Abstract
Methcillin-resistant Staphylococcus aureus (MRSA) has emerged as an important cause of community-acquired infections, which has been recently designated as community-associated (CA) MRSA. Panton-Valentine leukocidin (PVL)-negative multilocus sequence type 72 (ST72)-staphylococcal cassette chromosome mec (SCCmec) type IV has been reported as the predominat CA-MRSA strain in Korea and is commonly associated with skin and soft tissue infections in addition to healthcare-associated pneumonia. However, community-acquired pneumonia (CAP) for this strain has not yet been reported. We hereby report two cases of CAP caused by PVL-negative ST72-SCCmec type IV strain in patients who had no risk factors for MRSA acquisition. While CA-MRSA infections are not yet prevalent in Korea, our cases suggest that CA-MRSA should be considered in cases of severe CAP, especially for cases associated with necrotizing pneumonia.
Methicillin-resistant Staphylococcus aureus (MRSA) is a well-known cause of healthcare-associated infection1. However, MRSA infections have been reported in previously healthy individuals with no recent history of healthcare contact1,2. While community-associated MRSA (CA-MRSA) has primarily been described as a cause of skin and soft-tissue infections2, it has also been associated with sepsis and necrotizing pneumonia3-5. Many of these MRSA strains carry the type IV and type V staphylococcal cassette chromosome mec (SCCmec) which produce certain toxins (Panton-Valentine leukocidin [PVL]). These strains are generally only resistant to the β-lactams and macrolides and have specific molecular typing patterns6.
S. aureus is an important cause of nosocomial pneumonia and less commonly a cause of community-acquired pneumonia (CAP). In recent years, CA-MRSA strains, particularly PVL-positive strains, have been increasingly reported as causative agents of CAP in the United States and Europe3-5. In Korea, PVL-negative multilocus sequence type 72 (ST72)-SCCmec type IV has been reported as the predominant CA-MRSA stain7. Although healthcare-associated pneumonia is one of the most frequent types of community-onset healthcare-associated infections caused by ST72-SCCmec type IV strain in Korea, CAP due to the strain has not been reported8. We report two extraordinary cases of CAP caused by the ST72-SCCmec type IV strain in patients who had no prior risk factors for MRSA acquisition.
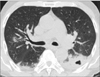
A 66-year-old man was referred to the Samsung Medical Center, Seoul, Korea, following a diagnosis of CAP with cytopenia which was made at another hospital. Three weeks prior to admission, he had ingested water of boiled wild mushroom. While he developed nausea and headache, which spontaneously resolved without medication, he did not experience any respiratory symptoms. Two week later, he developed dyspnea on exertion. He visited his regional hospital presenting with fever and dyspnea and was diagnosed with CAP. However, he was referred to our hospital for leukopenia (leukocyte count, 300/µL; absolute neutrophil count, 0/µL) and thrombocytopenia (platelet count, 3,000/µL) found on initial laboratory tests at the regional hospital. On admission to our hospital, his condition deteriorated rapidly and he was placed on mechanical ventilation for severe hypoxemia. Chest computed tomography (CT) showed consolidation and ground-glass opacity with cavitation in the left lower lobe which was compatible with necrotizing pneumonia (Figure 1). The patient was diagnosed with severe necrotizing pneumonia in a neutropenic patient and was administered vancomycin, piperacillin-tazobactam and levofloxacin. Aplastic anemia associated with wild mushroom toxin was diagnosed with bone marrow biopsy which showed hypocellular marrow with suppressed trilineage hematopoiesis. While the Gram stain of respiratory specimens showed gram-positive cocci in pairs, chains and clusters, the urinary antigen test for Streptococcus pneumoniae was negative. The culture from sputum grew MRSA and while the strain was susceptible to gentamicin, rifampicin, ciprofloxacin and trimethoprim/sulfamethoxazole, it was resistant to erythromycin and clindamycin. The patient recovered completely following a 2 week treatment course with vancomycin. In order to genotype the bacterial isolate, multilocus sequence typing (MLST) was performed using polymerase chain reaction (PCR) amplification and sequencing of seven housekeeping genes (arcC, aroE, glpF, gmk, pta, tpi, and yqiL) as previously described9. SCCmec type was determined by the multiplex PCR method. The isolate was screened for the genes (lukF-PV and lukS-PV) encoding the components of the PVL toxin by PCR amplification10. Typing of the MRSA isolate from the patient revealed that the isolate belonged to MLST ST72, carried SCCmec type IV and was negative for PVL.
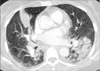
A 57-year-old woman who had previously been healthy except for a history of pulmonary tuberculosis thirty years ago and who was on current medication for hypertension and depressive episodes, was admitted to our hospital with high fever, cough and sputum for 3 days. On admission, dyspnea and chest pain developed. Chest CT showed multiple patchy consolidations in both lower lobes and the right middle lobe of the lung (Figure 2). Laboratory tests revealed a leukocyte count of 1,820/µL, hemoglobin at 9.9 g/dL, and a platelet count of 192,000/µL. After 2 days, she rapidly deteriorated and was admitted to the intensive care unit (ICU) following intubation for severe hypoxemia. She was diagnosed with severe CAP and ceftriaxone and azithromycin were administrated empirically. While Gram stain of respiratory specimens revealed gram-positive cocci, the urinary antigen test for S. pneumoniae was negative. MRSA grew from sputum culture and the strain was susceptible to gentamicin, rifampicin, ciprofloxacin, trimethoprim/sulfamethoxazole, erythromycin and clindamycin. Vancomycin was added to the empiric treatment on hospital day 5. Due to the persistent fever following administration of vancomycin for 7 days, vancomycin was replaced with linezolid. Bilateral infiltration in the lungs with respiratory failure resulted in acute respiratory distress syndrome which was treated with adjunctive corticosteroid treatment. Ultimately, the patient recovered following linezolid treatment for 7 days in addition to vancomycin treatment for 7 days and corticosteroid treatment for 4 weeks. Typing of the MRSA isolate from the patient revealed that the isolate belonged to MLST ST72, carried SCCmec type IV and was negative for PVL.
To our knowledge, this is the first report of CAPs caused by ST72-SCCmec, type IV strain which is the predominant CA-MRSA strain in Korea. Although the first case developed in an immunocompromised individual with aplastic anemia associated with wild mushroom toxin, the patient had severe pneumonia requiring admission to the ICU and mechanical ventilation support, which are consistent with previously reported cases of CA-MRSA pneumonia3,5. Nonetheless, each isolate was negative for PVL which is a cytotoxin produced by approximately 5% of S. aureus strains and is associated with up to 85% of severe necrotizing pneumonia5,10,11. Some of these respiratory infections have been associated with septic shock, hemoptysis, respiratory failure and intensive care admission for ventilatory or circulatory support12,13. However, recently reported case series have revealed that PVL-negative CA-MRSA may also cause severe necrotizing pneumonia suggesting the presence of other virulence factors responsible for necrotizing pneumonia caused by CA-MRSA14. While some data suggest an important pathogenic role of PVL in MRSA pneumonia, debate remains about the importance of this toxin in the pathogenesis of CA-MRSA pneumonia or whether PVL is merely a marker of CA-MRSA infections13.
CA-MRSA infections previously tended to arise largely from specific patient groups especially in high-risk settings such as military recruits, sports teams and individuals living in close communities or involved in activities resulting in skin abrasions13. However, recent CA-MRSA infections have arisen in otherwise healthy individuals who did not have such risk factors. Young age of patients has been a remarkable feature of CA-MRSA pneumonia in both European and US cases4,5,12,13. Severe cases of CA-MRSA pneumonia have been reported during influenza season or have been associated with a preceding influenza or influenza-like illness in the majority of cases4,5,12,13. In our cases, a preceding influenza-like illness was mentioned in the first case but not in the second case. In contrast to other bacterial pneumonia in which leukocytosis is a prominent feature, leukopenia may be observed in a substantial proportion of cases and is predictive of poor outcome3,15. Although the patient in the first case developed cytopenia associated with aplastic anemia, both of them had leukopenia.
In conclusion, we report the emergence of CA-MRSA in Korea as a cause of CAP in otherwise healthy individuals. While CA-MRSA infections are not yet prevalent in Korea7,8, our cases suggest that CA-MRSA should be considered in cases of severe CAP, especially in those cases associated with necrotizing pneumonia.
Figures and Tables
Acknowledgements
The authors would like to thank J.Y. Baek, Asia Pacific Foundation for Infectious Diseases, Seoul, Korea, for her technical assistance.
References
1. Fridkin SK, Hageman JC, Morrison M, Sanza LT, Como-Sabetti K, Jernigan JA, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005; 352:1436–1444.
2. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006; 355:666–674.
3. Francis JS, Doherty MC, Lopatin U, Johnston CP, Sinha G, Ross T, et al. Severe community-onset pneumonia in healthy adults caused by methicillin-resistant Staphylococcus aureus carrying the Panton-Valentine leukocidin genes. Clin Infect Dis. 2005; 40:100–107.
4. Hageman JC, Uyeki TM, Francis JS, Jernigan DB, Wheeler JG, Bridges CB, et al. Severe community-acquired pneumonia due to Staphylococcus aureus, 2003-04 influenza season. Emerg Infect Dis. 2006; 12:894–899.
5. Gillet Y, Issartel B, Vanhems P, Fournet JC, Lina G, Bes M, et al. Association between Staphylococcus aureus strains carrying gene for Panton-Valentine leukocidin and highly lethal necrotising pneumonia in young immunocompetent patients. Lancet. 2002; 359:753–759.
6. Patel M. Community-associated meticillin-resistant Staphylococcus aureus infections: epidemiology, recognition and management. Drugs. 2009; 69:693–716.
7. Kim ES, Song JS, Lee HJ, Choe PG, Park KH, Cho JH, et al. A survey of community-associated methicillin-resistant Staphylococcus aureus in Korea. J Antimicrob Chemother. 2007; 60:1108–1114.
8. Joo EJ, Chung DR, Ha YE, Park SY, Kang SJ, Kim SH, et al. Community-associated Panton-Valentine leukocidin-negative meticillin-resistant Staphylococcus aureus clone (ST72-MRSA-IV) causing healthcare-associated pneumonia and surgical site infection in Korea. J Hosp Infect. 2012; 81:149–155.
9. Enright MC, Day NP, Davies CE, Peacock SJ, Spratt BG. Multilocus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000; 38:1008–1015.
10. Lina G, Piemont Y, Godail-Gamot F, Bes M, Peter MO, Gauduchon V, et al. Involvement of Panton-Valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. Clin Infect Dis. 1999; 29:1128–1132.
11. Micek ST, Dunne M, Kollef MH. Pleuropulmonary complications of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus: importance of treatment with antimicrobials inhibiting exotoxin production. Chest. 2005; 128:2732–2738.
12. Rubinstein E, Kollef MH, Nathwani D. Pneumonia caused by methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008; 46:Suppl 5. S378–S385.
13. Hidron AI, Low CE, Honig EG, Blumberg HM. Emergence of community-acquired meticillin-resistant Staphylococcus aureus strain USA300 as a cause of necrotising community-onset pneumonia. Lancet Infect Dis. 2009; 9:384–392.
14. Thomas R, Ferguson J, Coombs G, Gibson PG. Community-acquired methicillin-resistant Staphylococcus aureus pneumonia: a clinical audit. Respirology. 2011; 16:926–931.
15. Gillet Y, Vanhems P, Lina G, Bes M, Vandenesch F, Floret D, et al. Factors predicting mortality in necrotizing community-acquired pneumonia caused by Staphylococcus aureus containing Panton-Valentine leukocidin. Clin Infect Dis. 2007; 45:315–321.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download