue and fluid for cytological diagnosis and culture can be aspirated by FNAB12,13.
Treatment of empyema necessitatis includes antimicrobial therapy and surgical drainage. While standard antituberculosis regimen can be used for treatment14, dose adjustments for patients with chronic kidney disease are necessary.
In summary, empyema necessitatis should be considered in any patient with an enlarging soft tissue mass on the chest wall especially in immunocompromised patients such as patients with chronic renal failure on dialysis, even though history or symptoms of infection are absent. Early diagnosis and proper management can be associated with the best outcome.
Figures and Tables
Figure 1
Skin lesions. Pink erythematous, cold, soft, tender subcutaneous mass of 6×3 cm size are noted on the right chest wall between the fifth and seventh ribs.

Figure 3
(A, B) On admission, the chest computed tomography (CT) reveals a calcified pleural thickening with loculated fluid collection in the right lower anterior hemithorax (arrowhead) and with multiple cystic extrapleural masses in right anterior chest wall (arrows). (C, D) After 5 months of therapy, the chest CT reveals a reduced loculated fluid collection in the right lower anterior hemithorax (arrowhead) and a reduced size of the multiple cystic extrapleural masses in the right anterior chest wall (arrows).
References
1. Jover F, Andreu L, Cuadrado JM, Montagud J, Merino J. Tuberculous empyema necessitatis in a man infected with the human immunodeficiency virus. South Med J. 2002; 95:751–752.
2. Aylk S, Qakan A, Aslankara N, Ozsoz A. Tuberculous abscess on the chest wall. Monaldi Arch Chest Dis. 2009; 71:39–42.
3. Llamas-Velasco M, Dominguez I, Ovejero E, Perez-Gala S, Garcia-Diez A. Empyema necessitatis revisited. Eur J Dermatol. 2010; 20:115–119.
4. Sindel EA. Empyema necessitates. Q Bull Sea View Hosp. 1940; 6:1–49.
5. Freeman AF, Ben-Ami T, Shulman ST. Streptococcus pneumoniae empyema necessitatis. Pediatr Infect Dis J. 2004; 23:177–179.
6. Hussein MM, Mooij JM, Roujouleh H. Tuberculosis and chronic renal disease. Semin Dial. 2003; 16:38–44.
7. el-Shahawy MA, Gadallah MF, Campese VM. Tuberculosis of the spine (Pott's disease) in patients with end-stage renal disease. Am J Nephrol. 1994; 14:55–59.
8. Akgul AG, Orki A, Orki T, Yuksel M, Arman B. Approach to empyema necessitatis. World J Surg. 2011; 35:981–984.
9. Reyes CV. Cutaneous tumefaction in empyema necessitatis. Int J Dermatol. 2007; 46:1294–1297.
10. Noyes BE, Michaels MG, Kurland G, Armitage JM, Orenstein DM. Pseudomonas cepacia empyema necessitatis after lung transplantation in two patients with cystic fibrosis. Chest. 1994; 105:1888–1891.
11. Tonna I, Conlon CP, Davies RJ. A case of empyema necessitatis. Eur J Intern Med. 2007; 18:441–442.
12. Reyes CV, Thompson KS, Jensen J. Fine needle aspiration biopsy of mastitis secondary to empyema necessitatis: a report of two cases. Acta Cytol. 1999; 43:873–876.
13. Glicklich M, Mendelson DS, Gendal ES, Teirstein AS. Tuberculous empyema necessitatis. Computed tomography findings. Clin Imaging. 1990; 14:23–25.
14. Chaiyasate K, Hramiec J. Images in clinical medicine. Tuberculosis empyema necessitatis. N Engl J Med. 2005; 352:e8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download