This article has been
cited by other articles in ScienceCentral.
Abstract
Aspergillus causes a variety of clinical syndromes in the lung including tracheobronchial aspergillosis, invasive aspergillosis, chronic necrotizing pulmonary aspergillosis, allergic bronchopulmonary aspergillosis, and aspergilloma. Aspergilloma usually results from ingrowths of colonized Aspergillus in damaged bronchial tree, pulmonary cyst or cavities of patients with underlying lung diseases. There are a few reports on endobronchial aspergilloma without underlying pulmonary lesion. We have experienced a case of endobronchial aspergilloma associated with foreign body developed in an immunocompetent patient without underlying lung diseases. A 59-year-old man is being hospitalized with recurring hemoptysis for 5 months. X-ray and computed tomography scans of chest showed a nodular opacity in superior segment of left lower lobe. Fiberoptic bronchoscopy revealed an irregular, mass-like, brownish material which totally obstructed the sub-segmental bronchus and a foreign body in superior segmental bronchus of the lower left lobe. Histopathologic examinations of biopsy specimen revealed fungal hyphae, characteristic of Aspergillus species.
Go to :

Keywords: Aspergillosis, Foreign Bodies, Immunocompetence
Introduction
Aspergillosis is extensive, ranging from allergic reactions to colonization of preexisting pulmonary cavities to invasion and destruction of lung tissue with pyemic spread to brain, skin, and other organs and rapid death. Aspergilloma is mass of fungal mycelia that grow in preexisting lung cavities
1. It is composed of hyphae of
Aspergillus, fibrin, mucus, inflammatory cells, blood, and epithelial cell components
2. Aspergilloma which occurs in immunocompetent patient without underlying cavitary lesion, is undistinguishable according to conventional classification
3. There are a few reports of endobronchial aspergilloma without underlying pulmonary lesion
4-
6.
We experienced a case of endobronchial aspergilloma associated with foreign body via fiberoptic bronchoscopy in immunocompetent patient without underlying disease who visited with recurrent hemoptysis. We report this case with review of literatures.
Go to :

Case Report
A 59-year-old man visited with recurrent hemoptysis for 5 months. He was a never-smoker and had no underlying disease. Patient had aspiration history of chicken bone 3 years ago, but no loss of consciousness. On admission, he presented with 110/70 mm Hg of blood pressure, 75 beats per minute of heart rate, 20 breaths per minute of respiratory rate, 36.0℃ of body temperature. Lymph node in neck was not palpated. Physical examination of chest revealed no crackle or wheezing. Complete blood count results were white blood cell 6,800/mm3 (neutrophils 56%, lymphocytes 33%, monocytes 8%, and eosinophils 3%), hemoglobin 15.4 g/dL, and platelet 195,000/mm3. Routine blood chemistries and tumor makers were within normal limits. Human immunodeficiency virus antibody test was negative.
Chest X-ray showed a nodular opacity in left hilar field (
Figure 1A). Computed tomography (CT) scan of chest revealed a 2.4×1.8 cm-sized spiculated mass and surround small nodular opacities in superior segment of left lower lobe (
Figure 1B). Fiberoptic bronchoscopy re vealed an irregular mass-like, brownish material which totally obstruct subsegmental bronchus (
Figure 2A) and a foreign body in superior segmental bronchus of left lower lobe (
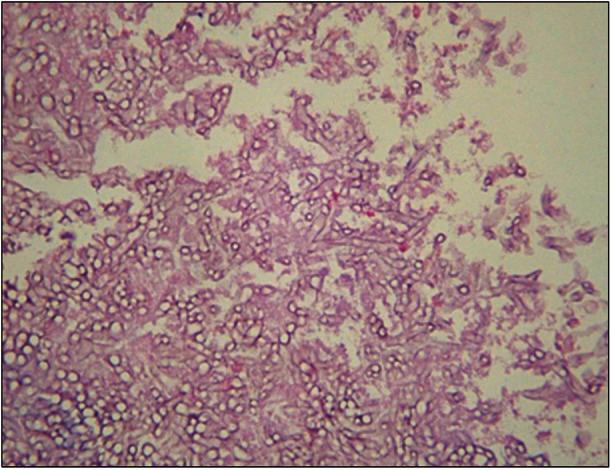
Figure 2B). We repeatedly tried removing a foreign body, but could not succeed because it was impossible to be held by forceps or snare within narrow lumen. Histopathologic examination of bronchoscopic biopsy specimen showed mostly fungal hyphae (
Figure 3).
 | Figure 1(A) A chest X-ray showed a nodular opacity in left hilar field. (B) A computed tomography scan of chest showed a 2.4×1.8 cm-sized spiculated nodule and surrounding nodular opacities in superior segment of lower left lobe. 
|
 | Figure 2(A) Fiberoptic bronchoscopy reveals an irregular, mass-like, brownish material which totally obstructed the sub-segmental bronchus in superior segmental bronchus of the lower left lobe. (B) A foreign body was noted in other sub-segmental bronchus quite near the aspergilloma. 
|
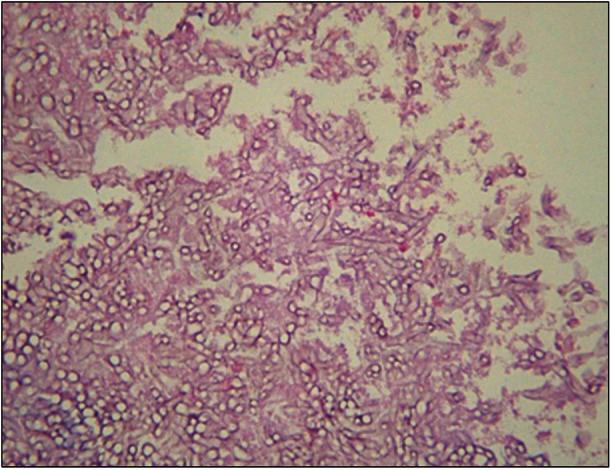 | Figure 3Histopathologic examination showed numerous hyphae branching with approximately 45° angle, characteristic of Aspergillus species (H&E stain, ×100). 
|
Go to :

Discussion
Aspergillus causes disease of wide clinical diversity that usually can be classified into 5 categories. Tracheobronchial aspergillosis has a spectrum of disease ranging from colonization to destructive tracheobronchitis almost exclusively in immunosuppressed individuals. Allergic bronchopulmonary aspergillosis affects patients with asthma and bronchiectasis. Chronic necrotizing pulmonary aspergillosis is locally invasive and occurs in modestly immunocompromised patients with underlying lung disease. Invasive aspergillosis occurs in patients with defects in phagocyte number, function, or both. Finally, aspergilloma occurs when fungus colonizes and grows in existing pulmonary cavities
1. Many cavitary lung diseases such as tuberculosis, sarcoidosis, cavitary tumor, pulmonary fibrosis, bronchiectasis, and histoplasmosis are complicated by aspergilloma. Pulmonary tuberculosis is the most common cause of cavities facilitating development of aspergilloma
2.
Aspergilloma may develop in healthy lungs. This is understood that
Aspergillus species colonizing respiratory tract can secrete digestive enzymes into the surrounding lung parenchyme and create space for growth of fungus ball
7. In immunocompetent patients, aspergilloma requires a nidus or structural changes that induce airflow stasis to colonize bronchial lumen. Ma et al.
8 reported that 4 patients without underlying lung disease had an endobronchial lesion similar to foreign body such as broncholith, lung cancer, and granulation tissue or suture material of anastomosis site after pulmonary resection. They suggested that these endobronchial lesions may act as a nidus for colonization of
Aspergillus. Eom et al.
5 and Kim et al.
6 also suggested that foreign body such as endobronchial calcified lesion may act as a nidus. Our patient had no previous surgery or endobronchial calcified lesion. We found a foreign body within bronchus via fiberoptic bronchoscopy, but which was locating within the other subsegmental bronchus of same segmental bronchus. Because patient had not any other causable lesion and a foreign body was locating quite near aspergilloma, we presumed that this foreign body might act as a nidus of
Aspergillus growth. We could not succeed in removing a foreign body, and need to be attentive that a remaining foreign body contains some possibility of acting as a nidus once again.
Quoix et al.
9 reported a case of endobronchial aspergillosis associated with carcinoid tumor, and Ham et al.
10 reported a case of lung cancer obscured by endobronchial aspergilloma. Because our case showed a spiculated mass appearance, he underwent positron emission tomography to evaluate possibility of lung malignancy. Positron emission tomography suggested possibility of benign inflammatory process. CT scan of chest followed up 3 months later revealed decreased size of nodule to 2.1×1.6 cm. We planned follow-up of CT scan to completely exclude lung cancer.
Optimal treatment of endobronchial aspergilloma has not yet been established. In asymptomatic patients, no therapy is warranted. In cases of mild hemoptysis as same as our patient, medical therapy with bed rest, humidified oxygen, cough suppressants, and postural drainage is helpful. There is no consistent evidence that aspergilloma responds to systemic administration of antifungal agents, and these drugs rarely achieve minimal inhibitory concentrations within lung cavities
11. Inhaled, intracavitary, and endobronchial instillations of antifungal agents have been tried with no consistent success
12. Surgical approach needs to be considered in patients with massive hemoptysis and adequate pulmonary reserves. We suggest that therapeutic decisions in this disease must be individualized to take into account patient's overall health and risks attendant with each treatment modality.
As our case study, endobronchial aspergilloma may occur in immunocompetent patient without underlying lung disease. It requires a nidus for colonization and proliferation of Aspergillus. We think that intrabronchial foreign body may act as a nidus for Aspergillus growth.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download