Abstract
Although endobronchial hamartoma is a rare benign tumor, most patients with endobronchial hamartoma have respiratory symptoms such as obstructive pneumonia, hemoptysis, cough, or dyspnea due to bronchial obstruction. It can cause irreversible post-obstructive pulmonary destruction, thus early diagnosis and treatment is very important. Recently, there have been cases of neodymium-doped yttrium aluminum garnet (Nd:YAG) laser and electrocautery procedures for bronchoscopic treatment of malignant or benign central airway obstruction with comparable therapeutic efficacy and few complications. Bronchoscopic cryotherapy is a newly developed technique for management of central airway obstruction. Moreover, it provides diagnostic methods with improving diagnostic yield and safety. We report two cases of endobronchial hamartoma, each diagnosed and definitively treated with bronchoscopic techniques. Endobronchial biopsy and removal was successfully performed by cryotherapy via flexible bronchoscopy without notable complications. Follow-up bronchoscopic examinations excluded residual or recurrent disease.
Endobronchial hamartoma is a rare benign tumor derived from peribronchial mesenchymal tissue. It can cause irreversible postobstructive pulmonary destruction with respiratory symptoms. Early diagnosis and treatment is very important. Traditionally, surgical resection has been considered the standard of treatment for endobronchial hamartoma. However, there is increasing experience using endoscopic treatment such as neodymium-doped yttrium aluminum garnet (Nd:YAG) laser and electrocautery for benign endobronchial tumor with a paucity of reported complications1.
Bronchoscopic cryotherapy is a technique in which endobronchial tissue is destroyed by repeated freezing and thawing. This bronchoscopic technique is most often employed as a palliative therapy for malignant central airway obstruction with or without other modalities of endobronchial treatment2,3.
We report two cases of endobronchial hamartoma, each diagnosed and definitively treated by cryotherapy via flexible bronchoscopy.
A 49-year-old man was referred to our hospital for bronchoscopic evaluation for obstructive pneumonia on superior segment of right lower lung (RS6) on chest X-ray and chest computed tomography (CT) (Figure 1A-D). The bronchoscopic examination with autofluorescence bronchoscopy (system: Onco-Life for Improved Cancer Detector; Xillix, Richmond, Canada and bronchoscope: BF-1T40; Olympus, Tokyo, Japan) showed the superior segmental bronchus of right lower lung (RB6) was obstructed by pedunculated mass. The cryotherapy was performed for endobronchial biopsy and tumor cryodebridement. Flexible cryoprobe (length 80 cm, length of probe tip 7 mm, diameter 2.2 mm) with cryomachine (ERBE, Tubingen, Germany) was passed through the working channel of the flexible bronchoscopy (system: ELVIS LUCERA CV-260 and CLV-260; Olympus and bronchoscope: BF-1T260; Olympus) into the tumor. The tip of flexible bronchoscope was positioned 1.0 cm from the tumor. The cryoprobe was kept about 4 mm away from the tip of the bronchoscope. Then, the tip of the cryoprobe that was placed in direct contact with the tumor was cooled to approximately -89℃ with cryogen (nitrous oxide; N2O) for 10 seconds using the foot pedal. After that time, the probe was pulled, the probe with frozen tissue was withdrawn with bronchoscope (pull-out method). The mass was successfully removed with several repeated procedures with small amount of bleeding (Figure 2A-G). The bleeding was controlled by iced saline. The biopsy result of removed mass was chondroid hamartoma (Figure 2H). Imaging study at 3 months after removal of endobronchial hamartoma showed completely resolution of previous obstructive pneumonia on RS6 (Figure 1E-H). And bronchoscopic examination after 3 months after removal showed good patency without any obstruction of RB6 (Figure 2I, J).
A 53-year-old man was referred to our hospital for bronchoscopic evaluation for abnormal density in front of superior segmental bronchus of left lower lung (LB6) on chest CT on personal health examination (Figure 3A-C). The bronchoscopic examination with autofluorescence bronchoscopy showed LB6 was obstructed by pedunculated mass. The cryotherapy was performed for endobronchial biopsy and tumor cryodebridement with same above described procedures. The mass was successfully removed with small amount of bleeding (Figure 4A-G). The bleeding was controlled by iced saline. The biopsy result of removed mass was hamartoma (Figure 4H). Chest X-ray at 1 month after resection of endobronchial hamartoma showed normal chest X-ray finding (Figure 3D, E). And bronchoscopic examination after 1 month after removal showed good patency without any obstruction of LB6 (Figure 4I, J).
Pulmonary hamartomas are the most common benign tumors of lung, with incidence 0.32% according to autopsy study4. Pulmonary hamartomas divided into two groups according to their location: parenchymal hamartomas or endobronchial hamartomas. Endobronchial hamartomas have low frequency between 1.4% and 13.8% of all pulmonary hamartomas5,6,7,8. Unlike the patients with parenchymal hamartomas, most patients with endobronchial hamartomas had at least one of respiratory complaints due to bronchial obstruction such as obstructive pneumonia, hemoptysis, cough, or dyspnea. Although endobronchial hamartomas are benign tumor with very low risk of malignancy and low rate of recurrence, early diagnosis and treatment is very important due to potential risk of bronchial obstruction, bleeding, and subsequent respiratory symptoms.
Although surgical resection has been considered the standard of treatment for endobronchial hamartomas, there is increasing case reports and case series using bronchoscopic treatment such as Nd:YAG laser and electrocautery with comparable therapeutic efficacy with surgical resection and few reported complications1.
Cryotherapy is the application of extreme cold energy to diseased tissue, in which cells are destroyed by the formation of intracellular ice crystals. In 1968, the first case of the use of rigid cryoprobe through a rigid bronchoscope to relieve endobronchial obstruction by a tumor causing a postobstructive pneumonia was reported9,10. Because of the need of general anesthesia and rigid bronchoscopy as well as development of other bronchoscopic treatment modalities such as laser resection, electrocautery, argon plasma coagulation, and photodynamic therapy, there was a relatively little interest in bronchoscopic cryotherapy until introduction of a flexible cryoprobe that allowed delivery through the flexible bronchoscope in 1994. Now, bronchoscopic cryotherapy is recognized as a useful endobronchial treatment modality in the palliative management for airway obstruction due to a malignancy11,12. Bronchoscopic cryotherapy is also useful in management for airway obstruction due to a benign endobronchial lesion, inoperable microinvasive carcinoma, hemoptysis due to a visible lesion, and the extraction of foreign bodies.
For tumor cryodebridement, cryotherapy can be delivered through rigid or flexible bronchoscopy. After a full examination of bronchial segments, the tip of the bronchoscope is positioned 0.5-1.0 cm from the identified endobronchial lesion. Then, the cryoprobe inserted via the working channel of the bronchoscope. The cryoprobe is placed in direct contact with the tumor. Using the foot pedal, the bronchoscopist activates the cryoprobe. Cryogen will cool the probe tip to about -89℃. At this time, there are two techniques of cryodebridements: repeated thawing-freezing technique and pull-out technique9,10. In a repeated thawing-freezing technique, freezing is continued for 30 seconds, after which the foot pedal is released, and passive thawing is allowed. This cycle is repeated an average of three cycles at each site of the tumor. Resultant necrotic tissue can be removed by suctioning, by biopsy forceps, or freezing the tissue to the cryoprobe. Repeated bronchoscopic examination is necessary for removal of necrotic tissue and clearing of secretion due to delayed sloughing of treated tissue. In a pull-out technique, the tip of the cryoprobe is cooled for 5-20 seconds. Then, the probe is pulled strongly, and the cryoprobe with frozen tissue attached to its tip is withdrawn along with the bronchoscope. The Pull-out technique, a newer method, has the potential advantage to decrease procedural time and achieve faster results with less need of repeated procedures9. In our two cases, we selected a pull-out technique as a technique of cryotherapy for this reasons.
Recently, two diagnostic methods with cryotherapy were developed with improving diagnostic yield and safety: endobronchial biopsy with cryotherapy and fluoroscopy-guided transbronchial cryoprobe lung biopsy13,14. During performing an endobronchial biopsy with cryoprobe, the cryoprobe is passed through the working channel of the bronchoscope and advanced 4 mm beyond the tip of the bronchoscope. Direct contact between the probe and the lesion is achieved. Tissue is frozen to the cryoprobe tip by activating the probe for approximately 5 seconds. While maintaining probe activation, the cryoprobe, with the frozen sample attached to it, is retracted back through the working channel of the bronchoscope. Alternatively, the cryoprobe with the frozen tissue attached to it can also be removed along with the flexible bronchoscope9.
The effectiveness of cryotherapy is limited in long-segment, submucosal, and extrinsic tumors9. Our cases were suitable for cryotherapy because endobronchial tumors narrowly attached the bronchus with stalk. We could relatively easily perform the endobronchial biopsy and removal of endobronchial hamartoma using cryotherapy via flexible bronchoscopy without complications. In case series of 521 patients, in-hospital mortality rate was 1%, all of which was due to respiratory failure3. Three percent of patients developed respiratory distress after procedure which eventually resolved. Bleeding is usually mild and can generally be controlled by suction. During our procedures and postprocedural period, there was no notable complication except small amount of bleeding that was easily controlled by iced saline. Follow-up bronchoscopic examinations excluded residual or recurrent disease in our cases.
Although endobronchial cryotherapy has the disadvantages of potential need for repeated procedure, some delayed effects of treatment, and the relative resistance of certain benign tumors than other thermal techniques, this procedure has the advantage of a more favorable safety profiles and easier setup and procedural technique9,10. We suggested cryotherapy with flexible bronchoscopy may be useful diagnostic and therapeutic modality in management of endobronchial tumor with few complications with or without other thermal modalities of endobronchial treatment.
Figures and Tables
Figure 1
(A-D) Imaging study on admission day suggested obstructive pneumonia on superior segment of right lower lung (RS6). (A, B) Posterior-anterior (PA) view and lateral view of chest X-ray. (C) Transverse section of chest computed tomography (CT). (D) Coronal section of chest CT. (E-H) Imaging study at 3 months after removal of endobronchial hamartoma on superior segmental bronchus of right lower lung (RB6) showed completely resolution of previous obstructive pneumonia on RS6. (E, F) PA view and lateral view of chest X-ray. (G) Transverse section of chest CT. (H) Coronal section of chest CT.
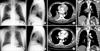
Figure 2
(A, B) The bronchoscopic examination showed the superior segmental bronchus of right lower lung (RB6) was obstructed by pedunculated mass. (A) White light image. (B) Autofluorescence image. (C-G) Procedure image of resection of the mass on RB6 with cryotherapy. Biopsy showed chondroid hamartoma (H&E stain, ×100) (H) and bronchoscopic examination after 3 months after resection of endobronchial hamartoma showed good patency without any obstruction of RB6 (I, J).

Figure 3
(A-C) Imaging study of personal health examination showed a 1.1 cm-sized fat density lesion on superior segmental bronchus of left lower lung (LB6). (A) Posterior-anterior (PA) view of chest X-ray. (B) Transverse section of chest computed tomography (CT). (C) Coronal section of chest CT. (D, E) Imaging study at 1 month after resection of endobronchial hamartoma on LB6. (D) PA view of chest X-ray. (E) Lateral view of chest X-ray.
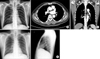
Figure 4
(A, B) The bronchoscopic examination showed the superior segmental bronchus of left lower lung (LB6) was obstructed by pedunculated mass. (A) White light image. (B) Autofluorescence image. (C-G) Procedure image of resection of the mass on LB6 with cryotherapy. Biopsy showed hamartoma (H&E stain, ×100) (H) and bronchoscopic examination after 1 month after resection of endobronchial hamartoma showed good patency without any obstruction of LB6 (I, J).

References
1. Miller SM, Bellinger CR, Chatterjee A. Argon plasma coagulation and electrosurgery for benign endobronchial tumors. J Bronchology Interv Pulmonol. 2013; 20:38–40.
2. Mathur PN, Wolf KM, Busk MF, Briete WM, Datzman M. Fiberoptic bronchoscopic cryotherapy in the management of tracheobronchial obstruction. Chest. 1996; 110:718–723.
3. Maiwand MO, Asimakopoulos G. Cryosurgery for lung cancer: clinical results and technical aspects. Technol Cancer Res Treat. 2004; 3:143–150.
4. Murray J, Kielkowski D, Leiman G. The prevalence and age distribution of peripheral pulmonary hamartomas in adult males: an autopsy-based study. S Afr Med J. 1991; 79:247–249.
5. Gjevre JA, Myers JL, Prakash UB. Pulmonary hamartomas. Mayo Clin Proc. 1996; 71:14–20.
6. Lee SH, Yoon HK, Song SH, Lee SY, Kim SC, Ahn JH, et al. Clinical analysis of pulmonary hamartoma: 29 cases. Tuberc Respir Dis. 2002; 53:644–649.
7. Kim SA, Um SW, Song JU, Jeon K, Koh WJ, Suh GY, et al. Bronchoscopic features and bronchoscopic intervention for endobronchial hamartoma. Respirology. 2010; 15:150–154.
8. Cosio BG, Villena V, Echave-Sustaeta J, de Miguel E, Alfaro J, Hernandez L, et al. Endobronchial hamartoma. Chest. 2002; 122:202–205.
9. Sunna R. Chapter 33. Cryotherapy and cryodebridement. In : Ernst A, Herth FJ, editors. Principles and practice of interventional pulmonology. New York: Springer Science;2013. p. 343–350.
10. Morgan RK, Ernst A. Chapter 12. Cryotherapy. In : Strausz J, Bolliger CT, editors. Interventional pulmonology: European respiratory monograph. Sheffield: European Respiratory Society;2010. p. 161–172.
11. Ernst A, Feller-Kopman D, Becker HD, Mehta AC. Central airway obstruction. Am J Respir Crit Care Med. 2004; 169:1278–1297.
12. Vergnon JM, Huber RM, Moghissi K. Place of cryotherapy, brachytherapy and photodynamic therapy in therapeutic bronchoscopy of lung cancers. Eur Respir J. 2006; 28:200–218.
13. Schumann C, Hetzel J, Babiak AJ, Merk T, Wibmer T, Moller P, et al. Cryoprobe biopsy increases the diagnostic yield in endobronchial tumor lesions. J Thorac Cardiovasc Surg. 2010; 140:417–421.
14. Babiak A, Hetzel J, Krishna G, Fritz P, Moeller P, Balli T, et al. Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration. 2009; 78:203–208.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download