Abstract
Typhlitis is a necrotizing colitis that usually occurs in neutropenic patients and develops most often in patients with hematologic malignancies such as leukemia and lymphoma. Typhlitis may proceed to bowel perforation, peritonitis and sepsis, which requires immediate treatment. Irinotecan is a semisynthetic analogue of the natural alkaloid camptothecin which prevents DNA from unwinding by inhibition of topoisomerase I. It is mainly used in colon cancer and small cell lung carcinoma (SCLC), of which the most common adverse effects are gastrointestinal toxicities. To the best of our knowledge, no case of typhlitis after chemotherapy with a standard dose of irinotecan in a solid tumor has been reported in the literature. We, herein, report the first case of typhlitis developed after chemotherapy combining irinotecan and cisplatin in a patient with SCLC.
Irinotecan (camptothecin-11) is a semisynthetic analogue of the natural alkaloid camptothecin, which can be used as the first-line chemotherapy of colorectal cancer and small cell lung carcinoma (SCLC). In a randomized, phase III study involving 154 patients with extensive small cell lung carcinoma, irinotecan-plus-cisplatin therapy was compared with etoposide-plus-cisplatin therapy resulting in more effective outcome with higher overall response rate (84.4% vs. 67.5%) and median survival (12.8 months vs. 9.4 months)1. Gastrointestinal toxicities are common side effects in the patients treated with irrinotecan, such as abdominal pain, nausea, and vomiting. Especially, diarrhea is the most common and serious complication, reporting incidence rate of more than 80%2. Typhlitis, neutropenic enterocolitis, is most commonly reported in leukemias while it is rare in solid tumors. We report a case of typhlitis in a patient with SCLC after treatment with standard dose of irinotecan and cisplatin with a review of the literature.
A 73-year-old man was admitted to our hospital with a complaint of diffuse abdominal pain that had lasted for 2 days. He was diagnosed as extensive stage SCLC of the left lung with multiple metastases of brain, right adrenal gland, pancreas and lumbar spine, 2 months ago, and had received radiation therapy for the metastatic brain tumor. He had been taking hydrochlorothiazide for 5 years under the diagnosis of hypertension, and had a history of 35 pack-year smoking.
Ten days before admission, chemotherapy consisting of irinotecan 100 mg (60 mg/m2 days 1 and 8) and cisplatin 100 mg (60 mg/m2 day 1) was started. On admission day, vital signs were blood pressure 130/70 mm Hg, heart rate 76/min, respiration rate 20/min, and body temperature 36.6℃. Bowel sound was hyperactive, and there was mild tenderness on the right lower quadrant without rebound tenderness or palpable mass. Laboratory data showed white blood cell (WBC) count of 4,000/mm3 with absolute neutrophil 3,600/mm3, hemoglobin 10.6 g/dL, platelet 210,000/mm3, high sensitivity C-reactive protein was 8.10 mg/dL. His liver and renal function panel were unremarkable. Chest X-ray films showed left hilar mass without interval change compared with the one taken at the time of cancer diagnosis (Figure 1). On the abdominal X-ray films, there was a nonspecific gaseous distension (Figure 2). He was treated with antispasmodics, symptomatically.
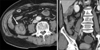
On the day 3 of hospitalization (day 13 of chemotherapy), despite supportive care, he complained of aggravated abdominal pain and developed fever of 37.6℃. Laboratory data revealed a hematological toxicity, hemoglobin decreased to 9.2 mg/dL, WBC count to 1,400/mm3, absolute neutrophil count to 1,064/mm3, and platelets to 161,000/mm3. An enhanced abdomen computed tomography (CT) scan revealed bowel wall thickening in the cecum and terminal ileum, and surrounding mesenteric inflammation, consistent with typhlitis (Figure 3). He was treated with empirical antibiotics and supportive therapy of bowel rest, intravenous fluids, and nutritional support.
During the next 4 days, his abdominal pain improved slowly. On the day 7 of hospitalization, oral intake was available and absolute neutrophil count increased to 1,704/mm3. Follow-up ultrasonography performed on the day 16 of hospitalization showed resolution of bowel wall thickening, and he was discharged on hospital day 29. After discharge, he refused additional chemotherapy and expired 3 months later due to progression of SCLC.
Typhlitis, a necrotizing enterocolitis, is usually reported in neutropenic patients during chemotherapy, which mainly involves cecum, ileum, and the ascending colon. Typhlitis can be a life-threatening complication in the neutropenic patients, that may progress to intestinal necrosis, hemorrhage, perforation, peritonitis, and eventually sepsis3. Mechanism of chemotherapy related typhlitis is as follows. Anticancer agents cause direct mucosal cytotoxicity of the gastrointestinal tract and neutropenia leading to enteral microorganism proliferation. Bacterial endotoxins result in intestinal mucosal ischemia, necrosis, and a breakdown of intestinal mcosal barrier4. Cecum is the most common site of typhlitis, because of its poor blood supply, lymphatic drainage and direct exposure to colonic bacteria, making it more liable to infection4,5.
The typical clinical manifestations of typhlitis include abdominal pain and fever in a patient during chemotherapy, as in this case. Early diagnosis is the most important in the treatment of typhlitis. Abdominal CT, ultrasonography, and barium enema can be used as diagnostic tools. CT scan is a valuable tool for early diagnosis. Findings include an edematous colon, symmetric mucosal thickening more than 5 mm, and inflammation of the pericolonic tissues3,5,6, as shown in Figure 3. Ultrasonography is also a good diagnostic tool, which may reveal a target sign encircling mural thickening as a result of mucosal edema in the ileum and cecum6. For this reason, we performed abdominal ultrasonography to follow him up.
Typhlitis usually occurs in leukemia patients receiving chemotherapy. Recently, as high-dose chemotherapy became popular, the incidence of typhlitis is increasing in patients with solid tumors7. In particular, several cases of typhlitis have been reported in lung cancer and pemetrexed, paclitaxel, docetaxel, 5-fluorouracil and vinorelbine were suggested as causative agents8.
Irinotecan is a derivatives of the natural cytototoxic compound camptothecin which produces anticancer effects through inhibition of DNA topoisomerase I9. The most common complication of irinotecan is gastrointestinal mucosal toxicities, in particular, more than 80% of patients receiving irinotecan therapy experience diarrhea2.
Although five cases of typhlitis have been reported in phase I study determining the maximum tolerated dose of camtothecin analogues (topotecan and irinotecan)9, no case has been reported in patients treated with standard dose. It is unknown how typhlitis occurs after chemotherapy with irinotecan. The following characteristics of irinotecan may be helpful in the comprehension of the irinotecan induced typhlitis. Irinotecan has a stronger gastrointestinal mucosal cytotoxicity than any other anticancer drug. In addition, it is well known that patients with UGT1A1 genetic mutation tend to develop severe side effects10. In this case, due to the lack of his genetic study at that time, we were not able to completely exclude the possibility of the genetic mutation. We presume that he might have had a UGT1A1 polymorphism, because irinotecan induced typhlitis was developed under not severe neutropenia.
It is still controversial whether medical or surgical treatment is more proper. In the past, surgical treatment was preferred3,5. However, because of poor prognosis due to underlying diseases, and high mortality due to severe postoperative complications, priority is shifting to conservative treatment including broad spectrum antibiotics, bowel rest, intravenous fluids, and parenteral nutritional support5. On the other hand, surgical treatment takes priority in patients with gastrointestinal hemorrhage, bowel perforation, and sepsis4,11. In this case, this patient was successfully treated with conservative therapy without need of surgical intervention.
In conclusion, although patient is treated with standard dose, the clinicians should be aware of the possibility of chemotherapy related typhlitis during the therapy with irinotecan in order to optimize the effect of treatment and prevent toxic mortality.
Figures and Tables
References
1. Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura T, Yokoyama A, et al. Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer. N Engl J Med. 2002. 346:85–91.
2. Bleiberg H, Cvitkovic E. Characterisation and clinical management of CPT-11 (irinotecan)-induced adverse events: the European perspective. Eur J Cancer. 1996. 32A:Suppl 3. S18–S23.
3. Gorschlüter M, Mey U, Strehl J, Ziske C, Schepke M, Schmidt-Wolf IG, et al. Neutropenic enterocolitis in adults systematic analysis of evidence quality. Eur J Haematol. 2005. 75:1–13.
4. Keidan RD, Fanning J, Gatenby RA, Weese JL. Recurrent typhlitis: a disease resulting from aggressive chemotherapy. Dis Colon Rectum. 1989. 32:206–209.
5. Oh YS, Yoo JH, Kim YR, Hahn CW, Park CW, Shin WS, et al. Four cases of typhlitis in patients with acute leukemia. Korean J Med. 1995. 49:550–555.
6. Cartoni C, Dragoni F, Micozzi A, Pescarmona E, Mecarocci S, Chirletti P, et al. Neutropenic enterocolitis in patients with acute leukemia: prognostic significance of bowel wall thickening detected by ultrasonography. J Clin Oncol. 2001. 19:756–761.
7. Kim YB, Lee SJ, Lee YH, Lee YK, Sin SK, Kim JS, et al. A case of typhlitis developed after anticancer chemotherapy in a patient with solid tumor. Korean J Med. 2002. 62:657–660.
8. Tiseo M, Gelsomino F, Bartolotti M, Barili MP, Ardizzoni A. Typhlitis during second-line chemotherapy with pemetrexed in non-small cell lung cancer (NSCLC): A case report. Lung Cancer. 2009. 65:251–253.
9. Rodriguez-Galindo C, Crews KR, Stewart CF, Furman W, Panetta JC, Daw NC, et al. Phase I study of the combination of topotecan and irinotecan in children with refractory solid tumors. Cancer Chemother Pharmacol. 2006. 57:15–24.
10. Hahn KK, Wolff JJ, Kolesar JM. Pharmacogenetics and irinotecan therapy. Am J Health Syst Pharm. 2006. 63:2211–2217.
11. Shamberger RC, Weinstein HJ, Delorey MJ, Levey RH. The medical and surgical management of typhlitis in children with acute nonlymphocytic (myelogenous) leukemia. Cancer. 1986. 57:603–609.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download