Abstract
Mucormycosis is a rare fungal disease that holds a fatal opportunistic fungal infection in diabetes mellitus, hematological malignancy, and immunocompromised host. Isolated pulmonary mucormycosis is extremely rare. Optimal therapy is a combined medical-surgical approach and a management of the patient's underlying disease. Herein, we report a case-study of isolated pulmonary mucormycosis which was being presented as multiple lung nodules in a patient with no underlying risk factors. Considering that the patient had poor pulmonary functions, we treated him with only antifungal agent rather than a combined medical-surgical approach. After treatment with antifungal agent for six months, the nodules of pulmonary mucormycosis were improved with the prominent reductions of size on the computed tomography.
Mucormycosis is a life-threatening fungal infection which occurs in patients with diabetes mellitus, hematological malignancy. Although the infection commonly begins by invading the respiratory tract, isolated pulmonary mucormycosis is extremely rarely reported1,2. Typically an airborne infection, mucormycosis is able to extent to the whole body by invading alveolar blood vessel after germinating in paranasal sinuses3. Isolated pulmonary mucormycosis is rare, and usually occurs in the patients with diabetes mellitus, hematological malignancy or cancer undergoing induction chemotherapy4-7.
In this case reports, we report isolated pulmonary mucormycosis that arose as multiple nodule in health patient without apparent immune deficiency which was suspected as lung cancer.
A 52-year-old male presented to our hospital with a chief complaint of sputum. Productive cough with yellowish sputum for two months, four pulmonary nodule in both lungs which was detected in chest computed tomography (CT).
Using inhalers (tiopropium, salmeterol/fluticasone) because of chronic obstructive pulmonary disease (COPD) which was diagnosed 15 years ago. Seven years ago, he received occasionally a intravenous steroids because of COPD flare-ups which occurs one or two time. Pulmonary tuberculosis had been treated for three-years medical care in 13 years ago. Hepatitis C was diagnosed in 10 years ago.
His vital signs were within the normal range. There was no lymphadenopathy in the cervical, axillary, or inguinal regions. His had barrel chest. On auscultation of the chest, a coarse breathing sound with wheezing in left upper lung fields was heard.
Laboratory data were within the normal range. Blood glucose was 116 mg/dL. HbA1c was 6.1%. Hepatitis C virus antibody test was positive. Human immunodeficiency virus antigen and antibody were negative, Paragonimus antibody and Aspergillus antigen were negative.
We confirmed no endobronchial lesion by bronchoscopy. The bronchoscopic washing specimen was negative for the acid-fast bacilli smear and culture test, and also for the microbial and fungal culture test. A transcutaneous needle biopsy of the nodule at left lower lobe showed thick fungal hyphe with right-angle branching, highly suggestive for mucormycosis (Figure 3). Because the patient was immunocompetent, we screened other affected lesion. However brain magnetic resonance imaging and nasal endoscopy showed no apparent lesion.
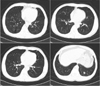
The patient was started on amphotericin B. Surgical resection of the affected lobe was not possible treatment option, because pulmonary function test showed that forced expiratory volume in one second of the patient was 45%. Amphotericin B was used during 1 week and discontinued after discharge. Posaconazole oral suspension was started for home treatment. Total treatment duration is 3 months. After treatment, the chest CT in the follow-up showed that the size of the nodules was reduced (Figure 4). After the end of the treatment for 3 months, chest radiography revealed no definitive relapse of mucormycosis (Figure 5).
Pulmonary mucormycosis is the one of a fatal opportunistic fungal infection in immunocompromised host. The infection was accompanied by a high mortality rate (50-70%)2,8. Although fever and cough are mainly reported as the main symptom of pulmonary mucormycosis, those are not specific for the infection. Hemoptysis is also observed, because mucormycosis has a high affinity for invading blood vessels. Although those symptoms and signs manifest chronically over one month, massive hemoptysis is fatal for a patient. Therefore, proper diagnosis and treatment for the infection are needed9. Sputum culture which is non-invasive test for fungal infection is not possible for a patient, if there was no productive cough. A resected specimen is often not suitable for diagnosis, because necrosis is main portion of the lesion. Without suspecting, the fungal culture test of specimen is not often done in the laboratory. Above factors are the obstacles for diagnosis of the mucormycosis infection3,9. Although a chest radiography has no specific sign for mucormycosis, unilateral infiltrate in upper lobe are mainly reported. Because the air-crescent sign in chest radiography is the sign of massive fatal hemoptysis which is cause of the death, careful assessments are needed9. The patient in this case report was immunocompetent, and has multiple nodules in both lower lobes, which are not common sign of the pulmonary mucormycosis. Therefore, the nodules could be mistaken for lung cancer.
The main principles of the therapy for mucormycosis are management of the patient's underlying disease and a combined medical-surgical approach. The motality rate of the mucormycosis is reported as 50%, and that of pulmonary mucormycosis is reported up to 80%. Surgical resection of invaded lobe and anti-fungal agent are required for the pulmonary mucormycosis accompanied with massive hemoptysis3,8. However, the patient in this case report has the affected lesion in both side of lung and the low pulmonary function, surgical resection was not possible. Medical approach, combining amphotericin B and posaconazole oral suspension, was successfully reduced the size of the affected lesion.
Because it is rare that isolated pulmonary mucormycosis occur as the nodules in chest radiography without immunodeficiency, the proper diagnosis and treatment was not possible without suspecting the fungal infection in the transcutaneous biopsy. The important negative factor for the good prognosis in fungal infection is the delayed diagnosis and treatment9. We confirmed that medical approach using posaconazole oral suspension without surgical resection and long-term hospitalization is suitable treatment for the immunocompetent patient with pulmonary mucormycosis.
Figures and Tables
Figure 2
Computed tomography of chest showed three long nodules in lower left lobe of lung and one lung nodule in lower right lobe.
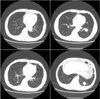
Figure 3
Pathological findings of lung tissue are shown as thick, irregular and non-septated fungal hyphaes with right-angle branching in hematoxylin and eosin stain (A, ×400) and Gomori's methenamine silver stain (B, ×400).

References
1. Butala A, Shah B, Cho YT, Schmidt MF. Isolated pulmonary mucormycosis in an apparently normal host: a case report. J Natl Med Assoc. 1995; 87:572–574.
2. Ibrahim AS, Spellberg B, Walsh TJ, Kontoyiannis DP. Pathogenesis of mucormycosis. Clin Infect Dis. 2012; 54:Suppl 1. S16–S22.
3. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 2012; 54:Suppl 1. S23–S34.
4. Kim TJ, Park CY, Jin YG, Park KE, Her KM, Kim YH, et al. A case of pulmonary mucormycosis associated uncontrolled diabetes mellitus. Korean J Med. 1997; 53:Suppl 3. S792–S796.
5. Lee SJ, Yoon SJ, Kim EJ, Cha SI, Park JY, Jung TH, et al. A case of pulmonary mucormycosis complicated by pneumomediastinum and subcutaneous emphysema after chemotherapy in a patient with small cell lung cancer. Korean J Med. 2007; 72:551–557.
6. Pagano L, Offidani M, Fianchi L, Nosari A, Candoni A, Piccardi M, et al. Mucormycosis in hematologic patients. Haematologica. 2004; 89:207–214.
7. Cho YJ, Kang MH, Kim HS, Jeong YY, Jang IS, Kim HC, et al. A case of angio-invasive pulmonary mucormycosis with uncontrolled diabetes mellitus. Tuberc Respir Dis. 2008; 64:451–455.
8. Spellberg B, Kontoyiannis DP, Fredricks D, Morris MI, Perfect JR, Chin-Hong PV, et al. Risk factors for mortality in patients with mucormycosis. Med Mycol. 2012; 50:611–618.
9. Hamilos G, Samonis G, Kontoyiannis DP. Pulmonary mucormycosis. Semin Respir Crit Care Med. 2011; 32:693–702.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download