Abstract
A patient who has multiple lung masses with a history of malignancy in organs other than the lung is more likely to be diagnosed with metastatic rather than primary lung cancer. Rarely, metastatic cancer can coexist with primary. We experienced a case of concurrent diagnosis of primary small cell lung cancer and pulmonary metastasis of uterine malignant mixed Müllerian tumor (MMMT). The patient was a 52-year-old female with femur fracture and multiple lung masses with a history of an operation for uterine MMMT. The small cell lung cancer was diagnosed by bronchoscopic biopsy. The central lung mass decreased after chemotherapy for small cell lung cancer but multiple peripheral masses increased. A percutaneous biopsy for one of peripheral masses revealed metastatic uterine MMMT. We suggest that we have to consider the possible presence of concomitant malignancies of different origins in one organ especially with patients who had a history of malignancy in another organ.
When we encounter a patient who has multiple lung masses with a history of malignancy in organs other than the lung, it is reasonable to suspect pulmonary metastasis first rather than primary lung cancer. However, if the patient is diagnosed with primary lung cancer, then we would have to change subsequent diagnostic and treatment plans. Although, it is rare, we can suspect the concurrent presence of primary and the metastatic malignancies if the standard chemotherapy for the primary lung cancer yields to the responses inconsistently. Here we report a patient with a history of a surgery for malignant mixed Müllerian tumor (MMMT) one and a half years ago, who exhibited femur fracture and multiple lung masses. The biopsies for the two different lung masses revealed small cell lung cancer and MMMT for each mass.
A 52-year-old woman visited the department of orthopedic surgery due to the pain in her left hip for 3 months. She was a housewife who had never smoked, and she had been taking a medicine for hypertension. She had no recent trauma. A fracture of left femoral head and the enlarged right inguinal and the left iliac lymph nodes were found on the hip magnetic resonance imaging. She was referred to pulmonology department because her chest X-ray showed multiple bilateral lung masses (Figure 1). The only respiratory symptom was mild dry cough. We found a lung mass that surrounds the left lower lobar bronchus, multiple peripheral lung masses, and the lymph node enlargements of the mediastinal areas from the chest computed tomography (Figure 2). On both sides of her lower neck, multiple lymph nodes were palpable. The routine laboratory findings were not remarkable.
She had a history of total hysterectomy for uterine MMMT (Figure 3) one and a half years ago. Multiple pelvic lymph node enlargements were found 6 months later and a recurrence of MMMT was confirmed by surgical biopsy. At that time, there was no small cell carcinoma component in uterine cancer pathologically. No further treatment for MMMT was given to her. Based on her past history, we initially suspected lung and femur metastases of MMMT. The protruding mass lesion on the orifice of the left lower lobe basal segment was found and biopsied by the bronchoscopy. However, the pathologic features of this mass was the typical small cell lung carcinoma (Figure 4) rather than metastatic MMMT from uterus. We assumed that all of these findings are attributable to small cell lung cancer, and we started the treatment accordingly. She was treated with etoposide plus cisplatin. Radiation was delivered to her femur for palliation of pain. After 2 cycles of chemotherapy, most lesions that were located relatively central (mediastinal lymph nodes and the mass around the left lower lobar bronchus) slightly decreased, but the most of peripheral masses increased (Figure 5). In the meantime, she had to undergo hemiarthroplasty of the left hip due to persistent pain. The pathologic finding of femur head was consistent with metastatic adenocarcinoma (Figure 6). It was possible that the metastases of carcinomatous component of MMMT probably appeared in the femur. After these observations, we had the percutaneous needle biopsy for the peripheral lung mass on the left lower lobe which showed rapid growing even after chemotherapy because we suspected the possible presences of both primary and metastatic lung cancers. The pathology revealed the metastasis of sarcomatous component of MMMT (Figure 7). This finding was coincident with the pathology of uterine cancer.
As the metastases to lung from MMMT progressed
rapidly, her performance status was getting worse. She
suffered from anorexia, asthenia, and dyspnea. Eventually,
massive left pleural effusion developed. Cancer
antigen 125 (CA-125) level of pleural effusion was 149.9
U/mL (~35 U/mL). Tumor thrombi occluded the inferior
vena cava and the external iliac vein. Salvage chemotherapy
for MMMT with ifosfamide and cisplatin was
done, but it was not efficacious. Unfortunately, she deceased
because of acute renal and respiratory failure.
Initially, it is natural to suspect pulmonary metastasis when multiple and bilateral lung masses are found. It is more likely to appear in patients with a recent history of malignancy in other organs like our patient. Contrary to our expectation, we got the diagnosis of small cell lung cancer in a relatively young non-smoking woman without a specific history of an exposure to carcinogens1. The second biopsy of another mass revealed metastatic lung cancer which was MMMT. The elevation of CA-125 from pleural effusion also supported the pleural metastasis of MMMT2. So the patient was found to have primary lung cancer and pulmonary metastasis of MMMT concomitantly. The situation like our patient might be extremely rare or the chance of diagnosis was missed because it is not a common practice to obtain multiple biopsies in a single organ.
MMMTs are rare gynecological cancer that normally affects post menopausal women. They can arise in the uterus, ovaries, fallopian tubes, vagina, and peritoneum, or rarely at extragenital sites. It comprises 1.5~5.0% of all malignant tumors of uterus3. They have both sarcomatous and carcinomatous components. Long-term survival can be expected by performing curative primary surgery4. However, this happens rarely because of the high rate of distant recurrence. The recurrence rate was 56% in patients with MMMT who were previously treated with curative intent5. The rate of distant metastasis was higher than the locoregional recurrences with 49% to 18%5. Approximately 85% of the distant metastases were diagnosed within 3 years of curative treatment. The most common site of distant metastasis is lung and abdomen follows it5. The usual pattern of pulmonary metastasis is multiple pulmonary nodules6 as it is shown in our case. However, a case of solitary lung metastasis causing superior vena cava syndrome was reported 7. Although bone metastasis of MMMT is not common, our patient had a single bone metastasis. It is also worth mentioning that carcinomatous and sarcomatous component of MMMT metastasized separately to lung and bone in our patient.
In conclusion, we report a patient who was diagnosed with small cell lung cancer and metastasis of MMMT concurrently. Although, the multiple bilateral lung masses and a history of malignancy in other organs were present, we must consider the possibility of primary lung cancer and the concomitant presence of different malignancy.
Figures and Tables
Figure 1
Initial chest X-ray. The chest radiography reveals two multilobulated masses (arrows) in retrocardiac area of the left lung and multiple round metastatic nodules in mid lung fields of both lung.

Figure 2
Initial chest computed tomography. (A) The axial image at the level of basal trunk of the left lower lobe bronchus reveals central lung cancer in the left lower lobe and massive subcarinal lymph node enlargement. (B) The axial image at the level of the lung base reveals a round metastatic mass in posterior basal segment of the left lower lobe.

Figure 3
Histopathologic finding of uterus. Malignant mixed Müllerian tumor, also known as carcinosarcoma, is composed of malignant epithelial and stromal components. This figure reveals glandular epithelial (A) and sarcomatous (B) elements of uterus lesion (A, B, H&E stain, ×400).
Figure 4
The histopathologic finding of bronchoscopic biopsy tissue. This slide shows round to oval tumor cells which have minimal cytoplasm and are about twice as large as neutrophil. Their nucleus are 'salt and pepper' chromatin pattern and don't have a prominent nucleoli. We can also find frequent mitoses. These pathologic findings are consistent with small cell carcinoma (H&E stain, ×400).
Figure 5
The computed tomography after two cycles of chemotherapy. (A) The mediastinal mass decreased (arrow). (B) The pleural based mass on left lower lobe increased markedly (arrow). Compare with pictures in Figure 2.
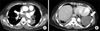
Figure 6
The histopathologic finding of femur bone. The bone lesion is composed of metastatic adenocarcinoma, which is similar to the carcinoma component of the uterus cancer. This is quite different from the lung lesion (H&E stain, decalcification, ×400).
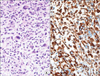
Figure 7
The histopathologic finding of percutaneous biopsy of peripheral lung mass. This slide reveals sarcoma which is composed of atypical spindle cells with frequent atypical mitoses. The pathologic features of uterine sarcoma elements resemble this (A). Vimentin immunohistochemistry was positve in this lung lesion (B) (A, H&E stain, ×400; B, vimentin immunohistochemistry, ×400).
References
1. Yonemori K, Kunitoh H, Sekine I. Small-cell lung cancer with lymphadenopathy in an 18-year-old female nonsmoker. Nat Clin Pract Oncol. 2006. 3:399–403.
2. Peters WA 3rd, Bagley CM, Smith MR. CA-125: use as a tumor marker with mixed mesodermal tumors of the female genital tract. Cancer. 1986. 58:2625–2627.
3. Barwick KW, LiVolsi VA. Malignant mixed mullerian tumors of the uterus: a clinicopathologic assessment of 34 cases. Am J Surg Pathol. 1979. 3:125–135.
4. Gourley C, Al-Nafussi A, Abdulkader M, Smyth JF, Gabra H. Malignant mixed mesodermal tumours: biology and clinical aspects. Eur J Cancer. 2002. 38:1437–1446.
5. Spanos WJ Jr, Peters LJ, Oswald MJ. Patterns of recurrence in malignant mixed müllerian tumor of the uterus. Cancer. 1986. 57:155–159.
6. Bouros D, Papadakis K, Siafakas N, Fuller AF Jr. Patterns of pulmonary metastasis from uterine cancer. Oncology. 1996. 53:360–363.
7. Ozkan M, Er O, Kaplan B, Altinbas M, Ozcelik B, Tokat F, et al. Presentation with superior vena cava syndrome secondary to solitary lung metastasis mimicking primary lung cancer following resection of a uterine malignant mixed mullerian tumor: brief case report. Eur J Obstet Gynecol Reprod Biol. 2005. 118:260–264.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download