Abstract
Capillary hemangioma of the tracheobronchial tree is an extremely rare benign tumor in adults, especially those located in the bronchus. Characteristics and treatment of capillary hemangiomas of adult tracheobronchial trees have not been well known. We present a 61-year-old man with hemoptysis, which was caused by a small tiny nodule in the left lingular segmental bronchus. The nodule was removed by a forcep biopsy, via flexible bronchoscopy, and it was revealed to be capillary hemangioma. A small isolated endobronchial capillary hemangioma can be treated with excisional forcep biopsy, but a risk of massive bleeding should not be overlooked.
Capillary hemangiomas are benign lesions which usually occur in the skin, mucous membranes of the oral cavity and lips, and internal viscera1. Capillary hemangiomas of tracheobronchial trees are very rare in both adults and infants2. In Korean literature, there have been several reports of capillary hemangioma of adult trachea3,4 and lung parenchyma5, but none has been reported to date in the lobar bronchus of adults. We report a case of isolated endobronchial capillary hemangioma in adult, which was diagnosed with pathologic examination of the forcep biopsied specimen.
A 61-year-old man visited to outpatient clinic due to small amount of fresh blood in sputum lasting for a week. He had been treated with asthma and emphysema with inhaled long-acting anticholinergics (Spiriva; Boehringer Ingelheim Pharmaceuticals, Inc., Ridgefield, CT, USA), inhaled corticosteroids (Alvesco; Nycomed GmbH, Milford, MA, USA) and oral theophylline from a year ago in our clinic. He was treated with pulmonary tuberculosis about 30 years ago and had tuberculosis sequelae in right upper lobe. He had smoked 30 pack-year of cigarettes and quit smoking 10 years ago. He had history of hypertension and diabetes mellitus, but has taken neither anti-platelet agent nor anticoagulant.
On physical examination, blood pressure was 140/80 mm Hg, heart rate was 88 beats/min, respiratory rate was 20 breaths/min, and body temperature was 36.1℃. The findings of auscultation were not significant. Laboratory tests revealed normal values of complete blood cell count, electrolytes, chemistry profile, arterial blood gas analysis, erythrocyte sedimentation rate, and C-reactive protein concentration.
Simple chest radiograph showed irregular nodular and linear opacities with volume loss in right upper lobe, which was compatible with inactive pulmonary tuberculosis. The opacities have not been changed in comparison with chest radiograph examined two-months ago. Chest computed tomography showed centrilobular and paraseptal airspace enlargement in both lungs and irregular linear and nodular opacities with distortion of surrounding architecture in right upper lobe. A tiny enhancing nodule was seen at bronchial wall of lingular segment of left upper lobe (Figure 1).
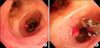
Flexible bronchoscopy was performed under local anesthesia and a 3 mm sized polypoid lesion with pinkish color was found on the medial side of left lingular segmental bronchus (Figure 2). Forcep biopsy was performed to examine and remove the lesion and small amount of bleeding was followed. The amount of bleeding was minimal and the bleeding stopped after endobronchial instillation of 1:10,000 diluted epinephrine. Small amounts of hemoptysis appeared one time after bronchoscopy, then no more hemoptysis was found till 4 weeks after bronchoscopy.
Light microscopic findings revealed small polypoid nodule which showed proliferation of blood vessels of capillary caliber and surface bronchial epithelium. The bronchial epithelium was partly eroded. Immunohistochemical stain for CD31 demonstrated vascular endothelial cells (Figure 3).
Hemangioma is a common benign tumor of the head and neck in children which usually appears a few weeks after birth, grows more rapidly during infancy, and undergoes spontaneous slow involution later in childhood6. There are several histologic and clinical variants: capillary hemangioma, carvenous hemangioma, and pyogenic granuloma. Capillary hemangioma is the most common variant of hemangiomas which occurs in the skin, subcutaneous tissues, and mucous membranes of the oral cavities and lips, as well as in internal viscera1.
Sweetser7 classified hemangiomas of the airways into an infantile and an adult variety. The infantile type is usually in the subglottic airways, rarely involving subcricoid area and usually developed dyspnea and stridor by three months. The adult types of hemangiomas are usually supraglottic, commonly involving the vocal cords. Hoarseness with little or no dyspnea is the most common manifestation, and hemoptysis occurs frequently. In both adults and infants hemangiomas involving the proximal bronchi are extremely rare2.
Characteristics and treatment of capillary hemangiomas of adult tracheobronchial trees has not been established yet because of the limited number of cases. Most frequent symptom is hemoptysis which ranges from minor to massive. In aspect of anatomic location, it can be found from trachea to lung parenchyma. The majority was found in trachea4 but isolated endobronchial lesion2,8 has been relatively infrequent. In Korean literature, several cases of tracheal capillary hemangioma3,4 and pulmonary capillary hemangioma5 were reported, and a case of capillary hemangioma of left main bronchus in an infant was reported9.
Treatment includes excisional forceps biopsy with adequate hemostasis, Nd-YAG laser, argon plasma coagulation, arteriographic embolization and endotracheal brachytherapy8,10. Most patients responded to such modalities well and showed favorable outcome. In our case, we used excisional forcep and safely removed the polypoid lesion without significant bleeding. The literature to date suggests that most cases have responded favorably to simple forceps excision via flexible fiberoptic bronchoscopy8.
Some endobronchial vascular lesions can appear to be mass-like lesions so that massive bleeding can be induced if endobronchial vascular lesions are injured during bronchoscopic biopsy. Especially, chronic destructive parenchymal diseases such as bronchiectasis and tuberculosis can lead to compensatory dilatation and proliferation of the bronchial arteries11. There are reports of massive and fatal haemorrhage from an endobronchial vascular lesion injured during bronchoscopic biopsy11,12. Because submucosal longitudinal tubular structures or pulsatile lesions could be vascular structure, bronchial arteriography should be performed before bronchoscopic biopsy in these patients11. When brochoschopic biopsy for hypervascular lesion is tried, it should be done with caution in a facility enable to do emergent intubation and well-equipped with laser coagulation or well-supported by interventional radiology to control unwanted massive bleeding. In our case, because the bronchoscopic finding was very characteristic for endobronchial haemangioma, showing a well-circumscribed reddish hypervascular lesion similar to cutaneous haemangioma, we decided to proceed bronchoscopic biopsy and tried carefully.
Capillary hemangiomas of tracheobronchial tree are a rare benign lesion, especially those located in lobar bronchus. It can be treated with several methods according to size of the lesion and amount of hemoptysis, but definite treatment has not been established. In case of a small lesion without significant amount of bleeding, excisional forcep biopsy can be safely tried like our case.
Figures and Tables
Figure 1
Axial (A) and sagittal (B) chest computed tomography scan shows a tiny protruding nodule with enhancement (arrowhead) at bronchial wall of lingular segment of left upper lobe.

References
1. Kumar V, Abbas AK, Fausto N, Aster J. Robbins and Cotran pathologic basis of disease. 8th ed. Philadelphia: Saunders Elsevier;2009.
2. Wigton RB, Rohatgi PK. Isolated bronchial capillary hemangioma: a rare benign cause of hemoptysis. South Med J. 1979; 72:1339–1340.
3. So SC, Kwack KK, Park HK, Kim JH, Shin HM, Lyu DY, et al. A case of tracheal hemangioma manifested massive hemoptysis. Tuberc Respir Dis. 1999; 47:704–708.
4. Kim HJ, Bae SY, Sung YK, Song SY, Jeon K, Koh WJ, et al. A case of tracheal capillary hemangioma in an adult. Tuberc Respir Dis. 2010; 69:385–388.
5. Kim EY, Kim TS, Han J, Kim H, Choi YS. Recurrent pulmonary capillary hemangioma: dynamic contrast-enhanced CT and histopathologic findings. Korean J Radiol. 2012; 13:350–354.
6. Werner JA, Dunne AA, Folz BJ, Rochels R, Bien S, Ramaswamy A, et al. Current concepts in the classification, diagnosis and treatment of hemangiomas and vascular malformations of the head and neck. Eur Arch Otorhinolaryngol. 2001; 258:141–149.
7. Sweetser TH. Hemangioma of the larynx. Laryngoscope. 1921; 31:797–806.
8. Rose AS, Mathur PN. Endobronchial capillary hemangioma: case report and review of the literature. Respiration. 2008; 76:221–224.
9. Park SI, Choi E, Kim YH, Park SH, Choi IC. Capillary hemangioma of the left main bronchus in an infant. Korean J Thorac Cardiovasc Surg. 2002; 35:736–739.
10. Jie S, Hong-rui L, Fu-quan Z. Brachytherapy for tracheal lobular capillary haemangioma (LCH). J Thorac Oncol. 2012; 7:939–940.
11. Park GY, Lee KY, Yoo CG, Kim YW, Han SK, Shim YS. Bronchoscopic findings of endobronchial vascular lesions in patients with haemoptysis. Respirology. 1999; 4:401–404.
12. Flick MR, Wasson K, Dunn LJ, Block AJ. Fatal pulmonary hemorrhage after transbronchial lung biopsy through the fiberoptic bronchoscope. Am Rev Respir Dis. 1975; 111:853–856.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download