Abstract
We present a case of congenital cystic adenomatoid malformation (CCAM) in a 25-year-old male who was presented with chronic cough. Chest radiography revealed an abnormal mass-like shadow in the right lower pulmonary zone. A contrast enhanced computed tomography showed an 11 cm solid, cystic mixed mass on the right lower lobe. A right lower lobectomy was performed by video-assisted thoracoscopic surgery without complications. The gross specimen showed a massive cavitation with multiloculated cysts of varying size, consistent with CCAM, along with noticeable granulomatous inflammation. Non-tuberculosis mycobacteria were isolated from a bronchial wash specimen, and the resected tissue homogenates were positive for Mycobacterium avium-intracellulare complex by polymerase chain reaction.
Congenital cystic adenomatoid malformation (CCAM) is a rare developmental anomaly of the terminal respiratory structures with an incidence of 1 in 10,000 to 1 in 35,000 births1. It was first described as a distinct disease by Ch'In and Tang in 19492. The lesion is almost always unilateral and may occur in any lobe. The clinical presentations of CCAM include acute respiratory distress, recurrent pulmonary infections, lung abscess, pneumothorax, or hemoptysis. Most cases are diagnosed antenatally or in neonates and infants who present with severe respiratory distress or pulmonary infections in the affected lung. Occasionally, CCAM remains unrecognized until adolescence or adulthood. Recurrent bacterial infections are a frequent feature of CCAM in adults. Here, we report a case of CCAM associated with a Mycobacterium avium-intracellulare complex (MAC) infection.
A 25-year-old male without a history of smoking presented with a 1-week history of cough and right-sided back pain when coughing. The patient had a history of one hospital admission due to pneumonia approximately ten years prior to the current presentation and complained of intermittent cough over the intervening ten years.
A physical examination identified decreased breathing sounds over the right lower lung without other findings. A complete blood count test, liver function test and urine analysis were normal. His erythrocyte sedimentation rate was 61 mm/hr and his high-sensitivity C-reactive protein was 3.86 mg/dL. Chest radiography showed an abnormal mass-like shadow in the right lower lung (Figure 1A). Contrast-enhanced computed tomography (CT) revealed an 11 cm solid, cystic mixed mass in the right lower lobe without a feeding vessel from the descending aorta (Figure 1B). Bronchoscopy disclosed purulent secretion from the posterior basal segmental bronchus of the right lower lobe. A pulmonary function test was normal.
Subsequently, the patient underwent a right lower lobectomy by video-assisted thoracoscopic surgery. A macroscopic examination showed a massive cavitation with multiloculated cysts of varying size within the lesion and pleural fibrosis (Figure 2). Microscopically, the specimen consisted of multiple cysts (Figure 3A) which were lined by cuboidal-to-ciliated pseudostratified columnar epithelium, and some cysts contained extensive secondary inflammation (Figure 3B). These histological features were consistent with typical type I CCAM. In addition, a microscopic examination revealed a noticeable caseous granulomatous inflammation in the cyst walls (Figure 3A). The necrotic center was surrounded by epithelioid histiocytes and then by a rim of lymphocytes (Figure 3C). Forty colony forming units of non-tuberculosis mycobacterium (NTM) were isolated from a bronchial wash specimen. Furthermore, resected lung tissue homogenates were positive for MAC by real-time polymerase chain reaction (Figure 3D). The postoperative course was uneventful without anti-mycobacterial treatment. Two years after surgery, chest radiography showed a well-expanded right lung without lesions.
CCAM is a rare developmental, non-hereditary, hamartomatous abnormality of the lower respiratory tract first described in 19492. It occurs sporadically and is not related to genetic predisposition, gender predilection, or maternal factors such as race, age, or environmental exposures. Stocker et al.3 suggested a new name, congenital pulmonary airway malformation, and classified CCAM into five types based on the site of the defect in the tracheobronchial tree. Type I CCAM is the most common subtype and consists of a single or multiple large epithelial-lined cysts. The walls of the cysts contain prominent smooth muscle and elastic tissue and mucus-producing cells are occasionally present3.
The pathogenesis of CCAM is uncertain but may include an imbalance between cell proliferation and apoptosis during organogenesis4. Affected patients may present with symptoms, including cough, dyspnea, hemoptysis, and respiratory distress, or remain asymptomatic. The typical manifestations include progressive respiratory distress in the newborn and recurrent pulmonary infections in older children.
The majority of cases are identified by prenatal ultrasound examinations. Additional prenatal magnetic resonance imaging may help to distinguish CCAM from other congenital lesions. A postnatal diagnosis can usually be made using plain radiography. Chest CT scans may be helpful for confirming the diagnosis in cases that are confusing. The differential diagnosis of CCAM includes bronchopulmonary sequestration, a congenital diaphragmatic hernia, a bronchogenic cyst, congenital lobar emphysema, and pneumatoceles. The most frequent complication of CCAM is recurrent or persistent pulmonary infection. Other complications include hemopneumothorax, hemoptysis, and chronic cough. CCAM has been associated with the development of malignancies, such as bronchioloalveolar carcinoma5, adenocarcinoma in aged6, and pleuropulmonary blastoma7. Surgical resection of the affected part of the lung is the treatment of choice, and this prevents recurrent infections and malignant transformation.
Pulmonary NTM infection usually occurs in patients with destroyed lungs, including those with chronic obstructive lung disease, pulmonary tuberculosis, bronchiectasis, or pneumonoconiosis. While NTM infection is known to occur commonly in old age, NTM infection occurs in destroyed lung caused by CCAM despite young age in our patient.
A few case reports have detailed NTM infection in congenital lung lesions such as bronchogenic cysts8 and pulmonary sequestration9-11, and surgical resections were performed in all cases with or without anti-mycobacterial medication. However, NTM has never been described in the etiology of an infected CCAM. To our knowledge, our patient is the first reported case of a CCAM combined with MAC disease. Surgical resection is the preferable treatment for the exact diagnosis and immediate removal of the infectious focus, thus preventing complications related to the infection or the malformation itself.
Figures and Tables
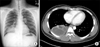 | Figure 1(A) A chest radiograph showing increased haziness in the right lower lobe. (B) A thoracic computed tomography scan performed at the same time showing an 11 cm solid, cystic mixed mass in the right lower lobe without feeding vessels from the descending aorta. |
 | Figure 2A cutting plane of the resected lung specimen shows massive cavitation with multiloculated cysts of varying size within the lesion. |
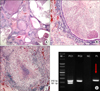 | Figure 3(A) The lesion consists of multiple cysts with caseous granulomas and inflamed granulation tissue (H&E stain, ×40). (B) The cysts are lined by cuboidal-to-ciliated pseudostratified columnar epithelium (H&E stain, ×100). (C) A marked caseous granuloma is shown, and the necrotic center is surrounded by epithelioid histiocytes (H&E stain, ×100). (D) Electrophoresis of the polymerase chain reaction product. M: size marker; PC 1: positive control (Kit-positive sample); PC 2: positive control (Mycobacterium avium-intracellulare complex); NC: negative control; Pt: patient sample. |
References
1. Laberge JM, Flageole H, Pugash D, Khalife S, Blair G, Filiatrault D, et al. Outcome of the prenatally diagnosed congenital cystic adenomatoid lung malformation: a Canadian experience. Fetal Diagn Ther. 2001. 16:178–186.
2. Ch'In KY, Tang MY. Congenital adenomatoid malformation of one lobe of a lung with general anasarca. Arch Pathol (Chic). 1949. 48:221–229.
3. Stocker JT, Madewell JE, Drake RM. Congenital cystic adenomatoid malformation of the lung: classification and morphologic spectrum. Hum Pathol. 1977. 8:155–171.
4. Fromont-Hankard G, Philippe-Chomette P, Delezoide AL, Nessmann C, Aigrain Y, Peuchmaur M. Glial cell-derived neurotrophic factor expression in normal human lung and congenital cystic adenomatoid malformation. Arch Pathol Lab Med. 2002. 126:432–436.
5. Kaslovsky RA, Purdy S, Dangman BC, McKenna BJ, Brien T, Ilves R. Bronchioloalveolar carcinoma in a child with congenital cystic adenomatoid malformation. Chest. 1997. 112:548–551.
6. Benouaich V, Marcheix B, Begueret H, Brouchet L, Velly JF, Jougon J. Malignancy of congenital cystic adenomatoid malformation of lung in aged. Asian Cardiovasc Thorac Ann. 2009. 17:634–636.
7. Nur S, Badr R, Sandoval C, Brudniki A, Yeh A. Syndromic presentation of a pleuropulmonary blastoma associated with congenital cystic adenomatoid malformation: a case report. J Pediatr Surg. 2007. 42:1772–1775.
8. Lin SH, Lee LN, Chang YL, Lee YC, Ding LW, Hsueh PR. Infected bronchogenic cyst due to Mycobacterium avium in an immunocompetent patient. J Infect. 2005. 51:e131–e133.
9. Sparks JD, Das BB, Eid NS, Austin EH, Recto M. Atypical mycobacterial infection in sequestrated lung in an infant presenting with chronic pneumonitis and recurrent wheezing. Congenit Heart Dis. 2008. 3:284–287.
10. Mooney LR, Brown JW 3rd, Saunders RL Jr. Intralobar pulmonary sequestration infected with a mycobacterium of the Battey-avium complex. Chest. 1975. 68:594–595.
11. Shiota Y, Arikita H, Aoyama K, Horita N, Hiyama J, Ono T, et al. Pulmonary sequestration associated by Mycobacterium intracellulare infection. Intern Med. 2002. 41:990–992.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download