Abstract
Background
Nontuberculous mycobacteria (NTM) are considered opportunistic pathogens, and several species of NTM are associated with human diseases that typically involve the pulmonary, skin/soft tissue, or lymphatic systems; such infection may also cause disseminated diseases. Recent studies have reported increasing rates of NTM-induced disease worldwide.
Methods
Respiratory samples are being analyzed for acid-fast bacilli (AFB) culture and NTM identification at Dankook University Hospital in Cheonan, Korea, from September 2005 to September 2011. Identification is performed by using polymerase chain reaction-restriction fragment length polymorphism analysis targeting a novel region of the rpoB gene.
Results
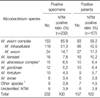
A total of 25,133 specimens were received for AFB culture, of which 1,014 (4.0%) were NTM-positive. A total of 267 samples from 186 patients were tested for NTM identifications, and 232 samples from 157 patients were positive for NTM species. Among the patients who tested positive for NTM, 65.6% were men and the average age was 63.3 years. Mycobacterium avium complex, the most commonly detected NTM pathogen, was found in 65.9% of the 232 samples. The annual average percentage of NTM isolates from AFB culture-positive specimens was 31.3%: the highest rate was seen in 2011 (44.3%), followed by 2009 (37.4%) and 2010 (37.2%). An upward trend in NTM incidence was found during the study period.
Mycobacteria species other than those of the Mycobacterium tuberculosis complex (MTBC) are called nontuberculous mycobacteria (NTM) or "atypical" mycobacteria. NTM are environmental organisms found in soil and water throughout the world1,2. NTM are generally hardy, ubiquitous environmental bacteria that vary in geographic distribution and pulmonary pathogenicity. NTM can also cause disseminated disease3. Disseminated disease due to NTM is primarily associated with acquired immunodeficiency syndrome and other forms of severe immunosuppression4. However, the incidence of NTM disease in patients without human immunodeficiency virus infection is increasing5.
Different NTM species have different antibiotic susceptibility patterns, and their resistance to anti-tuberculosis drugs is of particular importance. For these reasons, the accurate and early differential diagnosis of MTBC and NTM is required for optimal outcomes.
Currently, the identification of clinical isolates of mycobacteria at the species level is primarily based on the characteristics of the cultured bacteria and the biochemical test results. These conventional tests can take several weeks to perform and cannot always precisely identify the species6. Furthermore, these testing procedures are complex and laborious, and they are usually impeded by the slow growth of mycobacteria in culture. There are numerous species of NTM, and recently developed molecular methods have enabled the recognition of many of these species7. In this study, NTM were identified using a polymerase chain reaction (PCR)-restriction fragment length polymorphism (RFLP) method, based on the rpoB gene, at the Korean Institute of Tuberculosis8,9.
Mycobacterial identification at the species level is both of academic interest and of importance for gaining a better understanding of the organisms' epidemiology and pathogenesis. Geographic variability in the environmental exposure and prevalence of NTM disease is of global significance10.
Given these clinical challenges, further knowledge of the epidemiology of NTM in Korea is needed. The purpose of this study was to identify NTM and investigate their distribution in clinical specimens isolated from a tertiary teaching hospital in Cheonan, Korea.
This study included the isolation of NTM species from all clinical specimens referred to Dankook University Hospital Laboratory in Cheonan, Korea, from September 2005 to September 2011 (Table 1). Patients for whom NTM identification tests were requested provided samples of sputum and bronchial washing fluid. For this study, we retrospectively analyzed the results of these samples. Data were analyzed and categorized according to gender, age, and year of analysis.
For respiratory samples, N-acetyl-L-cysteine (NALC)-NaOH solution (5% NaOH+ 0.5% NALC) was added to the sample to liquefy and decontaminate the mucous sputum. The solution was centrifuged at 3,000 ×g for 18 minutes at 4℃, and the supernatant was discarded. Phosphate buffered saline 1 mL was added after the sediment had been vortexed.
The processed samples (0.2 mL) were used to inoculate 3% Ogawa medium (Eiken, Tokyo, Japan) and were cultured for 8 weeks in an incubator at 35-37℃ under 5-10% CO2. An interim report was provided at 4 weeks, if necessary.
Samples (0.5 mL each) were used to inoculate MGIT medium (Becton Dickinson, Sparks, MD, USA) after mixing with PANTA/supplement according to the manufacturer's protocol. The tubes were then incubated for 6 weeks in the BACTEC MGIT 960 system (Becton Dickinson). If fluorescence was detected in the tube, the test was considered positive.
A total of 25,133 specimens were received for AFB culture, of which 3,236 (12.9%) were AFB positive and 1,014 (4.0%) were NTM positive. A total of 267 samples from 186 patients were collected for NTM identification, and 232 samples from 157 patients were positive for NTM species (Table 1).
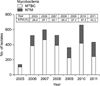
Gender analysis showed that 66.7% of all patients were men, and that 65.6% of the NTM-positive patients were men. The average patient age was 63.3 years (range, 33.3-91.1 years). More than 50% of patients were aged 60-79 years (Figure 1).
Mycobacterium avium complex (MAC), the most common NTM, was detected in 153 samples (65.9%): M. intracellulare was detected in 119 and M. avium in 34 samples. M. kansasii was the next most prevalent species (18 isolates, 7.8%), followed by M. abscessus complex (M. abscessus and M. massiliense; 15 isolates, 6.5%) and M. gordonae (12 isolates, 5.2%) (Table 2). The annual distributions of NTM species are detailed in Table 3.
The overall proportion of NTM isolates from among the respiratory AFB-positive specimens was 31.3% (1,014/3,236); the highest rate was seen in 2011 (192/433, 44.3%), followed by 2009 (135/361, 37.4%) and 2010 (246/662, 37.2%). There was an upward trend in NTM proportion in respiratory specimens during the study period (Cochran-Armitage test for trend, p<0.001) (Figure 2).
NTM are ubiquitous in the environment, and are found in water, soil, and air, as well as in animal-derived materials. Currently, more than 140 species of NTM are known11, and 50 species have been identified as opportunistic pathogens in humans12. NTM isolation and disease prevalence seems to be increasing worldwide13-15, and in Korea16-18. We assessed NTM species distribution and epidemiologic trends from isolates during 2005-2011 in the Cheonan area of Korea.
In the study by Lee et al.19, the gender ratio of patients with NTM disease was close to 1 (male:female ratio of 1.07:1). The study by Choi et al.20, on the other hand, found a male:female ratio of 2.56:1. Our results (male:female ratio of 1.91:1) lead us to conclude that NTM is not strongly associated with gender, but rather depends more on region and timing.
In our study, the average age was 63.3 years: 28.0% of patients were aged 60-69 years, and 23.6% were aged 70-79 years. The average patient age in other studies of NTM disease were as follows: 48.7 years in the study by Baek et al.21 performed in 1998-1999, 53 years in the study by Lee et al.19 performed in 1999, 58 years in the study by Choi et al.20 performed in 2002-2003, 58.7 years in the study by Lee et al.22 performed in 2002-2003, and 61 years in the study by Kim et al.23 performed in 2003. From these results, it appears that the average age of patients with NTM has been increasing since the late 1990s. Further research is warranted to investigate this phenomenon.
In this study, NTM species were more commonly isolated from men than from women; however, NTM was not strongly associated with gender, but rather depended more on region and timing. The average age of patients with NTM has been increasing since the late 1990s. The variation in rates reported by different hospitals may be due to variations in patient group characteristics, research periods, the specimen collection and detection methods used, and NTM detection thresholds.
The NTM species in the 232 samples in this study were as follows: M. intracellulare (119 samples, 51.3%), M. avium (34, 14.7%), and M. kansasii (18, 7.8%). In a study performed in Seoul17, MAC was found in 138 of the 328 samples (42.1%), while other identified species included M. fortuitum (64, 15.2%), M. abscessus (37, 11.3%), and M. gordonae (33, 10.1%). However, in a study conducted in the Masan20 area, MAC was found in 55 of 100 samples (55%), while other species included M. abscessus (25, 25%), M. fortuitum (9, 9%), and M. chelonae (8, 8%). In a study from Ulsan5, 22.7% of isolates from a total of 384 samples were identified as MAC, while 15.9% were M. kansasii, 11.5% were M. gordonae, and 8.9% were M. fortuitum. In a study conducted in Hong Kong24, 19% of detected species were M. gordonae, 15% were M. terrae, 12% were M. fortuitum, and 5% were M. chelonae. A Danish survey25 found that 55.3% of NTM isolates were M. gordonae, 19.3% were MAC, 4.8% were M. fortuitum, and 3.9% were M. abscessus. Finally, a US study26 reported rates of 80.1% for MAC, 12.1% for M. chelonae/abscessus, 5.6% for M. fortuitum, and 5.5% for M. kansasii. M. gordonae is often regarded as a contaminant7, although infections due to M. gordonae have been reported in some patients, such as those in an immunocompromised state27,28. Our results are quite different from those of studies performed in other countries, which further suggests that NTM disease depends on the characteristics of regional populations29.
In this study, NTM were found in 232 samples (7.17% positive rate in cultured specimens). The positive rate in Korea30,31 in the 1960s was <1%. In 1970, Kim et al.30 identified NTM species in sputum at a rate of 2.7%. More recently, NTM isolation rates in cultured specimens have been found to be approximately 10-30%, as represented by those from Seoul Asan Hospital32 (21.9%) in 2002, Seoul National University (SNU) Hospital9 (21.5%) in 2006, Fatima Hospital33 (7.9%) in 2009, and Gil Hospital34 (19.4%) in 2012. The variation in rates reported by different hospitals may be due to variations in patient group characteristics, research periods, specimen collection and detection methods used, and NTM detection thresholds.
Along with increases in the proportion of NTM isolates reported from referred specimens, the NTM ratio of respiratory AFB culture-positive specimens also increased between 2005 and 2011. Overall, an upward trend in NTM incidence was found during the study period.
Given these clinical challenges, further knowledge of the epidemiology of NTM in Korea is needed. Such knowledge will be beneficial in the treatment of NTM disease and the development of clinical science.
Figures and Tables
 | Figure 1Age group distribution of the positive specimens. Forty-four patients (28.0%) were aged 60-69 years, 37 patients (23.6%) were aged 70-79 years, and 34 patients (21.7%) were aged 50-59 years. M., Mycobacterium. |
 | Figure 2Annual changes in the proportions of nontuberculous mycobacteria (NTM) vs. Mycobacterium tuberculosis complex (MTBC) isolates in respiratory specimens. The trend showed increasing rates, from 25.6% in 2005 to 44.3% in 2011. |
Acknowledgements
The present research was supported by the research fund of Dankook University in 2004.
References
1. Katoch VM. Infections due to non-tuberculous mycobacteria (NTM). Indian J Med Res. 2004; 120:290–304.
2. Portaels F. Epidemiology of mycobacterial diseases. Clin Dermatol. 1995; 13:207–222.
3. Primm TP, Lucero CA, Falkinham JO 3rd. Health impacts of environmental mycobacteria. Clin Microbiol Rev. 2004; 17:98–106.
4. Olivier KN. Nontuberculous mycobacterial pulmonary disease. Curr Opin Pulm Med. 1998; 4:148–153.
5. Jeong J, Lee SH, Jeong US, Chang CL, Kim SR. Identification of mycobacteria using high performance liquid chromatography in clinical specimens. Korean J Clin Microbiol. 2004; 7:148–155.
6. Bang HI, Choi TY, Shin JW. Comparison of Ogawa media, BACTEC MGIT 960 system and TB/NTM real-time PCR for detecting Mycobacterium species. Tuberc Respir Dis. 2011; 71:249–253.
7. Koh WJ, Kwon OJ, Ham HS, Suh GY, Chung MP, Kim HJ, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens. Korean J Med. 2003; 65:10–21.
8. Lee H, Park HJ, Cho SN, Bai GH, Kim SJ. Species identification of mycobacteria by PCR-restriction fragment length polymorphism of the rpoB gene. J Clin Microbiol. 2000; 38:2966–2971.
9. Lee H, Bang HE, Bai GH, Cho SN. Novel polymorphic region of the rpoB gene containing Mycobacterium species-specific sequences and its use in identification of mycobacteria. J Clin Microbiol. 2003; 41:2213–2218.
10. Shin S, Kim EC, Yoon JH. Identification of nontuberculous mycobacteria by sequence analysis of the 16S ribosomal RNA, the heat-shock protein 65 and the RNA polymerase beta-subunit genes. Korean J Lab Med. 2006; 26:153–160.
11. Daley CL, Griffith DE. Nontuberculous mycobacterial infections. In : Mason RJ, Broaddus VC, Martin TR, King TE, Schraufnagel DE, Murray JE, editors. Murray and Nadel's textbook of respiratory medicine. 5th ed. Philadelphia: Saunders;2010. p. 793–810.
12. Brown-Elliott BA, Griffith DE, Wallace RJ Jr. Newly described or emerging human species of nontuberculous mycobacteria. Infect Dis Clin North Am. 2002; 16:187–220.
13. Marras TK, Chedore P, Ying AM, Jamieson F. Isolation prevalence of pulmonary non-tuberculous mycobacteria in Ontario, 1997-2003. Thorax. 2007; 62:661–666.
14. Lai CC, Tan CK, Chou CH, Hsu HL, Liao CH, Huang YT, et al. Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000-2008. Emerg Infect Dis. 2010; 16:294–296.
15. Thomson RM. NTM working group at Queensland TB Control Centre and Queensland Mycobacterial Reference Laboratory. Changing epidemiology of pulmonary nontuberculous mycobacteria infections. Emerg Infect Dis. 2010; 16:1576–1583.
16. Jeon K, Koh WJ, Kwon OJ, Suh GY, Chung MP, Kim H, et al. Recovery rate of NTM from AFB smear-positive sputum specimens at a medical centre in South Korea. Int J Tuberc Lung Dis. 2005; 9:1046–1051.
17. Lee JY, Choi HJ, Lee H, Joung EY, Huh JW, Oh YM, et al. Recovery rate and characteristics of nontuberculous mycobacterial isolates in a university hospital in Korea. Tuberc Respir Dis. 2005; 58:385–391.
18. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, et al. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010; 14:1069–1071.
19. Lee J, Kim Y, Park J, Ko W, Yang D, Kim S, et al. Clinical utility of bronchial washing PCR for IS6110 and amplicor for the rapid diagnosis of active pulmonary tuberculosis in smear negative patients. Tuberc Respir Dis. 2001; 50:213–221.
20. Choi SP, Lee BK, Min JH, Kim JH. Pathogenic classification and clinical characteristics of nontuberculous mycobacterial pulmonary disease in a national tuberculosis hospital. Tuberc Respir Dis. 2005; 59:606–612.
21. Baek SH, Lee JM, Kang MJ, Son JW, Lee SJ, Kim DG, et al. How reliable is sputum PCR test in the diagnosis of pulmonary tuberculosis when sputum smear is negative? Tuberc Respir Dis. 2001; 50:222–228.
22. Lee JS, Ji HS, Hong SB, Oh YM, Lim CM, Lee SD, et al. Clinical utility of polymerase chain reaction for the differentiation of nontuberculous mycobacteria in patients with acid-fast bacilli smear-positive specimens. Tuberc Respir Dis. 2005; 58:452–458.
23. Kim HK, Kim YR, Park JP, Kim NH, Ok CH, Jung MH, et al. Isolation of nontuberculous mycobacteria by DNA probe and clinical characteristics of patients with NTM pulmonary disease. Tuberc Respir Dis. 2005; 58:248–256.
24. Simons S, van Ingen J, Hsueh PR, Van Hung N, Dekhuijzen PN, Boeree MJ, et al. Nontuberculous mycobacteria in respiratory tract infections, eastern Asia. Emerg Infect Dis. 2011; 17:343–349.
25. Andrejak C, Thomsen VO, Johansen IS, Riis A, Benfield TL, Duhaut P, et al. Nontuberculous pulmonary mycobacteriosis in Denmark: incidence and prognostic factors. Am J Respir Crit Care Med. 2010; 181:514–521.
26. Prevots DR, Shaw PA, Strickland D, Jackson LA, Raebel MA, Blosky MA, et al. Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. Am J Respir Crit Care Med. 2010; 182:970–976.
27. Douglas JG, Calder MA, Choo-Kang YF, Leitch AG. Mycobacterium gordonae: a new pathogen? Thorax. 1986; 41:152–153.
28. Asija A, Prasad A, Eskridge E. Disseminated Mycobacterium gordonae infection in an immunocompetent host. Am J Ther. 2011; 18:e75–e77.
29. Yim JJ, Park YK, Lew WJ, Bai GH, Han SK, Shim YS. Mycobacterium kansasii pulmonary diseases in Korea. J Korean Med Sci. 2005; 20:957–960.
30. Kim KS, Shin YD, Ahn JW. Epidemiologic study of unclassified mycobacteria. Tuberc Respir Dis. 1966; 13:5–20.
31. Lee SK, Shin YD. Epidemiologic study of atypical mycobacterial infection. Tuberc Respir Dis. 1967; 14:12–38.
32. Lee HW, Kim MN, Shim TS, Bai GH, Pai CH. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients. Tuberc Respir Dis. 2002; 53:173–182.
33. Lee JK, Kwon HY, Kwon JK, Lee HJ, Lee DW, Lee YJ, et al. Recovery rate of nontuberculous mycobacteria and the clinical course of nontuberculous mycobacterial pulmonary disease at a secondary hospital. Tuberc Respir Dis. 2009; 67:199–204.
34. Lee MK, Seo YH, Jeong JH, Park PW, Kim KH, Ahn JY, et al. Nontuberculous mycobacteria isolated from respiratory specimens during recent two years: distribution and clinical significance. Korean J Clin Microbiol. 2012; 15:98–103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download