Abstract
Background
Osteopontin (OPN) and carbonic anhydrase IX (CAIX), which are expressed on the surface of tumor cells, are associated with hypoxia during tumor development and progression. However, the roles of these proteins in the plasma of patients with non-small cell lung cancer (NSCLC) are poorly understood. Herein, we hypothesized that plasma OPN and CAIX levels could be used as diagnostic and prognostic tumor markers in patients with NSCLC.
Methods
Fifty-three patients with NSCLC and 50 healthy control subjects were enrolled. We selected controls without malignancy and matched them with NSCLC patient cases according to age and gender. Blood samples were collected at the time of diagnosis; the plasma levels of OPN and CAIX were measured by enzyme-linked immunosorbent assays.
Results
The plasma levels of OPN in the patients with NSCLC were significantly elevated as compared to those in the controls (p=0.016). However, there was no difference in the plasma level of CAIX between the NSCLC patients and controls. NSCLC patients with a distant metastasis had a remarkable increase in plasma OPN compared with patients without metastasis (p=0.026), but no such correlation was found for CAIX. There was no difference in overall survival rates according to the plasma level of OPN between the two groups (by Kaplan-Meier survival analysis).
Cancer is a major public health problem in many countries, and lung cancer is the world's most common leading cause of cancer death1. As there is currently no screening modality with widely accepted efficacy, most patients with lung cancer have locally advanced or metastatic disease at the time of diagnosis. Therefore, the discovery of circulating biomarkers is important for the diagnosis of lung cancer.
Tumor hypoxia affects the malignant progression of transformed cells, and the response to therapy is reduced in cells with a diminished apoptotic potential and increased metastatic ability2. Among the markers associated with tumor hypoxia, osteopontin (OPN) and carbonic anhydrase IX (CAIX) have shown elevated expression in non-small cell lung cancer (NSCLC)3. Patients with more hypoxic tumors had higher expression levels of OPN and CAIX, and there was a significant inverse correlation between tumor/normal lung pO2 and plasma OPN.
OPN is a multifunctional phosphoprotein secreted from malignant epithelial cells4. In cancer, OPN supports cell migration and protects against programmed cell death5. These functions can enhance cancer development, progression, and metastasis. OPN expression in cancer tissue is associated with tumor growth, tumor staging, and lymph node invasion for patients with NSCLC6,7. The diagnostic or prognostic value of circulating OPN has been investigated in a number of malignancies, including breast8, ovarian9, and hepatocellular carcinomas10. The few reports regarding circulating levels of OPN in NSCLC suggest that elevated circulating levels of OPN may correlate with a poor prognosis11-13.
Carbonic anhydrases are zinc metalloenzymes that catalyze the reversible hydration of carbon dioxide for pH regulation and participate in a variety of physical processes14. Fourteen isoenzymes15, including CAIX, are expressed on the surface of tumor cells and contribute to an acidic extracellular microenvironment and intracellular alkalosis, allowing tumor cells to survive under hypoxic conditions and favoring tumor growth, invasion, and development14. A high expression level of CAIX is an independent prognostic factor in early-stage NSCLC16. The association of plasma CAIX levels with cancer has been reported for a number of cancers, including renal cell carcinoma17, urogenital cancer18, and breast cancer19. However, little is known about the relationship between plasma CAIX levels and NSCLC, as only one study has been performed. Ilie et al.20 suggested that high plasma levels of CAIX may be an independent prognostic biomarker in patients with early-stage NSCLC.
The role of OPN and CAIX in the plasma of patients with NSCLC is poorly understood. We hypothesized that plasma levels of OPN and CAIX could be used as diagnostic and prognostic tumor markers in patients with NSCLC.
In this study, 53 patients who were diagnosed with NSCLC between July 2009 and December 2010 were enrolled. The diagnosis of lung cancer was confirmed by pathological methods, including percutaneous lung biopsy, bronchoscopic biopsy, metastatic lymph node biopsy, pleural biopsy, and pleural fluid cytology. We determined the stage of lung cancer using the 2007 International Association for the Study of Lung Cancer (IASLC) 7th tumor node metastasis (TNM) classification system21.
In addition, 50 healthy controls who had visited the hospital for a regular health screening were enrolled in the study. We selected controls without malignancy and matched them with NSCLC patient cases according to age (±5 years) and sex.
Blood samples were collected at the time of diagnosis before any treatment had been initiated. The samples were separated by centrifugation at 2,500 rpm for 20 minutes and the plasma stored at -80℃ until the time of analysis. Plasma levels were measured using commercially available enzyme-linked immunosorbent assay kits with specific monoclonal antibodies against OPN and CAIX (R&D Systems, Minneapolis, MN, USA). All samples were tested in duplicate.
All samples were derived from the National Biobank of Korea. This study was approved by the institutional review boards at participating centers. All subjects provided written informed consent.
The associations between plasma levels of OPN and CAIX in NSCLC patients and controls were analyzed using the chi-square test and Mann-Whitney U test. The relationships between plasma OPN and CAIX levels and smoking status were analyzed with Spearman's correlation. Receiver operating characteristic (ROC) curve analysis of plasma OPN levels was used to differentiate between NSCLC patients and controls. Kaplan-Meier survival curves were compared using the log-rank test. All analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). All tests were two-sided, with significance set at p<0.05.
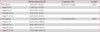
The baseline characteristics of the subjects are shown in Table 1. The mean age of the NSCLC patients was 71 years. The healthy controls and patients with NSCLC showed no differences in age, sex, or underlying disease. However, the level of cigarette smoking in the patients with NSCLC was higher than that in the controls (p<0.05) (Table 1).
A total of 31 patients had squamous cell carcinoma, while 18 had adenocarcinoma; 4 patients were nontypable. Five patients had stage I disease, two had stage II disease, 23 had stage III disease, and 23 had stage IV disease (Table 1). All patients with stage I or II disease were confirmed by surgery; of these, 15 patients (6 with stage IIIB disease and 9 with stage IV disease) were treated with supportive care. Six patients were lost to follow-up. The median follow-up period was 10 months (range, 0-30 months).
The median plasma levels of OPN were 93.07 ng/mL (range, 5.34-454.34 ng/mL) in the NSCLC patients and 48.41 ng/mL (range, 6.52-274.85 ng/mL) in the control group (Table 2). OPN levels were significantly higher in the plasma of patients with NSCLC than in the plasma of controls (p=0.016, Mann-Whitney U test). No correlation was observed between the plasma OPN level and smoking status (pack-year) (Spearman's r=0.111).
There was no significant difference in the plasma level of OPN between patients with adenocarcinoma (median, 91.87 ng/mL; range, 5.34-454.34 ng/mL) and those with squamous cell carcinoma (median, 98.56 ng/mL; range, 6.48-385.33 ng/mL).
The plasma level of OPN did not differ significantly according to TNM staging: stage I (median, 73.85 ng/mL; range, 5.34-117.85 ng/mL), stage II (median, 69.97 ng/mL; range, 9.83-130.10 ng/mL), stage III (median, 93.07 ng/mL; range, 6.52-454.34 ng/mL), and stage IV (median, 152.07 ng/mL; range, 6.48-385.33 ng/mL) (Table 2). The median plasma OPN level in patients with a distant metastasis, including stage IV (152.07 ng/mL; range, 6.48-385.33 ng/mL), was significantly elevated (p=0.026) compared with that in NSCLC patients without a distant metastasis, including stages I-III (80.64 ng/mL; range: 5.34-454.34 ng/mL). The median plasma OPN level was higher in NSCLC patients without metastasis compared with the controls (48.41 ng/mL; range, 6.52-274.85 ng/mL), but the difference was not significant (Figure 1).
The median plasma levels of CAIX were 73.36 pg/mL (range, 9.46-2,223.19 pg/mL) in the NSCLC patients and 71.18 pg/mL (range, 2.09-453.54 pg/mL) in the controls (Table 2). The plasma CAIX level did not differ between the NSCLC patients and controls, and was not correlated with smoking status (pack-year) (Spearman's r=0.155).
The plasma levels of CAIX were higher in adenocarcinoma patients (median, 109.11 pg/mL; range, 9.46-2,223.19 pg/mL) than in squamous cell carcinoma patients (median, 66.11 pg/mL; range, 18.40-261.55 pg/mL), but the difference was not significant.
There was no significant difference in the plasma level of CAIX according to TNM staging: stage I (median, 119.26 pg/mL; range, 35.54-209.64 pg/mL), stage II (median, 66.62 pg/mL; range, 48.93-84.31 pg/mL), stage III (median, 66.11 pg/mL; range, 18.40-364.13 pg/mL), and stage IV (median, 78.46 pg/mL; range, 9.46-2,223.19 pg/mL) (Table 2).
When a ROC curve was generated, the area under the curve for the discrimination of OPN in NSCLC patients and controls was 0.638 (95% confidence interval, 0.525-0.751; p=0.016) (Figure 2). At a plasma OPN level of 68.51 ng/mL, the sensitivity was 62.3% and the specificity was 76.0%. Based on this cutoff, we obtained a positive predictive value of 75.0% and a negative predictive value of 69.6%.
The relationship between the plasma OPN level and patient survival was investigated using Kaplan-Meier survival analysis for overall survival. The patients were dichotomized based on the median plasma OPN level (93.07 ng/mL). The median survival times of patients with plasma OPN levels higher and lower than the median level were 10.1 months and 7.9 months, respectively. Overall survival did not differ significantly between the two groups (p=0.301) (Figure 3).
In this study, we found that the plasma level of OPN was significantly elevated in Korean patients with NSCLC when compared with age- and sex-matched healthy controls. Moreover, the plasma levels of OPN were significantly higher in patients with a distant metastasis than in those without a distant metastasis. However, the plasma levels of CAIX did not vary between the NSCLC patients and controls.
OPN, which is produced by osteoclasts, macrophages, T cells, kidney cells, and vascular smooth muscle cells, regulates normal physiological processes, including bone resorption, wound healing, tissue remodeling, immunological responses, and vascularization, as well as various pathophysiological conditions22. OPN has been recognized as an important molecule in all stages of cancer progression, including tumor invasion, angiogenesis, and metastasis22. The role of OPN in promoting cancer involves the regulation of vascular endothelial growth factor expression through the activation of various signaling mechanisms23.
In previous studies, the median levels of OPN in patients with NSCLC have ranged from 69 to 592 ng/mL11-13,24. In Asian studies, the median OPN levels in patients with NSCLC were 86-92 ng/mL for early-stage disease and 118.3-158.2 ng/mL for advanced-stage NSCLC24. Our results (68.05 ng/mL in early-stage and 109.85 ng/mL in advanced-stage NSCLC) are consistent with those. However, in American studies, the circulating levels of OPN in patients with NSCLC (271 ng/mL in early-stage13 and 592 ng/mL in advanced-stage NSCLC11) were higher than those in Asian studies. This difference may be due to differences in subject ethnicity25. Differences in circulating OPN levels according to race should be studied further.
The circulating levels of OPN in healthy controls have only been reported in only two studies6,13. One study comprised a very small population with 25 healthy controls. In the second study, the mean plasma level of OPN was 40±2 ng/mL, which is similar to the present results (median plasma OPN level, 48.41 ng/mL). Blasberg et al.13 also reported that patients with early-stage NSCLC (n=53) had higher plasma levels of OPN compared with normal smokers. In our study, the number of patients with early-stage NSCLC (stages I and II) was too small (n=7) to show a significant difference in the plasma OPN level between patients with early-stage NSCLC and controls. Nevertheless, we showed a clear difference in the plasma level of OPN between all patients with NSCLC and the controls. Moreover, the ROC curves demonstrated that by using plasma OPN as a biomarker, patients with NSCLC could be distinguished from healthy controls with a sensitivity of 62.3% and specificity of 76.0%. Therefore, plasma OPN may be a diagnostic biomarker for differentiating patients with and without NSCLC.
To date, only two studies have reported OPN to be a useful prognostic marker of advanced NSCLC11,12. The normal value for plasma OPN has not been well known until now. Therefore, previous studies have analyzed survival according to their median plasma OPN levels11,12. We conducted survival analysis in the same way. However, our results did not show a difference in overall survival according to plasma OPN level. The patients enrolled in the two previous studies were classified as either stage IIIB with pleural metastasis or stage IV NSCLC. However, by applying the 2007 staging system21, all of these patients would now be considered to have stage IV disease. Of the patients in our study, 43.4% (23 patients) were stage IV, and we concluded that predicting survival based on the plasma level of OPN was not effective. Blasberg et al.13 reported no association between the plasma OPN level and disease stage, which strong agrees with our results. Finally, the circulating OPN level can be used only as a biomarker for advanced disease in NSCLC, and is not related to survival.
The tissue expression levels of CAIX in patients with NSCLC have been described previously, but plasma levels of CAIX in patients with NSCLC have been largely ignored. Our study makes an important contribution in this regard. In 2010, Ilie et al.20 reported that the plasma level of CAIX was higher in patients with NSCLC (mean, 45.40 pg/mL) than in healthy individuals (mean, 2.48 pg/mL), which is different from our result. As most biomarkers are influenced by age, sex, and race25, we selected age- and sex-matched controls. Although Ilie et al.20 did not provide the age or sex of their healthy controls, this may explain the difference between the study results.
Our study has several strengths. First, we used the new 2007 TNM staging system21. All previous studies have used the old TNM staging system, and many cases classified as stage III in earlier studies would now be considered stage IV. Therefore, previous studies11,12 should be re-analyzed using the new staging system21. Second, this is the first study in an Asian population to compare plasma CAIX levels between patients with NSCLC and age- and sex-matched controls.
Our study has some limitations. First, the history of cigarette smoking differed between the two groups. Some studies have reported that the sputum OPN level was elevated in patients with smoking-related interstitial lung disease26 and smoking-induced asthma27. They explained that increased OPN in sputum was associated with the accumulation of inflammatory cells such as macrophages or neutrophils. However, the relationship between circulating OPN and smoking has not been studied until now. Our results indirectly show no association between smoking status (pack-year) and the plasma OPN level by Spearman's correlation. The role of circulating OPN according to cigarette smoking status should be studied further. Second, the number of patients with early-stage NSCLC was small. Therefore, our results may not apply to patients with early-stage NSCLC. In in future, a study in patients with early-stage NSCLC must be performed. Third, we did not examine the patient death rate according to the treatment modality or cause of death.
In conclusion, a higher plasma OPN level can be a useful diagnostic biomarker for advanced NSCLC, but a higher plasma OPN level does not indicate prognosis. Additionally, circulating CAIX cannot be used as a biomarker in patients with NSCLC.
Figures and Tables
 | Figure 1Box plots depicting plasma levels of osteopontin (OPN) according to distant metastasis. The box plots indicate the levels of OPN in individual plasma samples. The box is bound above and below by the 75th and 25th percentiles, respectively. The horizontal line within the box indicates the median plasma OPN level. The upper and lower horizontal bars indicate the maximal and minimal levels, respectively. The circles show outliers. The plasma levels of OPN were elevated in patients with distant metastasis. *p<0.05 by the Mann-Whitney U test. NS: not significant. |
 | Figure 2Receiver operating characteristic curve analysis of the plasma osteopontin levels in the non-small cell lung cancer patients and controls. |
 | Figure 3Kaplan-Meier survival curves according to plasma osteopontin (OPN) levels in patients with non-small cell lung cancer (NSCLC). Overall survival curves of patients with plasma OPN levels higher or lower than the median plasma OPN level (93.07 ng/mL). The solid line indicates the cumulative survival of patients with higher OPN levels, and the dashed line indicates the cumulative survival of patients with lower OPN levels. N: number of patients. |
Acknowledgements
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (1020420). The blood samples were generously provided by the Kangwon National University Hospital Biobank. The members of the National Biobank of Korea are supported by the Ministry of Health and Welfare, Republic of Korea.
References
1. Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010; 60:277–300.
2. Brown JM, Giaccia AJ. The unique physiology of solid tumors: opportunities (and problems) for cancer therapy. Cancer Res. 1998; 58:1408–1416.
3. Le QT, Chen E, Salim A, Cao H, Kong CS, Whyte R, et al. An evaluation of tumor oxygenation and gene expression in patients with early stage non-small cell lung cancers. Clin Cancer Res. 2006; 12:1507–1514.
4. Rittling SR, Chambers AF. Role of osteopontin in tumour progression. Br J Cancer. 2004; 90:1877–1881.
5. Weber GF, Lett GS, Haubein NC. Categorical meta-analysis of Osteopontin as a clinical cancer marker. Oncol Rep. 2011; 25:433–441.
6. Hu Z, Lin D, Yuan J, Xiao T, Zhang H, Sun W, et al. Overexpression of osteopontin is associated with more aggressive phenotypes in human non-small cell lung cancer. Clin Cancer Res. 2005; 11:4646–4652.
7. Zhao B, Sun T, Meng F, Qu A, Li C, Shen H, et al. Osteopontin as a potential biomarker of proliferation and invasiveness for lung cancer. J Cancer Res Clin Oncol. 2011; 137:1061–1070.
8. Bramwell VH, Doig GS, Tuck AB, Wilson SM, Tonkin KS, Tomiak A, et al. Serial plasma osteopontin levels have prognostic value in metastatic breast cancer. Clin Cancer Res. 2006; 12(11 Pt 1):3337–3343.
9. Mrochem J, Sodowski K, Deja R, Walaszek-Gruszka A, Wojcieszek A, Kolosza Z, et al. Evaluation of selected serum protein markers as early detectors of ovarian cancer. Ginekol Pol. 2008; 79:271–275.
10. Abu El, Abdel-Aleem A, Ali A, Saber R, Shatat M, Rahem DA, et al. Diagnostic significance of plasma osteopontin in hepatitis C virus-related hepatocellular carcinoma. Ann Hepatol. 2011; 10:296–305.
11. Mack PC, Redman MW, Chansky K, Williamson SK, Farneth NC, Lara PN Jr, et al. Lower osteopontin plasma levels are associated with superior outcomes in advanced non-small-cell lung cancer patients receiving platinum-based chemotherapy: SWOG Study S0003. J Clin Oncol. 2008; 26:4771–4776.
12. Isa S, Kawaguchi T, Teramukai S, Minato K, Ohsaki Y, Shibata K, et al. Serum osteopontin levels are highly prognostic for survival in advanced non-small cell lung cancer: results from JMTO LC 0004. J Thorac Oncol. 2009; 4:1104–1110.
13. Blasberg JD, Pass HI, Goparaju CM, Flores RM, Lee S, Donington JS. Reduction of elevated plasma osteopontin levels with resection of non-small-cell lung cancer. J Clin Oncol. 2010; 28:936–941.
14. Winum JY, Scozzafava A, Montero JL, Supuran CT. Inhibition of carbonic anhydrase IX: a new strategy against cancer. Anticancer Agents Med Chem. 2009; 9:693–702.
15. Supuran CT, Briganti F, Tilli S, Chegwidden WR, Scozzafava A. Carbonic anhydrase inhibitors: sulfonamides as antitumor agents? Bioorg Med Chem. 2001; 9:703–714.
16. Kim SJ, Rabbani ZN, Vollmer RT, Schreiber EG, Oosterwijk E, Dewhirst MW, et al. Carbonic anhydrase IX in early-stage non-small cell lung cancer. Clin Cancer Res. 2004; 10:7925–7933.
17. Pena C, Lathia C, Shan M, Escudier B, Bukowski RM. Biomarkers predicting outcome in patients with advanced renal cell carcinoma: results from sorafenib phase III Treatment Approaches in Renal Cancer Global Evaluation Trial. Clin Cancer Res. 2010; 16:4853–4863.
18. Hyrsl L, Zavada J, Zavadova Z, Kawaciuk I, Vesely S, Skapa P. Soluble form of carbonic anhydrase IX (CAIX) in transitional cell carcinoma of urinary tract. Neoplasma. 2009; 56:298–302.
19. Muller V, Riethdorf S, Rack B, Janni W, Fasching PA, Solomayer E, et al. Prospective evaluation of serum tissue inhibitor of metalloproteinase 1 and carbonic anhydrase IX in correlation to circulating tumor cells in patients with metastatic breast cancer. Breast Cancer Res. 2011; 13:R71.
20. Ilie M, Mazure NM, Hofman V, Ammadi RE, Ortholan C, Bonnetaud C, et al. High levels of carbonic anhydrase IX in tumour tissue and plasma are biomarkers of poor prognostic in patients with non-small cell lung cancer. Br J Cancer. 2010; 102:1627–1635.
21. Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007; 2:706–714.
22. Ahmed M, Behera R, Chakraborty G, Jain S, Kumar V, Sharma P, et al. Osteopontin: a potentially important therapeutic target in cancer. Expert Opin Ther Targets. 2011; 15:1113–1126.
23. Chakraborty G, Jain S, Behera R, Ahmed M, Sharma P, Kumar V, et al. The multifaceted roles of osteopontin in cell signaling, tumor progression and angiogenesis. Curr Mol Med. 2006; 6:819–830.
24. Chang YS, Kim HJ, Chang J, Ahn CM, Kim SK, Kim SK. Elevated circulating level of osteopontin is associated with advanced disease state of non-small cell lung cancer. Lung Cancer. 2007; 57:373–380.
25. Wagner PD, Srivastava S. New paradigms in translational science research in cancer biomarkers. Transl Res. 2012; 159:343–353.
26. Prasse A, Stahl M, Schulz G, Kayser G, Wang L, Ask K, et al. Essential role of osteopontin in smoking-related interstitial lung diseases. Am J Pathol. 2009; 174:1683–1691.
27. Hillas G, Loukides S, Kostikas K, Simoes D, Petta V, Konstantellou E, et al. Increased levels of osteopontin in sputum supernatant of smoking asthmatics. Cytokine. 2013; 61:251–255.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download