Abstract
Background
Periostin is preferentially expressed in periosteum, indicating a potential role in bone formation. Recently, there have been emerging controversies about its role in invasion and metastasis of human malignancies. We attempted to determine the clinicopathological significance of periostin expression in non-small cell lung carcinoma (NSCLC).
Methods
Immunohistochemical staining of periostin protein from 91 cases of NSCLCs was performed using tissue microarray blocks. The results were correlated with clinicopathological parameters.
Results
Positive reaction to periostin was predominantly noted in the tumor stroma. The strongest reaction presented as a band-like pattern just around the tumor nests. Non-neoplastic lung tissue and most in-situ carcinomas did not show a positive reaction in their stroma. With respect to tumor differentiation, moderate to poor differentiated tumors (47/77) revealed even higher periostin expression than the well-differentiated ones (4/14) (p=0.024). High periostin expression was positively correlated with E-cadherin and p53 expression, but was not related with patient age, sex, tumor type, PCNA index, b-catenin, cyclin D1, pTNM-T, pTNM-N, stage, and patient survival (p>0.05).
Periostin, homologous with an insect cell adhesion molecule fasciclin I, is a recently identified gene that is preferentially expressed in periosteum, indicating a potential role in bone formation and maintenance of bone structure1. It has also been shown to be involved in the development of heart valves and other tissues2-4, and to interact with other extracellular matrix proteins such as fibronectin, tenascin-C, collagen V, and periostin itself5,6. Functionally, periostin interacts with integrins to support cell adhesion and the spreading of chondrocytes, fibroblasts, and cancer cells6. In addition, recent studies have reported that periostin is frequently found to be highly expressed in various types of human cancer cell lines in vitro and human cancer tissues in vivo7-10. In tumorigenesis, however, there have been controversies about its role for invasion and metastasis of human malignancies. Kudo et al.11 introduced that periostin was highly expressed in head and neck squamous cell carcinomas (HNSCC) in comparison with normal tissues, and the level of periostin expression was well correlated with the invasiveness of HNSCC cases. On the other hand, Kim et al.12 reported that the expression of periostin mRNA is significantly repressed in human bladder cancer tissues, and that periostin plays a role as a suppressive factor for invasion and metastasis. Collectively, the role of periostin in carcinogenesis is much variable so far. In human lung cancer, Sasaki et al.13 demonstrated the non-small cell lung carcinoma (NSCLC) patients with high periostin expression had significantly poorer survival than the patients without periostin expression by reverse transcriptase (RT)-PCR analysis. So, they suggested that periostin could be used as prognostic marker of NSCLC.
In this study, we analyzed the expression of periostin protein in both tumor and intratumoral stroma in a cohort group of NSCLC (n=91) by immunohistochemistry and correlated the findings with clinicopathologic parameters such as demography (age, gender), TNM stage, and histologic factors (type, differentiation, β-catenin, E-cadherin, p53 and PCNA index).
All patients with NSCLC who underwent lobectomy or pneumonectomy at Pusan National University Hospital, Busan, Korea, between June 2000 to October 2008 were considered for inclusion in this study. After exclusion of cases in which there was insufficient pathological material remaining for further study, a total of 91 cases were selected for this study (80 men and 11 women). The mean patient age was 65.2 years (range, 40.0~85.0 years; median, 67.0 years). Tumors were staged according to the TNM classification of the International Union Against Cancer (UICC) staging system14 after reviewing of the clinical, radiological, and pathological data. Other clinical information was extracted from medical records.
The surgically resected specimens were immediately fixed in 10% buffered formalin (pH 7.0). All sections containing both tumor tissue and surrounding lung tissue were embedded in paraffin. Pathologic diagnosis was based on the third edition of the World Health Organization classification15. There were 46 cases of squamous cell carcinoma (SqCC) and 45 cases of adenocarcinoma (AdC).
The representative tumor areas to be sampled for tissue microarray (TMA) were carefully selected and marked on the H&E slides. TMAs were assembled using a tissue-arraying instrument consisting of thin-walled stainless biopsy needles and stylets used to empty and transfer the needle contents. The assembly was held in an X-Y position guide that was manually adjusted by micrometers. Briefly, the instrument was used to create holes in a recipient paraffin block and to acquire tissue cores from the donor block using a thin-walled needle. The cylindrical sample was retrieved from the selected region in the donor block and extruded directly into the recipient block with defined array coordinates. A solid stylet, closely fitted in the needle, was used to transfer the tissue cores into the recipient block. Taking tumor heterogeneity into account, we used a large-diameter stylet (2.0 mm). The study specimens were routinely oversampled with two replicate core tumor region samples (different areas) from each donor block. Forty-eight cores from 24 tumors were included in each tissue array block. Multiple 4-µm sections were cut with a microtome.
Sections from TMA blocks were transferred to poly-L-lysine-coated glass slides and air-dried overnight at 37℃. They were then dewaxed in xylene (three changes), rehydrated in a graded series of decreasing ethanol concentrations, and rinsed in pH 7.4 Tris-buffered saline (TBS). Endogenous peroxidase activity was inactivated with 5% hydrogen peroxide in methanol for 15 min at 37℃.
Antigen retrieval, except for anti-proliferating cell nuclear antigen (PCNA), was performed using 5-minute microwave treatment (×2) in TBS. The following primary antibodies were used: periostin, β-catenin, E-cadherin, p53 and PCNA. Each antibody was incubated with tissue sections at room temperature. Immunohistochemical procedures were performed using two-step Envision Plus kit (Zymed Co.) with chromogen DAB. Detailed information concerning the antibodies used is summarized in Table 1.
For periostin stain, when the positive reaction to the antibody was found in less than 25% of tumor area stroma, it was scored semiquantitatively 'low expression'. With more than 25%, it was considered 'high'. For PCNA, the labeling index was determined by the percentage of positive nuclear staining after counting approximately 1,000 tumor cells from tumor areas at high power field (×400). In case of other antibodies (p53, β-catenin, E-cadherin), if less than 5% of tumor cells were positive, it was considered 'negative'. When 5 to 25% of tumor cells are positive for antibodies, it was '1+'. When more than 25% of tumor cells are positive, it was considered '2+'.
Pearson χ2 and Student's t tests were performed in the statistical analyses. For univariate survival analysis, the Kaplan-Meier method was applied. Clinicopathologic variables were further analyzed by multivariate Cox proportional hazards regression models to test for independent prognostic value. All analyses were carried out using the SPSS 15.0 software package (SPSS Inc., Chicago, IL, USA). p-values less than 0.05 were regarded as statistically significant.
The stromas from non-neoplastic lung and most of in situ carcinomas, including bronchioloalveolar carcinoma, were immunonegative to extracellular matrix protein periostin (Figure 1A, 1C). Positive periostin immunoreaction was frequently accentuated toward intratumoral stroma around invasive carcinoma cells. The strongest reaction in the positive stroma was present as band-like pattern just around tumor nests (Figure 1B, 1E). Occasionally, tumor cells themselves showed cytoplasmic expression of periostin in 4 of 46 SqCC cases (8.7%) and in 2 of 45 AdC (4.4%) (Figure 1D). The distribution of tumor cells with cytoplasmic expression was chiefly in the periphery of tumor nests in SqCC, whereas the cells with cytoplasmic expressin were randomly scattered in AdC. None of the tumors with intracellular periostin expression morphologically exhibited spindle-cell or mesenchymal morphologic change.
Correlation between histologic types of NSCLC and periostin expression was not shown. Regarding tumor differentiation, moderately to poorly differentiated tumors (47/77) revealed even higher periostin expression than well-differentiated ones (4/14) (p=0.024, Table 2). Otherwise, high periostin expression was positively correlated with E-cadherin and p53 expression (Table 3). However, it was not related with PCNA index, β-catenin, and cyclin D1 (respectively, p>0.05). Among other clinicopathologic parameters, patient age, sex, TNM-pT, TNM-pN and stage were not correlated with the degree of periostin expression (respectively, p>0.05). Occasional expression of periostin in tumor cell cytoplasm also did not reveal any specific relation with clinicopathologic parameters, although the ratio was very small (4.4~8.7%).
With regard to the degree of periostin expression, univariate survival analysis of NSCLC patients was performed by Kaplan-Meier method. Thirty-three of 40 patients with low expression were censored and 7 were died (mean and median survival times, 81.0 and 42.5 months, respectively). Thirty-five of 51 patients with high expression were censored and 16 died (mean and median survival times, 79.1 and 34.0 months, respectively). The overall survival was not related with the degree of periostin expression (p=0.126 by log-rank test, Figure 2). Additionally, multivariate Cox proportional hazards regression analysis showed independent prognostic value only in TNM-N stage (Table 4), but other factors including periostin failed to reveal significant prognostic value.
There has been a growing awareness that the cellular microenvironment throughout tumorigenesis plays a critical role in providing supportive microsurroundings for cancer cell proliferation, survival, migration and invasion16-18. Cancer cells launch various signaling pathways to respond to the altered external microenvironment19.
Periostin is a secreted protein that was originally isolated from MC3T3-E1 osteoblast cells to modulate cell adhesion as an extracellular matrix (ECM)-associated molecule20. Though structurally unrelated, it could directly interact with integrin as ECM-associated molecules. Baril et al.21 demonstrated that periostin promotes the survival of pancreas cancer cells by inducing Akt phosphorylation through binding to β4 integrin and activation of PI3 kinase pathway. Furthermore, periostin-integrin interaction may affect the ECM-integrin interaction and trigger the intracellular signaling and activation of certain genes that are involved in tumor progression9.
In the present study, the extracellular matrix protein periostin regularly showed an expression gradient in the stroma as band-like fashion immediately surrounding invasive nests of cancer cells. In NSCLC, periostin was shown to be up-regulated on mRNA level at the tumor periphery, predominantly in the stromal cells just around the carcinoma cells, with very little expression in the tumor cells themselves22. The present study also showed similar results, although it was just performed by immunohistochemical stain. The significance of this spatial distribution of periostin expression remains unclear, although the question arises if a peritumoral band-like expression of periostin in the tumor stroma facilitate invasion or rather mediate protective functions against the invading tumor. When interpreting immunohistochemical result of periostin, we originally had used four-tiered system based on the extent of the staining, as 0, 1+, and 2+, and 3+. But, we finally decided to change the system into two-tiered one to decrease possible interobserver discrepancies and improve statistical significance. Because of the small diameter of each specimen and relatively unfamiliar peritumoral imunostaining pattern, relatively concurred results compared with others were not made in this study.
In fact, clinicopathological studies revealed that periostin can serve as a prognostic marker that is overexpressed in many kinds of tumor tissues such as non-small-cell lung carcinomas, ovarian carcinoma, oral cancer, and head and neck squamous cell carcinoma23. These results suggest that periostin should play an important role in the tumor cell adhesion of NSCLC, and partly contribute its aggressive behavior. However, the serum level of periostin expression may not be associated with well-known prognostic indicators of NSCLC such as stage, tumor size and nodal status24. Interestingly, authors found that there was no relation between the expression level of periostin and progression variables such as tumor size, nodal status, stage, etc. Soltermann et al.25 reported that patients of SqCC histology, male gender, or lower age had a particularly periostin-rich stroma. On the contrary, our study result was also out of line with theirs.
Herein, high periostin expression was not correlated with advanced stage and periostin expression showed no statistical relationship with histologic type, patient age and sex. According to our results, there was no relationship with periostin expression and patient's survival from the Kaplan-Meier method for univariate survival analysis. Additionally, multivariate Cox proportional hazards regression analysis was also applied. From the analysis, only TNM-nodal stage showed independent prognostic value, but other factors including periostin failed to reveal any prognostic value. These results may be related with some limitations of this study. Thus, the demerits of the study could include a relatively small number of cases studied, a large proportion of early stage tumors (stage I in 46.2% out of the total 91 cases), and a relatively short postoperative follow-up period. In spite of the limitations, however, we presume that periostin may be not a consistent prognostic marker of NSCLC.
On the other hand, periostin expression was related with tumor differentiation. High periostin expression was correlated with moderately to poorly differentiated tumors. The result suggests that periostin expression might be related with aggressiveness of tumor cells. Further study using a large number of cases with poorly differentiated tumors is needed to confirm significance of periostin expression in tumor differentiation and aggressive behavior.
Hong et al.24 showed that periostin could promote the proliferation and migration of A549 cells (NSCLC cell line) by inducing vimentin and N-cadherin expression and downregulating E-cadherin expression. On the other hand, Shao et al.26 used three tumor cell lines to engineer stable cell lines that overexpress periostin. Unexpectedly, the proliferation rate of these periostin-producing cells was noticeably slower than that of the control cells in culture, suggesting that periostin does not promote proliferation of tumor cells in vitro. Kudo et al.11 also demonstrated that periostin overexpression does not promote cell proliferation, but it dramatically enhances the invasiveness of the head and neck cancer cell lines HSC2 and HSC3. In the present study, immunohistochemical expression levels of periostin in NSCLC were not correlated with tumor cell PCNA index (42.0±22.2% in low expression group vs. 39.7±22.3% in high group), either. Instead, the proliferation index in high expression group was slightly lower than that in low group. The expression of cyclin D1, another indicator of tumor cell proliferation, was also not related with the level of periostin expression.
Recently, it is suggested that secreted periostin interacts with αvβ5 integrins, and the intracellular signaling activation via cross-talk between integrins, and EGFR promotes the cell to undergo epithelial-mesenchymal transition (EMT), resulting in tumor invasion and metastasis27. The molecular basis of EMT in cancer cells that is a process of morphologic transdifferentiation involves multiple changes in expression, distribution, and/or function of several proteins that include periostin, vimentin, integrins, matrix metalloproteinases, and cadherins27-29. In the present study, high periostin expression was positively correlated with E-cadherin and p53 expression, but it was not related with β-catenin, a member of the wnt signaling. Cadherins are a multifunctional family of Ca2+-dependent, transmembrane glycoproteins, and their expression is known to be required for the assembly of cells into solid tissues. Importantly, E-cadherins are involved in a homotypic epithelial adhesion30. Therefore, we assumed that the expression level of periostin, an EMT-related protein, would be inversely correlated with E-cadherin. However, the result was the converse. Though the precise reason of this discordance remains unclear in this study, it might be related with a rather small sample size of NSCLC, interpretation method for immunohistochemical staining, and any character of monoclonal antibody used. Further studies would be necessary to identify the regulators of periostin in tumorigenesis.
In conclusion, these results suggest that periostin might play a role in the aggressive biologic behavior of NSCLC. However, in contrast with the previous results, their expression may not be associated with well-known prognostic indicators such as stage and tumor cell proliferation.
Figures and Tables
Figure 1
Periostin expression in tumors and intratumoral stroma (immunostain, ×200). (A) Non-neoplastic lung stroma shows negative (right) immunostaining in contrast to neoplastic stroma (left). (B) Intratumoral stoma around invasive adenocarcinoma shows positive immunoreaction. (C) The stroma of bronchioloalveolar carcinoma is negative for periostin. (D) Occasionally, the cytoplasm of adenocarcinoma cells shows positive reaction to periostin. (E) The strongest reaction in the positive stroma of squamous cell carcinoma shows a band-like pattern. (F) Intratumoral stroma of well to moderately differentiated squamous cell carcinoma shows negative staining to periostin.

Figure 2
Overall survival curves for patients with non-small cell lung carcinoma showing low expression (n=40) and high expression (n=51) of periostin.
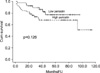
Table 2
Relationship between periostin expression in peritumoral stroma and clinicopathological parameters in non-small cell lung carcinomas

Acknowledgements
This work was supported by a grant from the National R&D Program for Cancer Control, Ministry for Health, Welfare and Family Affairs, Republic of Korea (0920050).
References
1. Horiuchi K, Amizuka N, Takeshita S, Takamatsu H, Katsuura M, Ozawa H, et al. Identification and characterization of a novel protein, periostin, with restricted expression to periosteum and periodontal ligament and increased expression by transforming growth factor beta. J Bone Miner Res. 1999. 14:1239–1249.
2. Kühn B, del Monte F, Hajjar RJ, Chang YS, Lebeche D, Arab S, et al. Periostin induces proliferation of differentiated cardiomyocytes and promotes cardiac repair. Nat Med. 2007. 13:962–969.
3. Lie-Venema H, Eralp I, Markwald RR, van den Akker NM, Wijffels MC, Kolditz DP, et al. Periostin expression by epicardium-derived cells is involved in the development of the atrioventricular valves and fibrous heart skeleton. Differentiation. 2008. 76:809–819.
4. Norris RA, Borg TK, Butcher JT, Baudino TA, Banerjee I, Markwald RR. Neonatal and adult cardiovascular pathophysiological remodeling and repair: developmental role of periostin. Ann N Y Acad Sci. 2008. 1123:30–40.
5. Norris RA, Damon B, Mironov V, Kasyanov V, Ramamurthi A, Moreno-Rodriguez R, et al. Periostin regulates collagen fibrillogenesis and the biomechanical properties of connective tissues. J Cell Biochem. 2007. 101:695–711.
6. Takayama G, Arima K, Kanaji T, Toda S, Tanaka H, Shoji S, et al. Periostin: a novel component of subepithelial fibrosis of bronchial asthma downstream of IL-4 and IL-13 signals. J Allergy Clin Immunol. 2006. 118:98–104.
7. Bao S, Ouyang G, Bai X, Huang Z, Ma C, Liu M, et al. Periostin potently promotes metastatic growth of colon cancer by augmenting cell survival via the Akt/PKB pathway. Cancer Cell. 2004. 5:329–339.
8. Siriwardena BS, Kudo Y, Ogawa I, Kitagawa M, Kitajima S, Hatano H, et al. Periostin is frequently overexpressed and enhances invasion and angiogenesis in oral cancer. Br J Cancer. 2006. 95:1396–1403.
9. Kudo Y, Siriwardena BS, Hatano H, Ogawa I, Takata T. Periostin: novel diagnostic and therapeutic target for cancer. Histol Histopathol. 2007. 22:1167–1174.
10. Puglisi F, Puppin C, Pegolo E, Andreetta C, Pascoletti G, D'Aurizio F, et al. Expression of periostin in human breast cancer. J Clin Pathol. 2008. 61:494–498.
11. Kudo Y, Ogawa I, Kitajima S, Kitagawa M, Kawai H, Gaffney PM, et al. Periostin promotes invasion and anchorage-independent growth in the metastatic process of head and neck cancer. Cancer Res. 2006. 66:6928–6935.
12. Kim CJ, Yoshioka N, Tambe Y, Kushima R, Okada Y, Inoue H. Periostin is down-regulated in high grade human bladder cancers and suppresses in vitro cell invasiveness and in vivo metastasis of cancer cells. Int J Cancer. 2005. 117:51–58.
13. Sasaki H, Lo KM, Chen LB, Auclair D, Nakashima Y, Moriyama S, et al. Expression of Periostin, homologous with an insect cell adhesion molecule, as a prognostic marker in non-small cell lung cancers. Jpn J Cancer Res. 2001. 92:869–873.
14. Sobin LH, Wittekind C. International Union against Cancer. TNM Classification of malignant tumours. 1997. 5th ed. New York: Wiley-Liss.
15. Travis WD, Colby TV, Corrin B, Shimosato Y, Brambilla E, Sobin LH. Histological typing of lung and pleural tumours. International histological classification of tumours. 1999. 3rd ed. Berlin: Springer-Verlag.
16. Hu M, Polyak K. Microenvironmental regulation of cancer development. Curr Opin Genet Dev. 2008. 18:27–34.
17. Bissell MJ, Radisky D. Putting tumours in context. Nat Rev Cancer. 2001. 1:46–54.
18. Radisky D, Hagios C, Bissell MJ. Tumors are unique organs defined by abnormal signaling and context. Semin Cancer Biol. 2001. 11:87–95.
19. López-Maury L, Marguerat S, Bähler J. Tuning gene expression to changing environments: from rapid responses to evolutionary adaptation. Nat Rev Genet. 2008. 9:583–593.
20. Takeshita S, Kikuno R, Tezuka K, Amann E. Osteoblast-specific factor 2: cloning of a putative bone adhesion protein with homology with the insect protein fasciclin I. Biochem J. 1993. 294:271–278.
21. Baril P, Gangeswaran R, Mahon PC, Caulee K, Kocher HM, Harada T, et al. Periostin promotes invasiveness and resistance of pancreatic cancer cells to hypoxia-induced cell death: role of the beta4 integrin and the PI3k pathway. Oncogene. 2007. 26:2082–2094.
22. Sasaki H, Dai M, Auclair D, Fukai I, Kiriyama M, Yamakawa Y, et al. Serum level of the periostin, a homologue of an insect cell adhesion molecule, as a prognostic marker in nonsmall cell lung carcinomas. Cancer. 2001. 92:843–848.
23. Ouyang G, Liu M, Ruan K, Song G, Mao Y, Bao S. Upregulated expression of periostin by hypoxia in non-small-cell lung cancer cells promotes cell survival via the Akt/PKB pathway. Cancer Lett. 2009. 281:213–219.
24. Hong L, Sun H, Lv X, Yang D, Zhang J, Shi Y. Expression of periostin in the serum of NSCLC and its function on proliferation and migration of human lung adenocarcinoma cell line (A549) in vitro. Mol Biol Rep. 2010. 37:2285–2293.
25. Soltermann A, Tischler V, Arbogast S, Braun J, Probst-Hensch N, Weder W, et al. Prognostic significance of epithelial-mesenchymal and mesenchymal-epithelial transition protein expression in non-small cell lung cancer. Clin Cancer Res. 2008. 14:7430–7437.
26. Shao R, Bao S, Bai X, Blanchette C, Anderson RM, Dang T, et al. Acquired expression of periostin by human breast cancers promotes tumor angiogenesis through up-regulation of vascular endothelial growth factor receptor 2 expression. Mol Cell Biol. 2004. 24:3992–4003.
27. Yan W, Shao R. Transduction of a mesenchyme-specific gene periostin into 293T cells induces cell invasive activity through epithelial-mesenchymal transformation. J Biol Chem. 2006. 281:19700–19708.
28. Larue L, Bellacosa A. Epithelial-mesenchymal transition in development and cancer: role of phosphatidylinositol 3' kinase/AKT pathways. Oncogene. 2005. 24:7443–7454.
29. Mimeault M, Batra SK. Interplay of distinct growth factors during epithelial mesenchymal transition of cancer progenitor cells and molecular targeting as novel cancer therapies. Ann Oncol. 2007. 18:1605–1619.
30. Takeichi M. Cadherin cell adhesion receptors as a morphogenetic regulator. Science. 1991. 251:1451–1455.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download