Abstract
A 62-year-old man with a chronic cough presented with atelectasis of the left upper lobe on chest X-ray. Chest computed tomography showed an atelectasis in the left upper lobe with bronchial wall thickening, stenosis, dilatation, and mucoid impaction. We performed bronchoscopy and found a well-circumscribed mass on the left upper lobe bronchus. The mass was removed by flexible bronchoscopy using an electrosurgical snare and diagnosed with lipoma. An endobronchial lipoma is a rare benign tumor that can be treated by a surgical or endoscopic approach. We report the successful removal of endobronchial lipoma via flexible bronchoscopic electrosurgical snare.
Benign tumors originating from the tracheobronchial tree are very uncommon, especially incidence of endobronchial lipoma in all lung tumors ranges from only 0.1% to 0.5% in all lung tumors1. Lipomas are slow-growing tumors that can remain clinically silent for a prolonged period. When symptoms develop, they are usually manifest as recurrent infections, which, if remaining undiagnosed over time, can lead to bronchiectasis secondary to endobronchial obstruction2. Clinical manifestations of endobronchial lipoma are presented variably, cough, wheezing, hemoptysis, chest pain, atelectasis in chest X-ray, recurrent pneumonia, and, rarely, empyema3-5. The removal of endobronchial lipoma can be achieved by surgical or bronchoscopic methods; generally through rigid bronchoscopy2,6. We present a case of endobronchial lipoma that was successfully removed via flexible bronchoscopy using an electrosurgical snare.
A 62-year-old man visited the respiratory outpatient department with symptoms of a chronic cough and atelectasis of the left upper lobe on chest X-ray. The patient had no specific past history and family history. Physical examination revealed clear breath sound without rales and wheezing sound. Laboratory tests were within normal range. Pulmonary function tests revealed a mild obstructive pattern (forced expiratory volume 1 second [FEV1], 96%; FEV1/forced vital capacity, 69%). A chest computed tomography (CT) revealed atelectasis, bronchial wall thickening, stenosis, dilatation, and mucoid impaction in the left upper lobe, without definite mass lesion (Figure 1A, C). Lymph node enlargements were apparent in the right hilum and left lower paratrachea. Two focal calcified granuloma were seen in the right lung.
Flexible bronchoscopy was performed and revealed a well-circumscribed mass on the left upper lobe bronchus. Biopsy was done and showed subepithelial mature adipose tissue. We tried to remove a mass with flexible bronchoscopic electrosurgical snare (Figure 2). After removal of the mass, a base remained on left upper lobe B1+B2. An additional coagulation using snare tip was carried out to the remove residual tumor base and to control the bleeding.
The patient was discharged and then followed up in the outpatient department. After 1.5 months, a follow-up bronchoscopy (Figure 3) and chest CT (Figure 1B, D) revealed remaining mass in left upper lobe B2. The remained mass was removed completely by forceps. On follow-up CT scans, atelectastasis was remained but no mass lesion was present in left upper lobe. The patient has been followed up in outpatient department regularly.
There are many methods to remove the endobronchial lipoma including surgical resection and endoscopic excision7,8. The majority of lipomas occur in the first three subdivisions of the tracheobronchial tree where there is abundant cartilage and adipocytes. Also, lipomas are poorly vascularized tumors. Therefore, they are amenable to endoscopic management both for diagnosis and treatment2,3. Endoscopic removal of lipoma includes laser ablation, electrocauterization, cryo-recanalization, and, as seen our case report, electrosurgical snaring9. Removal of endobronchial lipoma using flexible bronchoscopic electrosurgical snaring has some advantages. It does not require general anesthesia, can diagnose pathology and remove the mass at the same time, and is less invasive than surgical resection. But if there is massive bleeding during procedure, it is difficult to control bleeding and protect the airway than rigid bronchoscopy10.
Muraoka et al.1 reviewed the cases of endobronchial lipoma reported in Japan. Forty patients underwent surgical resection: four pneumonectomies, 24 lobectomies, eight bilobectomies, and four resections by bronchotomy. Seventeen patients have undergone bronchoscopic treatment: seven patients received Nd-YAG laser therapy, five tumors were removed by electrosurgical snaring forceps via flexible bronchoscope and five patients received a combined therapy using both laser techniques and polypectomy snares. No tumor recurrence was reported for these 17 patients after the bronchoscopic procedure. Bronchoscopic electrocautery, compared with Nd-YAG laser therapy, is the more simple and cost-effective, produces less significant bronchial stenosis and causes limited damage to the bronchial mucosa, although the outcome of both treatments are virtually the same11-14. But, in spite of several benefits of bronchoscopic resection, surgical resection is indicated for some patients. The conditions under which surgical resection is preferred are difficulty of definite diagnosis and possible complicated malignant tumor, peripheral destructive lung disease due to long-term atelectasis or pneumonia, extrabronchial growth or subpleural lipomatous disease, or expected technical difficulties during the bronchoscopic procedure due to multidirectional development of the tumor1.
In our opinion, there are differences between bronchoscopic and gastrointestinal endoscopic tumor removal by snare. On gastrointestinal endoscopy, it is possible that the tumor base can be separated by injection of dye fluid, so complete removal of a tumor including the base can be accomplished. But in the case of bronchoscopic tumor removal, it is difficult to apply of the method used in gastrointestinal endoscopy. Thus, we consider that a tumor should be initially removed by the snare as much as possible, with the remaining tumor base being coagulated by the snare tip or by argon-plasma coagulation.
In this report, we removed successfully endobronchial lipoma by electrosurgical snaring via flexible bronchoscopy. Based on this case and literature review, flexible bronchoscopic resection could be considered as the first option for the treatment of bronchial lipoma.
Figures and Tables
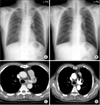 | Figure 1Chest X-ray and chest computed tomography (CT) image. (A) At admission, chest X-ray revealed atelectasis. (B) After 1.5 months, chest X-ray showed improvement of atelectasis. (C) At admission, chest CT revealed mucoid impaction in left upper lobe bronchus. (D) After 1.5 months, chest CT showed no definite mass lesion in the left upper lobe bronchus. |
 | Figure 2Datails of the procedure. (A) Endoscopic electrosurgical snare. (B) Bronchoscopic finding of endobronchial lipoma. The left upper lobe bronchus was obstructed with a round mass, which has a smooth, yellow colored surface. (C) Just after the mass was removed by electrosurgical snare, the left upper lobe bronchus was reopened. The tumor base was remained. (D) The resected endobronchial tumor. |
References
1. Muraoka M, Oka T, Akamine S, Nagayasu T, Iseki M, Suyama N, et al. Endobronchial lipoma: review of 64 cases reported in Japan. Chest. 2003. 123:293–296.
2. Nassiri AH, Dutau H, Breen D, Colchen A, Quiot JJ, Nguyen B, et al. A multicenter retrospective study investigating the role of interventional bronchoscopic techniques in the management of endobronchial lipomas. Respiration. 2008. 75:79–84.
3. Iwabuchi H, Kamura T, Tanaka M, Kato H. A case of endobronchial lipoma. Diagn Ther Endosc. 1999. 5:263–267.
4. Cao D, Sun Y, Yang S. Endobronchial lipoma: an unusual cause of bronchial obstruction. Case Rep Med. 2011. 2011:939808.
5. Ouadnouni Y, Bouchikh M, Bekarsabein S, Achir A, Smahi M, Msougar Y, et al. Endobronchial lipoma a rare cause of pleural empyema: a case report. Cases J. 2009. 2:6377.
6. Choi JC, Yu CM, Ryu YJ, Jeon K, Choi KA, Kwon OJ, et al. The role of endoscopic surgery for completely obstructive endobronchial benign tumor. Korean J Intern Med. 2006. 21:15–19.
7. Hurt R. Benign tumours of the bronchus and trachea, 1951-1981. Ann R Coll Surg Engl. 1984. 66:22–26.
8. MacArthur CG, Cheung DL, Spiro SG. Endobronchial lipoma: a review with four cases. Br J Dis Chest. 1977. 71:93–100.
9. Lamprecht B, Hutarew G, Porsch P, Wegleitner B, Studnicka M. Successful bronchoscopic cryorecanalization in a case of endobronchial lipoma. Diagn Ther Endosc. 2011. 2011:845686.
10. Landa JF. Indications for bronchoscopy. Chest. 1978. 73:5 Suppl. 686–690.
11. Boxem T, Muller M, Venmans B, Postmus P, Sutedja T. Nd-YAG laser vs bronchoscopic electrocautery for palliation of symptomatic airway obstruction: a cost-effectiveness study. Chest. 1999. 116:1108–1112.
12. van Boxem AJ, Westerga J, Venmans BJ, Postmus PE, Sutedja G. Photodynamic therapy, Nd-YAG laser and electrocautery for treating early-stage intraluminal cancer: which to choose? Lung Cancer. 2001. 31:31–36.
13. Bolliger CT, Sutedja TG, Strausz J, Freitag L. Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J. 2006. 27:1258–1271.
14. Choi SH, Kang JY, Joo YB, Kim SK, Mo EY, Lee SH, et al. An endobronchial lipoma treated by bronchoscopic excision. Korean J Med. 2011. 80:337–342.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download