Abstract
Background
Information regarding prognostic value of growth differentiation factor 15 (GDF-15) and heart-type fatty acid-binding protein (H-FABP) in patients with chronic obstructive pulmonary disease (COPD) exacerbation is limited. The aim of this study was to investigate whether serum levels of GDF-15 and H-FABP predict an adverse outcome for COPD exacerbation.
Methods
Clinical variables, including serum GDF-15 and H-FABP levels were compared in prospectively enrolled patients with COPD exacerbation that did or did not experience an adverse outcome. An adverse outcome included 30-day mortality and need for endotracheal intubation or inotropic support.
Results
Ninety-seven patients were included and allocated into an adverse outcome (n=10) or a control (n=87) group. Frequencies of mental change and PaCO2>37 mm Hg were significantly higher in the adverse outcome group (mental change: 30% vs. 6%, p=0.034 and PaCO2>37 mm Hg: 80% vs. 22%, p<0.001, respectively). Serum GDF-15 elevation (>1,600 pg/mL) was more common in the adverse outcome group (80% vs. 43%, p=0.041). However, serum H-FABP level and frequency of serum H-FABP elevation (>755 pg/mL) did not differ between the two groups. Multivariate analysis showed that an elevated serum GDF-15 and PaCO2>37 mm Hg were significant predictors of an adverse outcome (odds ratio [OR], 25.8; 95% confidence interval [CI], 2.7-243.8; p=0.005 and OR, 11.8; 95% CI, 1.2-115.3; p=0.034, respectively).
Chronic obstructive pulmonary disease (COPD) is expected to be the third leading cause of death in 20201. COPD exacerbation determines disease-associated morbidity and mortality2, and short-term and long-term mortalities are known to increase after COPD exacerbation3,4. Many factors have been reported to be associated with short-or long-term mortality in affected patients5, and because prognostic factors are helpful, attempts to identify new predictors are still required. Several blood biomarkers, including N-terminal-pro-B-type natriuretic peptide (NT-proBNP), troponin I or T, C-reactive protein (CRP), and procalcitonin have been proposed as prognostic factors of short-term outcome in patients with COPD exacerbation6,7,8,9. Among these, NT-proBNP and troponin T elevations are strong independent predictors of early mortality, but the pathophysiological bases of these relationships are unknown7.
Growth differentiation factor 15 (GDF-15) is a member of the transforming growth factor-β superfamily of cytokines, and plays important roles in cell growth and differentiation10. Under normal conditions, GDF-15 is weakly expressed in most tissues11. However, circulating levels of GDF-15 are elevated in acute coronary syndrome12,13, chronic heart failure14, acute pulmonary embolism15, and idiopathic pulmonary arterial hypertension16. These results suggest that blood GDF-15 levels increase in response to right ventricular (RV) or left ventricular (LV) overload. On the other hand, heart-type fatty acid-binding protein (H-FABP) plays a pivotal role in myocardial homeostasis, because this small cytoplasmic protein facilitates the intracellular transport of insoluble fatty acids in myocardium, in which energy is mainly provided by lipid oxidation17,18. H-FABP can be released by myocardial injury, such as acute coronary syndrome19, and may be elevated by RV stress, such as that caused by pulmonary embolism20,21,22. Therefore, H-FABP is a candidate biomarker of right and left cardiac dysfunction. However, no data are available on the prognostic values of GDF-15 and H-FABP in patients with COPD exacerbation.
We hypothesized elevated serum levels of GDF-15 and H-FABP might provide prognostic information in patients with COPD exacerbation. Thus, the aims of this study were to determine whether elevated serum levels of GDF-15 and H-FABP predict an adverse outcome in these patients.
Between April 2011 and April 2013, all patients hospitalized with COPD exacerbation at Kyungpook National University Hospital (KNUH), a tertiary referral center in Daegu, South Korea, were enrolled prospectively. The Institutional Review Board of the KNUH approved the study protocol, and informed consent was obtained from all participants. COPD was diagnosed based on available spirometric and medical records as recommended by the Global Initiative for Chronic Obstructive Lung Diseases (GOLD)23. COPD exacerbation was defined as acute deterioration requiring hospitalization from a stable condition24. On arrival at the hospital, emergency or internal medicine department physicians evaluated patients by history taking, physical examination, chest radiography, and routine laboratory tests. Patients with any specific causes identified during these examinations, including pneumonia, pneumothorax, and congestive heart failure, were excluded. After exclusions, all patients underwent computed tomography (CT) within 24 hours of admission. Patients with azotemia (serum creatinine>1.5 mg/dL) or exhibiting hypersensitivity to contrast media were excluded. As described in a previous study25, the etiologies of COPD exacerbations were determined as follows: 1) pneumonia was diagnosed when consolidation or ground-glass opacity (GGO) was observed by CT; 2) tracheobronchitis if symptoms suggestive of a respiratory infection, including increased sputum, purulent sputum, fever, or upper respiratory infection symptoms, were identified without consolidation or GGO by CT or if centrilobular nodules or a tree-in-bud pattern were observed on CT images, without consolidation or GGO; 3) congestive heart failure was diagnosed when CT findings indicated pulmonary edema with echocardiographic left LV dysfunction; 4) pulmonary embolism when a sharply delineated pulmonary arterial filling defect was located centrally within a vessel or made an acute angles at its interface with the vessel wall in at least two consecutive CT sections; and 5) undetermined etiology.
The 97 patients were allocated to two groups, that is, to an adverse outcome group (n=10) or to a control group (n=87). An adverse outcome was defined as a composite end point of 30-day mortality or the need for endotracheal intubation or inotropic support.
Baseline and clinical characteristics of the patients, including age, gender, smoking history, body mass index, comorbid conditions, and respiratory infection symptoms, were checked. Dyspnea was assessed using modified Medical Research Council (mMRC) grades26. For severity of COPD exacerbation, BAP-65 classes 27 were defined as follows: class I, patients≤65 years of age without any risk factors (blood urea nitrogen [BUN] level≥25 mg/dL, altered mental status, or pulse≥109 beats/min); class II, patients>65 years of age with no risk factor; and class III, IV, and V, patients with one, two, and three risk factors, respectively. Lengths of hospital stay were also recorded.
Pulmonary function testing (PFT) was performed as recommended by the American Thoracic Society and European Respiratory Society Guideline28. PFT data obtained within 6 months of index admission dates were used in the analysis.
Blood tests included white blood cell count, erythrocyte sedimentation rate (ESR), CRP, procalcitonin, NT-proBNP, troponin I, BUN, sodium, and albumin levels. Arterial blood gas analysis data, including partial oxygen pressure in arterial blood (PaO2), partial carbon dioxide pressure in arterial blood (PaCO2), inspired oxygen fraction (FiO2), PaO2/FiO2 ratio, and alveolar-arterial oxygen gradient (P[A-a]O2), were also checked.
Blood samples were obtained within 24 hours of arrival, centrifuged immediately, and stored at -80℃. Serum samples were registered and later provided by the National Biobank of Korea at the KNUH. Serum GDF-14 and H-FABP levels were measured using commercially available ELISA kits (Human GDF-15 Immunoassay; Quantikine, Minneapolis, MN, USA and Human H-FABP; Hycult Biotech, Uden, The Netherlands) according to the manufacturers' protocols.
Only 69 patients underwent echocardiography, because of operator non-availability. Transthoracic echocardiographic findings including the presence of RV dysfunction and RV systolic pressure (RVSP) were reviewed. RV dysfunction was echocardiographically defined as RV free wall hypokinesia, and RVSP was calculated using the tricuspid regurgitation flow velocity measured by Doppler echocardiography29. LV ejection fraction (LVEF) was determined by the Simpson biplane formula30.
CT scans were performed using a multidetector CT with 16 or 64 detector rows: Light Speed 16 (General Electric, Milwaukee, WI, USA) or Aquilion 64 (Toshiba Medical Systems, Tokyo, Japan). CT scans were reviewed by two radiologists (K-.M.S. and J.L.), and diagnoses were made by consensus. The presences of consolidation or GGO, bronchiolitis (centrilobular nodules or tree-in-bud pattern), bronchiectasis, bronchial wall thickening, and emphysema were checked. CT findings were defined as follows: consolidation as airspace opacification with obscuration of the underlying vasculature; GGO as mildly increased attenuation without obscuration of the underlying vasculature; tree-in-bud pattern as centrilobular nodules with either V- or Y-shaped branching linear opacities; bronchiectasis when bronchial internal diameter was greater than that of the adjacent pulmonary artery (PA); and bronchial anthracofibrosis as multiple smooth bronchial narrowing with adjacent calcified lymph nodes; bronchial wall thickening was assessed subjectively. As has been performed in previous studies31,32, diameters of main PA and ascending aorta (AA) at the level of the PA bifurcation were measured in order to obtain PA sizes and PA/AA diameter ratios. As in a previous study33, a PA/AA diameter ratio of >1 was selected as the cutoff value for pulmonary hypertension.
Statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Results are expressed as medians with ranges (interquartile range [IQR]) for continuous variables and numbers with percentages for categorical variables. The Mann-Whitney U test was used to compare continuous variables, whereas the chi-squared test or Fisher exact test was used to compare categorical variables. When continuous variables were converted to categorical variables, cut-off values were determined using receiver operating characteristic curves. To identify predictors of adverse outcomes, backward stepwise multiple logistic regression analysis was used using variables of p<0.1 in univariate analysis. A goodness-of-fit test used to assess the fit of logistic regression models was the Hosmer-Lemeshow test. Statistical significance was accepted for p<0.05.
Initially, 103 patients were enrolled. However, after reviewing CT scans, 6 were excluded due to underlying diseases with the potential to influence clinical features: pneumoconiosis, n=2; nonspecific interstitial pneumonia, n=1; lung cancer, n=1; tracheal cancer, n=1; and tracheal stenosis, n=1. As a result, 97 patients were included. The adverse outcome group comprised 10 patients; six died within 30 days after admission and four required inotropic support or endotracheal intubation. The remaining 87 patients were allocated to the control group.
In both groups, the majority of COPD exacerbations were caused by respiratory tract infections (pneumonia or tracheobronchitis) (Figure 1). The frequency of mental change was significantly more common in the adverse outcome group, as compared with the control group (3 [30%] vs. 5 [6%], p=0.034) (Table 1). However, no significant intergroup difference was found for BAP-65 class or the frequency of a high BAP-65 score (class IV-V). In addition, no significant difference was evident in percent predicted value of post-bronchodilator forced expiratory volume in one second (FEV1) and post-bronchodilator FEV1/forced vital capacity between the two groups.
Blood test results are presented in Table 2. Median ESR level tended to be lower in the adverse outcome group (14 mm/hr [IQR, 10-26 mm/hr] vs. 25 mm/hr [15-39 mm/hr]; p=0.068), and median serum CRP was significantly lower (1.26 mg/dL [0.35-2.92 mg/dL] vs. 3.54 mg/dL [1.33-8.27 mg/dL]; p=0.041). Median serum procalcitonin levels did not differ significantly. However, median serum NT-proBNP level tended to be higher in the adverse outcome group (1,799 [123-7,118] vs. 263 [69-833]; p=0.088). No significant difference was noted in plasma troponin I between the two groups. PaCO2>37 mm Hg was significantly more frequent in the adverse outcome group (8 [80%] vs. 19 [22%]; p<0.001), and P(A-a)O2 tended be higher in the adverse outcome group (105 mm Hg [36-157 mm Hg] vs. 52 mm Hg [34-75 mm Hg]; p=0.094).
Elevated serum GDF-15 levels (GDF-15>1,600 pg/mL) was significantly more common in the adverse outcome group (8 [80%] vs. 37 [43%]; p=0.041). In contrast, median serum H-FABP and the frequency of elevated H-FABP levels (H-FABP>755 pg/mL) were not significantly different between the two groups.
Echocardiographic parameters, including RV dysfunction, RVSP, and pulmonary hypertension, did not show any differences between the two groups (Table 3). There was no difference in LVEF between both groups. Of CT findings, no differences in PA/AA diameter ratio and signs of pulmonary hypertension (PA/AA diameter ratio>1) were observed between the two groups.
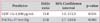
To identify predictors of adverse outcomes, we performed multiple logistic regression analysis. Of parameters with p<0.1 in the univariate analysis, serum NT-proBNP was excluded in multivariate analysis, because both NT-proBNP and GDF-15 are surrogate markers of myocardial stretch. Consequently, mental change, PaCO2>37 mm Hg, P(A-a)O2, and GDF-15 elevation (GDF-15>1,600 pg/mL) were selected for multivariate analysis to predict adverse outcomes in patients with COPD exacerbation (Table 4). The Hosmer-Lemeshow test indicated that the overall model fit was good (p=0.929). Multivariate analysis showed that PaCO2>37 mm Hg and GDF-15 elevation were significant predictors of adverse outcomes (odds ratio [OR], 25.8; 95% confidence interval [CI], 2.7-243.8; p=0.005 and OR, 11.8; 95% CI, 1.2-115.3; p=0.034, respectively).
The present study shows that an elevated serum GDF-15 level and PaCO2>37 mm Hg are predictors of an adverse outcome in patients hospitalized due to COPD exacerbation. To the best of our knowledge, this is the first report to suggest that serum GDF-15 is of prognostic value in patients presenting with COPD exacerbation. On the other hand, the present study failed to demonstrate that H-FABP predicts an adverse outcome in these patients.
GDF-15 functions as a stress-inducible cardiokine that protects against pathologic myocardial remodeling in response to a pressure or volume overload34. Blood biomarkers of cardiac dysfunction, such as NT-proBNP and troponin T, have been previously reported to indicate a poor prognosis in patients with COPD exacerbation7. Similarly, our results suggest an elevated serum GDF-15 level independently predict an adverse outcome in these patients. However, serum GDF-15 was not found to be significantly correlated with serum NT-proBNP (data not shown), which is predominantly released by cardiac stress due to myocardial stretch and pressure or volume overload. Furthermore, median values of echocardiographic LVEF were similar in the two groups, suggesting that less severe LV dysfunction occurs during COPD exacerbation than during overt left heart failure. Circulating levels of GDF-15 are known to be elevated in patients with acute pulmonary embolism15 and in those with idiopathic pulmonary arterial hypertension16, which suggests that GDF-15 may respond to RV overload. However, parameters suggestive of pulmonary hypertension, such as RVSP>40 mm Hg and PA/AA diameter ratio>1 were not different in our groups, and thus, it is not clear whether elevated GDF-15 levels resulted primarily from LV or RV dysfunction. Furthermore, serum GDF-15 levels are known to be elevated in other inflammatory conditions and cancer, which leads us to speculate GDF-15 elevation might be caused by systemic inflammation associated with COPD exacerbation. However, serum GDF-15 levels were not found to be correlated with the blood levels of inflammatory markers, such as ESR, CRP, or procalcitonin (data not shown). Consequently, we did not determine whether GDF-15 elevation was caused by RV or LV dysfunction or systemic inflammation.
H-FABP is released by irreversible damage to cardiomyocytes, a reversible disturbance of cardiomyocyte metabolism, or mechanical stretching mechanisms22. H-FABP and troponin I are both known biomarkers of myocardial injury, but were not found to be significant predictors of an adverse outcome for severe COPD exacerbation in this study. Furthermore, circulating H-FABP levels were not significantly correlated with the blood levels of troponin I or NT-proBNP (data not shown). Interestingly, PaCO2>37 mm Hg was also identified as an independent prognostic factor of an adverse outcome in patients with COPD exacerbation, which concurs with previous reports that hypercapnia can predict short-term mortality, admission to intensive care unit, and an adverse outcome in patients with COPD exacerbation6,7,35.
Several study limitations need to be mentioned. First, this study was performed at a single center and the number of patients studied was inadequate. Thus, we cannot present a definitive conclusion regarding the ability of serum GDF-15 to predict an adverse outcome in patients with COPD exacerbation. To confirm our conclusion, larger-scale study is needed. Second, although patients were prospectively enrolled into this study, not all patients underwent echocardiography, and thus, selection bias was not avoided. However, we do not believe echocardiographic findings influenced our main findings.
In conclusion, blood GDF-15 elevation and PaCO2>37 mm Hg were found to predict independently an adverse outcome in patients hospitalized for COPD exacerbation. These findings suggest that blood GDF-15 be considered to be a potential novel biomarker in patients with COPD exacerbation.
Figures and Tables
 | Figure 1Causes of chronic obstructive pulmonary disease exacerbation. The most common cause was tracheobronchitis (60% [n=6] in the adverse outcome group and 69% [n=60] in the control group, respectively), followed by pneumonia (30% [n=3] in the adverse outcome group and 22% [n=19] in the control group, respectively). |
References
1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997; 349:1498–1504.
2. Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev. 2010; 19:113–118.
3. Connors AF Jr, Dawson NV, Thomas C, Harrell FE Jr, Desbiens N, Fulkerson WJ, et al. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments). Outcomes following acute exacerbation of severe chronic obstructive lung disease. Am J Respir Crit Care Med. 1996; 154(4 Pt 1):959–967.
4. Groenewegen KH, Schols AM, Wouters EF. Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest. 2003; 124:459–467.
5. Singanayagam A, Schembri S, Chalmers JD. Predictors of mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013; 10:81–89.
6. Stolz D, Breidthardt T, Christ-Crain M, Bingisser R, Miedinger D, Leuppi J, et al. Use of B-type natriuretic peptide in the risk stratification of acute exacerbations of COPD. Chest. 2008; 133:1088–1094.
7. Chang CL, Robinson SC, Mills GD, Sullivan GD, Karalus NC, McLachlan JD, et al. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011; 66:764–768.
8. Baillard C, Boussarsar M, Fosse JP, Girou E, Le Toumelin P, Cracco C, et al. Cardiac troponin I in patients with severe exacerbation of chronic obstructive pulmonary disease. Intensive Care Med. 2003; 29:584–589.
9. Rammaert B, Verdier N, Cavestri B, Nseir S. Procalcitonin as a prognostic factor in severe acute exacerbation of chronic obstructive pulmonary disease. Respirology. 2009; 14:969–974.
10. Meadows CA, Risbano MG, Zhang L, Geraci MW, Tuder RM, Collier DH, et al. Increased expression of growth differentiation factor-15 in systemic sclerosis-associated pulmonary arterial hypertension. Chest. 2011; 139:994–1002.
11. Su AI, Wiltshire T, Batalov S, Lapp H, Ching KA, Block D, et al. A gene atlas of the mouse and human protein-encoding transcriptomes. Proc Natl Acad Sci U S A. 2004; 101:6062–6067.
12. Wollert KC, Kempf T, Peter T, Olofsson S, James S, Johnston N, et al. Prognostic value of growth-differentiation factor-15 in patients with non-ST-elevation acute coronary syndrome. Circulation. 2007; 115:962–971.
13. Kempf T, Bjorklund E, Olofsson S, Lindahl B, Allhoff T, Peter T, et al. Growth-differentiation factor-15 improves risk stratification in ST-segment elevation myocardial infarction. Eur Heart J. 2007; 28:2858–2865.
14. Kempf T, von Haehling S, Peter T, Allhoff T, Cicoira M, Doehner W, et al. Prognostic utility of growth differentiation factor-15 in patients with chronic heart failure. J Am Coll Cardiol. 2007; 50:1054–1060.
15. Lankeit M, Kempf T, Dellas C, Cuny M, Tapken H, Peter T, et al. Growth differentiation factor-15 for prognostic assessment of patients with acute pulmonary embolism. Am J Respir Crit Care Med. 2008; 177:1018–1025.
16. Nickel N, Kempf T, Tapken H, Tongers J, Laenger F, Lehmann U, et al. Growth differentiation factor-15 in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med. 2008; 178:534–541.
17. Alhadi HA, Fox KA. Do we need additional markers of myocyte necrosis: the potential value of heart fatty-acid-binding protein. QJM. 2004; 97:187–198.
18. Storch J, Thumser AE. The fatty acid transport function of fatty acid-binding proteins. Biochim Biophys Acta. 2000; 1486:28–44.
19. O'Donoghue M, de Lemos JA, Morrow DA, Murphy SA, Buros JL, Cannon CP, et al. Prognostic utility of heart-type fatty acid binding protein in patients with acute coronary syndromes. Circulation. 2006; 114:550–557.
20. Dellas C, Puls M, Lankeit M, Schafer K, Cuny M, Berner M, et al. Elevated heart-type fatty acid-binding protein levels on admission predict an adverse outcome in normotensive patients with acute pulmonary embolism. J Am Coll Cardiol. 2010; 55:2150–2157.
21. Puls M, Dellas C, Lankeit M, Olschewski M, Binder L, Geibel A, et al. Heart-type fatty acid-binding protein permits early risk stratification of pulmonary embolism. Eur Heart J. 2007; 28:224–229.
22. Boscheri A, Wunderlich C, Langer M, Schoen S, Wiedemann B, Stolte D, et al. Correlation of heart-type fatty acid-binding protein with mortality and echocardiographic data in patients with pulmonary embolism at intermediate risk. Am Heart J. 2010; 160:294–300.
23. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007; 176:532–555.
24. Tillie-Leblond I, Marquette CH, Perez T, Scherpereel A, Zanetti C, Tonnel AB, et al. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med. 2006; 144:390–396.
25. Choi KJ, Cha SI, Shin KM, Lee J, Hwangbo Y, Yoo SS, et al. Prevalence and predictors of pulmonary embolism in Korean patients with exacerbation of chronic obstructive pulmonary disease. Respiration. 2013; 85:203–209.
26. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988; 93:580–586.
27. Shorr AF, Sun X, Johannes RS, Yaitanes A, Tabak YP. Validation of a novel risk score for severity of illness in acute exacerbations of COPD. Chest. 2011; 140:1177–1183.
28. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.
29. McQuillan BM, Picard MH, Leavitt M, Weyman AE. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation. 2001; 104:2797–2802.
30. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989; 2:358–367.
31. Wells JM, Washko GR, Han MK, Abbas N, Nath H, Mamary AJ, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012; 367:913–921.
32. Devaraj A, Wells AU, Meister MG, Corte TJ, Wort SJ, Hansell DM. Detection of pulmonary hypertension with multidetector CT and echocardiography alone and in combination. Radiology. 2010; 254:609–616.
33. Edwards PD, Bull RK, Coulden R. CT measurement of main pulmonary artery diameter. Br J Radiol. 1998; 71:1018–1020.
34. Shimano M, Ouchi N, Walsh K. Cardiokines: recent progress in elucidating the cardiac secretome. Circulation. 2012; 126:e327–e332.
35. Matkovic Z, Huerta A, Soler N, Domingo R, Gabarrus A, Torres A, et al. Predictors of adverse outcome in patients hospitalised for exacerbation of chronic obstructive pulmonary disease. Respiration. 2012; 84:17–26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download