Abstract
A Septic embolism is a type of embolism infected with bacteria containing pus. These may become dangerous if dislodged from their original location. Embolisms of this type in the azygos vein are potentially fatal. The diagnosis of septic azygos vein embolism is difficult, so rapid diagnosis and treatment is important to avoid complications. Generally, treatment is enough for appropriate antibiotic therapy without anticoagulant therapy. We report a case of staphylococcal septic embolism in the azygos vein, which was discovered in a 51-year-old man exhibiting chest pain, dyspnea and fever. The patient was treated with antibiotic therapy alone without the use of anticoagulants.
Septic embolism is a rare disorder that is associated with bone infections, infective endocarditis, sinusitis, orbital cellulitis, femoral thrombophlebitis, urinary tract infections, central venous catheter infections, prosthetic cardiac valve infections and pacemaker infections. The most common causative organism is Staphylococcus aureus. Predisposing factors include diabetes mellitus, immunosuppression and intravenous drug use. Septic embolism can be difficult to diagnose and can present with a variety of features.
We report a case of staphylococcal septic embolism in the azygos vein, which was discovered in a 51-year-old man with chest pain, dyspnea and fever. The patient was treated with antibiotic therapy alone without anticoagulant therapy.
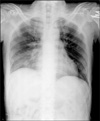
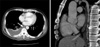
A 51-year-old male was admitted to our hospital with high grade fever, severe right-sided chest pain and dyspnea for five days. He had a history of poorly controlled type 2 diabetes mellitus. The patient appeared severely ill. On admission, his body temperature was 38.2℃, pulse rate was 93 per minute, respiration rate was 18 per minute and blood pressure was 120/90 mm Hg. Auscultation of the chest revealed decreased breath sound and inspiratory crackle at the right lower lung field. There was tenderness on palpation and percussion of his right lower chest wall. Initial laboratory evaluation showed white blood cell count of 22,300/µL with 88% segmented neutrophils, hemoglobin of 11.9 g/dL, platelets of 317,000/µL and C-reactive protein of 37.8 mg/dL. His plasma glucose was 438 mg/dL and hemoglobin A1C was 11%. He was negative human immunodeficiency virus. Chest X-ray showed right lower zone consolidation with pleural effusion and peripherally multiple nodular opacities (Figure 1). Further imaging with contrast enhanced helical computed tomography of the chest showed embolic occlusion of the azygos vein (Figure 2). Long vascular computed tomography did not show lower extremity deep vein thrombosis but showed intramuscular abscess on both lower legs (Figure 3). Initial empiric antibiotic therapy was started on ceftriaxone 2.0 g intravenously every twelve hours. The patient underwent a diagnostic thoracentesis with removal of serosanguinous fluid that was an exudative pleural effusion, negative bacterial and acid-fast stains and cytology. The pleural fluid cell count demonstrated a red blood cell count of 140/µL (per cubic millimeter), a white blood cell of 1,520/µL with 95% neutrophil and adenosine deaminase was normal. The patient's blood, sputum and pleural fluid cultures yielded oxacillin-sensitive S. aureus. Ceftriaxone was discontinued on day 3 of the admission. Nafcillin at 500 mg intravenously every four hours and isepamicin at 200 mg intravenously every twelve hours was begun. Transthoracic echocardiography revealed normal left ventricular function with no vegetation, valvular regurgitation and other signs of endocarditis.
With appropriate antibiotic therapy, the patient's clinical condition had been improved and subsequent chest X-ray showed gradual resolution of pneumonia and parapneumonic effusion. His diabetes was controlled well starting insulin therapy. After taking one month of antibiotics, a repeat chest computed tomography revealed complete resolution of septic embolism in the azygos vein without anticoagulant therapy (Figure 4).
Septic embolism is a type of embolism infected with bacteria, resulting in pus formation. The embolic blood clot that leads to an infarction in the pulmonary vasculature also contains microorganisms that incite a focal abscess. The bacterial insult to endothelium in vessel is postulated in regard to the pathogenesis of septic embolism. These may become dangerous if dislodged from their original location. Septic embolism in the azygos vein is potentially fatal because it may result in pulmonary embolism and sudden death. The most common causative organism is S. aureus. Predisposing factors include diabetes mellitus, immunosuppression and intravenous drug use1.
In this case, the patient presented sepsis with pneumonia and had signs of septic embolism with chest imaging such as poorly defined nodules in the lung periphery. Contrast enhanced helical computed tomography of the chest showed embolic occlusion of the azygos vein and long vascular computed tomography did not show lower extremity deep vein thrombosis (His Wells score for pulmonary embolism was 0 point, suggestive of low probability). In conclusion, the patient was diagnosed with septic azygos vein embolism caused by S. aureus bacteremia, parapneumonic effusion and lower leg intramuscular abscess. The patient was treated with antibiotics (nafcillin and isepamicin) without anticoagulant therapy and discharged after one month.
The diagnosis of septic embolism can be suspected from antecedents and symptoms, but imaging tests (especially, CT of the chest, and echocardiography) together with isolating cultures of microorganism play a key role in the diagnosis of septic embolism2. With early diagnosis, appropriate antimicrobial therapy and control of the infectious source, resolution of the illness can be expected for most patients with avoidance of potential complications. Other reports described that S. aureus was the predominant infective agent3,4. Therefore, initial empiric antibiotic therapy should include beta-lactamase-resistant penicillin by the intravenous route. There are no data available on whether an aminoglycoside should be added.
It may be difficult to the adequate management of septic patients with major deep venous thrombosis because septic embolism is the high risk for complications such as worsening sepsis, metastatic infection and pulmonary embolism by itself. However early administration of intravenous heparin followed by oral anticoagulant therapy in patients with septic embolism remains controversial. The presumed dangers include provocation of septic embolism from the infected thrombus itself or from concomitant infective endocarditis and complications of hemorrhage from unrecognized mycotic arterial aneurysms. Indeed, patient with septic embolism belong to a population at particularly high risk for development of infective endocarditis, and some authors have stated that anticoagulant therapy should be instituted only after infective endocarditis has been ruled out.
Patients with complications from septic vein embolism who fail to respond to antibiotic therapy alone may require anticoagulant therapy or inferior vana cava filter use. Greenfield and Proctor5 reviewed 175 septic patients who received inferior vena cava filters and found no reports of patients with recurrent sepsis episodes or any significant adverse events. On the other hand, an inferior vena cava filter has been shown to become infected during active sepsis6.
The diagnosis of septic azygos vein embolism is difficult, so rapid diagnosis and treatment is important to avoid complications. Radiologic imaging, especially CT of the chest, is valuable in the evaluation of patients with suspected azygos vein embolism7. Generally, appropriate antibiotic therapy without anticoagulant therapy may be a sufficient treatment of septic azygos vein embolism depending on the clinical situation.
Figures and Tables
Figure 1
Chest X-ray showed right lower zone consolidation with pleural effusion and peripherally multiple nodular opacities.
References
1. Ptaszynski AE, Hooten WM, Huntoon MA. The incidence of spontaneous epidural abscess in Olmsted County from 1990 through 2000: a rare cause of spinal pain. Pain Med. 2007. 8:338–343.
2. Cook RJ, Ashton RW, Aughenbaugh GL, Ryu JH. Septic pulmonary embolism: presenting features and clinical course of 14 patients. Chest. 2005. 128:162–166.
3. Ang AK, Brown OW. Septic deep vein thrombosis. J Vasc Surg. 1986. 4:563–566.
4. Andes DR, Urban AW, Acher CW, Maki DG. Septic thrombosis of the basilic, axillary, and subclavian veins caused by a peripherally inserted central venous catheter. Am J Med. 1998. 105:446–450.
5. Greenfield LJ, Proctor MC. Vena caval filter use in patients with sepsis: results in 175 patients. Arch Surg. 2003. 138:1245–1248.
6. Meda MS, Lopez AJ, Guyot A. Candida inferior vena cava filter infection and septic thrombophlebitis. Br J Radiol. 2007. 80:e48–e49.
7. Huang RM, Naidich DP, Lubat E, Schinella R, Garay SM, McCauley DI. Septic pulmonary emboli: CT-radiographic correlation. AJR Am J Roentgenol. 1989. 153:41–45.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download