Abstract
Background
Transbronchial lung biopsy (TBLB) is a valuable diagnostic tool for peripheral pulmonary lesions. The diagnostic yield of TBLB reportedly ranges from 41%-60%. Many studies demonstrated the various factors that influence the yield of TBLB, including size, location, and distance from the carina or pleura. However, no study has evaluated the effects of the bronchoscope diameter. We evaluated whether the bronchoscope diameter affected the diagnostic yield of TBLB.
Methods
We reviewed records from 178 patients who underwent TBLB using bronchoscopes of two different diameters (5.7 mm, thick outer diameter, Olympus BF-200; 4.9 mm, thin, BF-260). The fluoroscopic guidance rates, yield of TBLB and flexible bronchoscopy (FB) were compared between the two groups. Additionally, we compared the results of the procedures with respect to diagnosis, distance from the pleura, and size of the lesion.
Results
The results of fluoroscopic guidance, TBLB, and FB yield using thin diameter bronchoscope were significantly better than those obtained with a thick diameter bronchoscope (p=0.021, p=0.036, and p=0.010, respectively). Particularly, when the distance from the pleura was ≤ 10 mm, success rates for fluoroscopic guidance and FB with thin bronchoscope were higher (p=0.013 and p=0.033, respectively), as compared to with thick bronchoscope.
Transbronchial lung biopsy (TBLB) is a safe and valuable diagnostic tool in patients with pulmonary nodules or masses seen on chest radiography that are not visible on bronchoscopy. Results of TBLB were first reported in 1974 by Levin et al.1 Since the late 1970s, the reported diagnostic yield of TBLB has ranged from 41% to 69%2,3,4,5,6,7,8,9,10,11,12, and has been shown to be affected by many factors including size, location, border characteristics of the lesion, and distance from the hilum or carina5,6,7,8,9,10,11,12,13,14. Most studies have shown that lesion size is the most important factor influencing diagnostic yield, though lobar location and distance from the hilum can significantly influence results as well. However, there have not been any studies to date that have evaluated the effects of bronchoscope diameter. In this study, we evaluated whether bronchoscope diameter affects the diagnostic yield of TBLB.
We retrospectively reviewed the medical records of patients that underwent TBLB between February 2002 and January 2005 at a University Hospital. A total of 187 patients who met the following inclusion criteria were enrolled in this study: 1) presence of pulmonary nodules or masses surrounded by normal lung tissue or pleura; 2) lesions that were not visible endoscopically; 3) lesions measuring 6 cm or less at the greatest diameter on chest computed tomography (CT); 4) availability of chest radiographs and chest CT images; and 5) who underwent fluoroscopically-guided TBLB with one of two types of bronchoscopes, BF-260 (Olympus, Tokyo, Japan) or BF-200 (Olympus). Our study was approved by the institutional review board of our institute.
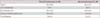
All bronchoscopy procedures were performed by pulmonary physicians who had the experience of bronchoscopy more than 2 years. One of two types of bronchoscope with different diameters was used for all procedures using a same video bronchoscopy system. The outer diameters of the bronchoscopes were 5.7 mm for the BF-200, thick bronchoscope and 4.9 mm for the BF-260, thin bronchoscope. All other functions of the bronchoscopes were identical, as shown in Table 1. All procedures were performed via the transnasal or oral route under local anesthesia. Oxygen was administered via nasal cannula at 2 L/min flow and was increased as needed to keep SpO2 above 90% as measured on continuous pulse oximetry monitoring. Atropine 0.5 mg was administered intramuscularly, and midazolam 0.07 mg/kg intravenously was used when needed to achieve adequate sedation prior to the procedure. The patient's oropharynx was sprayed with topical lidocaine (2%). Both bronchoscopes were introduced up to the 4th-5th generations of segmental bronchi. Once the bronchoscope was advanced beyond the vocal cords, secretions were collected using the suction channel into a trap, and were subsequently labeled as bronchial washings. Additional washings were obtained from the involved lobar segment. Biplane fluoroscopy was used for guidance of TBLB. If the biopsy forceps appeared to reach the lesion under fluoroscopy, fluoroscopic guidance was considered successful. If the lung lesion could not be reached by the forceps or visualized under fluoroscopy, fluoroscopic guidance was considered unsuccessful. The combined yield of TBLB and bronchial washings was defined as the yield of flexible bronchoscopy.
Patients who were not diagnosed by flexible bronchoscopy were performed another pathologic diagnostic methods (e.g., transthoracic needle aspiration or thoracoscopic biopsy) or followed until a diagnosis was confirmed. Pathologic diagnoses were established using bronchoscopic procedures such as TBLB, transbronchial needle aspiration (TBNA), bronchial washings or other techniques including CT-guided transthoracic needle biopsy and thoracotomy. In cases of benign disease, a pathologic diagnosis was not essential. A pathologic finding of acute inflammation or organizing pneumonia was considered diagnostic if the final tissue diagnosis came back as pneumonia or if the lesion disappeared after a course of antibiotics. A pathologic finding of caseating granuloma or a positive Ziehl-Neelsen stain was considered diagnostic for tuberculoma. A histologic diagnosis of nonspecific fibrosis such as anthracofibrosis and chronic inflammation was considered non-diagnostic, even if the final diagnosis was benign disease. The appearance of the lesions was analyzed retrospectively by a single radiologist. Size, location, and distance from the pleura were determined from the CT images. The greatest diameter of the lesion was used to define size. The distance from the pleura was measured in a straight line from the pleura to the peripheral edge of the lesion.
Severe bleeding as a complication associated with the procedure was considered when it required the examiner to prematurely abort the procedure or when topical epinephrine was needed for hemostasis. In all patients, chest radiography was done after the procedure to rule out pneumothorax.
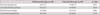
A total of 178 patients fulfilled the inclusion criteria and were enrolled in this study (thick bronchoscope, 88 patients; thin bronchoscope, 90 patients). The mean ages were 62.3 years and 61.2 years in the thick (thick BG) and thin bronchoscope groups (thin BG), respectively. There were no significant differences between groups in the size of the lesions, distance from the pleura, and number of patients undergoing biopsy (Table 2).
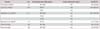
Of the 88 patients in the thick BG, 42 (47.7%) were diagnosed with malignant lesion and 38 (43.2%) were with benign lesion (Table 3). Of the 90 patients in the thin BG, malignancy was confirmed in 33 patients (36.7%), and benign disease was in 54 patients (60.0%). Adenocarcinoma was the most common malignancy, while tuberculoma was the most commonly diagnosed benign lesion among two groups.
A diagnosis was established by TBLB only in 93 patients (52.2%). Of the remaining 85 patients in whom TBLB failed, 36 patients received a diagnosis using CT-guided transthoracic needle biopsy and 18 patients had positive findings on bronchial washings. In seven patients, we established a diagnosis by thoracotomy. In four patients, pleural fluid cytology was positive for malignancy. Additionally, TBNAs of subcarinal and paratracheal nodes were performed in seven patients. The results of TBNA in two patients were reported as non-small cell carcinoma, which were not assumed the yield of flexible bronchoscopy. In nine patients, the appearance of the lesion on chest radiography remained stable for 2 years, and as a result was designated as benign. In 11 patients (eight patients in the thick BG; three patients in the thin BG), a final diagnosis could not be established due to insufficient follow-up.
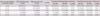
Table 4 illustrates the effects of the diameter of the bronchoscopes on the diagnostic yield. The rate of fluoroscopic guidance, diagnostic yield of TBLB, and TBLB with bronchial washings were significantly higher in thin BG than thick BG (p=0.021, p=0.036, and p=0.002, respectively). We also investigated whether the distance from the pleura affects the diagnostic yields of TBLB or fluoroscopic guidance (Table 5). In cases with less than 10 mm of the distance from the pleura, the rate of fluoroscopic guidance and diagnostic yields of TBLB with bronchial washings were higher in thin BG than thick BG (p=0.013 and p=0.033, respectively). However, when the distance from the pleura was greater than 10 mm, there were no significant differences between the two groups.
The sizes of the lesions were divided into four size criteria (criterion 1, ≤2 cm; criterion 2, 2-3 cm; criterion 3, 3-4 cm; and criterion 4, 4-6 cm). In the thick BG, the diagnostic yields of TBLB were 42.9% in criterion 1, 60.9% in criterion 2, 37.9% in criterion 3, and 33.3% in criterion 4. In the thin BG, the diagnostic yields of TBLB were 58.3%, 75.0%, 57.1%, and 52.0%, respectively. In the thin BG, the diagnostic yields of TBLB tended to be higher in size matched comparison with the thick BG (p=0.300, p=0.324, p=0.179, and p=0.251, respectively).
We identified the locations of the lesions not only with respect to distance from the pleura, but also by lobar location. There were no significant differences in the yield of TBLB according to lobar location between the two groups. The overall yields of different locations were as follows: right upper lobe, 30.3%; left upper lobe, 45.3%; right lower lobe, 23.0%; left lower lobe, 14.6%; and right middle lobe, 6.7%.
Bleeding associated with TBLB occurred in 38 patients, though none required invasive treatment for hemostasis. There was one case of pneumothorax after biopsy, which completely resolved after high O2 therapy for 4 days. There were no other significant complications such as hemoptysis or pneumonia, and none of the patients required admission to the intensive care unit.
This study showed that use of a bronchoscope with a smaller diameter increased the diagnostic yield of fluoroscopic guidance, TBLB, and TBLB with bronchial washings. Interestingly, when the lesion was peripherally located in 10 mm or less from pleura, the yields of fluoroscopic guidance and TBLB with bronchial washings using the thin bronchoscope were better than those of the thick one. These results suggest that a thinner bronchoscope is more useful when approaching peripheral lesions.
Previous studies have shown that the most important determinant of diagnostic accuracy is the size of the lesion. Some studies have reported a direct correlation between the size of the lesion and the diagnostic yield of flexible bronchoscopy5,6,7,14,15. However, there was no direct correlation in our data. Interestingly, we did find that the best results were typically obtained from lesions 2 to 3 cm in diameter. The overall success rate of TBLB was 52.2% (93/178) and rates according to the size of the lesion were as follows: lesions≤2 cm, 51.0%; lesions 2 to 3 cm, 67.4%; lesions 3 to 4 cm, 46.0%; and lesions 4 to 6 cm, 45.0%. The overall success rate of TBLB combined the results of bronchial washing was 67.4% (120/178) and rates according to the size of the lesion were 62.2%, 83.7%, 62.0%, and 62.5%, respectively. Our results may differ from those of previous studies due to differences in study design. Previous studies by Wallace and Deutsch9, Torrington and Kern13, and Radke et al.7 did not exclude patients with endobronchial lesions, which in turn affected their calculated yields. In studies conducted by Baaklini et al.6 and Chechani5, there was no upper limit for the size of the lesions, and thus their reported diagnostic yield for flexible bronchoscopy was greater than 90% for lesions≥6 cm. In our study, the diagnostic yield of lesions 6 cm or larger which were excluded from our results was 87.5% (data not shown). In addition, we excluded five patients who underwent both TBLB and bronchoscopic biopsy for visible endobronchial lesions. Therefore the inclusion criteria in our study were different from those in other studies which included the larger size of lesions and visible endobronchial lesions. Table 6 shows the calculated diagnostic yields for flexible bronchoscopy from several studies after exclusion of endobronchial lesions and lesions>4 cm in diameter. Recently, several studies demonstrated that ultrathin bronchoscopy had a role as a useful adjunct to standard bronchoscopic techniques in diagnosing of peripheral lung lesions16,17. They used the ultrathin bronchoscope which had the external diameter of 3.6 mm and revealed the diagnostic yield of 64.7%16. We found that the outer diameter of the bronchoscope contributed to the yield of flexible bronchoscopy.
Diagnostic yield is also affected by diagnosis. Baaklini et al.6 reported results of TBLBs according to diagnosis and had a higher diagnostic yield for malignant lesions (85/150, 57%) compared to benign lesions (6/26, 23%). Radke et al.7 reported a 63% yield for flexible bronchoscopy in cases of malignant lesions, and 38% in cases of benign lesions. Chechani5 reported similar results, with a yield of 80% for malignant and 50% for benign lesions. We had overall diagnostic yields for malignant and benign disease in this study (67.7% in malignant lesions, 62.4% in benign lesions). The diagnostic yield in benign lesions was higher than previous studies because a large number of tuberculomas was included in our studies. Pulmonary tuberculosis is known to be endemic in Korea, with a prevalence of 90 per 100,000 people, which is higher than the standard set by the World Health Organization. In this study, 46 patients (25.8%) with tuberculomas were enrolled. The success rates for TBLB and TBLB with bronchial washings for diagnosing tuberculoma were 63% (29/46) and 80% (37/46), respectively. Lai et al.15 reported a high yield for flexible bronchoscopy (22/40, 55%) for pulmonary tuberculomas in their study. Of those patients, 15 were diagnosed by TBLB and seven by bronchial washings only.
It has been debated whether the additional yield of bronchial washings justifies the cost of the procedure. Fletcher and Levin8 found that bronchial washings were positive in only 2 out of 54 bronchoscopies (4%), while de Gracia et al.10 found that bronchial washings were positive in 7 out of 35 cases (20%). Chechani5 reported that bronchial washings were never positive as a stand-alone specimen in their study. On the other hand, Baaklini et al.6 reported the high accuracy of bronchial washings (71/177, 40%). In our study, of the 85 patients in whom TBLB was unsuccessful, 18 patients (21.2%) received a diagnosis using bronchial washings. We propose that bronchial washings after biopsy have an additive effect to obtain cytologic samples detached malignant cells or microorganisms from pulmonary nodules or masses. This study demonstrated that stepwise performance of bronchial washings with TBLB increased the diagnostic yield of bronchoscopy.
Bleeding occurred in all patients that underwent TBLB and was controlled with local application of epinephrine. However, there was no significant bleeding that required invasive treatments, it suggested that TBLB is relatively safe procedure.
Limitations of this study include it being a single institute setting and a retrospective study design. As a consequence, the results from this study may not be generalizable to other institutions. This retrospective study was not able to completely remove the confounding variables and was not randomized. However, it could be analyzable because there were no differences between groups in clinical characteristics of subjects and characteristics of bronchoscopes were same excepting outer diameters of those.
In conclusion, this study retrospectively evaluated the effects of bronchoscope diameters on the yield of TBLB. Using of a thinner bronchoscope may increase the diagnostic yield of fluoroscopic guidance, TBLB, and TBLB with bronchial washings and be more useful when approaching peripheral pulmonary lesions.
Figures and Tables
Table 3
Diagnostic outcomes for 178 patients who underwent transbronchial lung biopsy for pulmonary nodules or masses

References
1. Levin DC, Wicks AB, Ellis JH Jr. Transbronchial lung biopsy via the fiberoptic bronchoscope. Am Rev Respir Dis. 1974; 110:4–12.
2. Andersen HA. Transbronchial lung biopsy in diffuse pulmonary disease. Ann Thorac Surg. 1977; 24:1.
3. Ellis JH Jr. Transbronchial lung biopsy via the fiberoptic bronchoscope: experience with 107 consecutive cases and comparison with bronchial brushing. Chest. 1975; 68:524–532.
4. Zavala DC. Diagnostic fiberoptic bronchoscopy: techniques and results of biopsy in 600 patients. Chest. 1975; 68:12–19.
5. Chechani V. Bronchoscopic diagnosis of solitary pulmonary nodules and lung masses in the absence of endobronchial abnormality. Chest. 1996; 109:620–625.
6. Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest. 2000; 117:1049–1054.
7. Radke JR, Conway WA, Eyler WR, Kvale PA. Diagnostic accuracy in peripheral lung lesions. Factors predicting success with flexible fiberoptic bronchoscopy. Chest. 1979; 76:176–179.
8. Fletcher EC, Levin DC. Flexible fiberoptic bronchoscopy and fluoroscopically guided transbronchial biopsy in the management of solitary pulmonary nodules. West J Med. 1982; 136:477–483.
9. Wallace JM, Deutsch AL. Flexible fiberoptic bronchoscopy and percutaneous needle lung aspiration for evaluating the solitary pulmonary nodule. Chest. 1982; 81:665–671.
10. de Gracia J, Bravo C, Miravitlles M, Tallada N, Orriols R, Bellmunt J, et al. Diagnostic value of bronchoalveolar lavage in peripheral lung cancer. Am Rev Respir Dis. 1993; 147:649–652.
11. Shiner RJ, Rosenman J, Katz I, Reichart N, Hershko E, Yellin A. Bronchoscopic evaluation of peripheral lung tumours. Thorax. 1988; 43:887–889.
12. Stringfield JT, Markowitz DJ, Bentz RR, Welch MH, Weg JG. The effect of tumor size and location on diagnosis by fiberoptic bronchoscopy. Chest. 1977; 72:474–476.
13. Torrington KG, Kern JD. The utility of fiberoptic bronchoscopy in the evaluation of the solitary pulmonary nodule. Chest. 1993; 104:1021–1024.
14. Cortese DA, McDougall JC. Biopsy and brushing of peripheral lung cancer with fluoroscopic guidance. Chest. 1979; 75:141–145.
15. Lai RS, Lee SS, Ting YM, Wang HC, Lin CC, Lu JY. Diagnostic value of transbronchial lung biopsy under fluoroscopic guidance in solitary pulmonary nodule in an endemic area of tuberculosis. Respir Med. 1996; 90:139–143.
16. Rooney CP, Wolf K, McLennan G. Ultrathin bronchoscopy as an adjunct to standard bronchoscopy in the diagnosis of peripheral lung lesions: a preliminary report. Respiration. 2002; 69:63–68.
17. Bose S, Ghatol A, Eberlein M, Yung RC. Ultrathin bronchoscopy in the diagnosis of peripheral cavitary lung lesions. J Bronchology Interv Pulmonol. 2013; 20:167–170.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download