Abstract
Background
Osteopontin (Opn) is recognized as an important adhesive bone matrix protein and a key cytokine involved in immune cell recruitment and tissue repair and remolding. However, serum levels of osteopontin have not been evaluated in patients with chronic obstructive pulmonary disease (COPD). Thus, the aim of this study was to evaluate and compare the serum levels of osteopontin in patients experiencing COPD exacerbations and in patients with stable COPD.
Methods
Serum samples were obtained from 22 healthy control subjects, 18 stable COPD patients, and 15 COPD with exacerbation patients. Serum concentrations of osteopontin were measured by the ELISA method.
Results
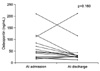
Serum levels of osteopontin were higher in patients with acute exacerbation than with stable COPD and in healthy control subjects (62.4±51.9 ng/mL, 36.9±11.1 ng/mL, 30±11 ng/mL, test for trend p=0.003). In the patients with COPD exacerbation, the osteopontin levels when the patient was discharged from the hospital tended to decrease compared to those at admission (45±52.1 ng/mL, 62.4±51.9 ng/mL, p=0.160). Osteopontin levels significantly increased according to patient factors, including never-smoker, ex-smoker and current smoker (23±5.7 ng/mL, 35.5±17.6 ng/mL, 58.6±47.8 ng/mL, test for trend p=0.006). Also, osteopontin levels showed a significantly negative correlation with forced expiratory volume in one second (FEV1%) predicted in healthy controls and stable COPD patients (r=-0.389; p=0.013). C-reactive protein (CRP) was positively correlated with osteopontin levels in patients with COPD exacerbation (r=0.775; p=0.002).
Figures and Tables
 | Figure 1Comparison of the OPN levels between healthy controls, stable COPD and COPD exacerbation. OPN level of patients with COPD exacerbation was much higher than those of healthy controls and stable COPD patients (30±11 ng/mL; 36.9±11.1 ng/mL; 62.4±51.9 ng/mL; test for trend, p=0.003). COPD: chronic obstructive pulmonary disease; OPN: Osteopontin. |
 | Figure 2Comparison of the OPN levels according to COPD severity. OPN level of stable COPD patients were increased according to COPD severity (30±11 ng/mL, 34.4±11.2 ng/mL; 43.3±8.4 ng/mL; 62.4±51.9 ng/mL; test for trend, p=0.002). OPN: osteopontin; COPD: chronic obstructive pulmonary disease. *p>0.05. |
 | Figure 3OPN levels were significantly higher, according to patients' status as never-smoked, ex-smoker, or current smoker (23±5.7 ng/mL; 35.5±17.6 ng/mL; 58.6±47.8 ng/mL; test for trend, p=0.006). OPN: osteopontin. |
 | Figure 4Relationship between CRP and OPN level in patients with COPD exacerbation. CRP was positively correlated with OPN level in patients with COPD exacerbation (r=0.775; p=0.002). CRP: C-reactive protein; COPD: chronic obstructive pulmonary disease; OPN: Osteopontin. |
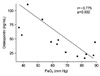 | Figure 5Relationship between PaO2 and OPN level in patients with COPD exacerbation. PaO2 was negatively correlated with OPN level in patients with COPD exacerbation (r=-0.775; p=0.002). OPN: osteopontin; COPD: chronic obstructive pulmonary disease. |
 | Figure 6Relationship between OPN and FEV1/FVC and FEV1. FEV1 percent predicted was significantly correlated with OPN level in healthy controls and stable COPD patients (r=-0.389; p=0.013). OPN: osteopontin; FEV1: forced expiratory volume in one second; FVC: force vital capacity; COPD: chronic obstructive pulmonary disease. |
References
1. O'Regan A. The role of osteopontin in lung disease. Cytokine Growth Factor Rev. 2003. 14:479–488.
2. Ashkar S, Weber GF, Panoutsakopoulou V, Sanchirico ME, Jansson M, Zawaideh S, et al. Eta-1 (osteopontin): an early component of type-1 (cell-mediated) immunity. Science. 2000. 287:860–864.
3. Chabas D, Baranzini SE, Mitchell D, Bernard CC, Rittling SR, Denhardt DT, et al. The influence of the proinflammatory cytokine, osteopontin, on autoimmune demyelinating disease. Science. 2001. 294:1731–1735.
4. Liaw L, Birk DE, Ballas CB, Whitsitt JS, Davidson JM, Hogan BL. Altered wound healing in mice lacking a functional osteopontin gene (spp1). J Clin Invest. 1998. 101:1468–1478.
5. Trueblood NA, Xie Z, Communal C, Sam F, Ngoy S, Liaw L, et al. Exaggerated left ventricular dilation and reduced collagen deposition after myocardial infarction in mice lacking osteopontin. Circ Res. 2001. 88:1080–1087.
6. Woodruff PG, Koth LL, Yang YH, Rodriguez MW, Favoreto S, Dolganov GM, et al. A distinctive alveolar macrophage activation state induced by cigarette smoking. Am J Respir Crit Care Med. 2005. 172:1383–1392.
7. King TE Jr, Savici D, Campbell PA. Phagocytosis and killing of Listeria monocytogenes by alveolar macrophages: smokers versus nonsmokers. J Infect Dis. 1988. 158:1309–1316.
8. Weber GF, Cantor H. The immunology of Eta-1/osteopontin. Cytokine Growth Factor Rev. 1996. 7:241–248.
9. Furger KA, Menon RK, Tuck AB, Bramwell VH, Chambers AF. The functional and clinical roles of osteopontin in cancer and metastasis. Curr Mol Med. 2001. 1:621–632.
10. Donati V, Boldrini L, Dell'Omodarme M, Prati MC, Faviana P, Camacci T, et al. Osteopontin expression and prognostic significance in non-small cell lung cancer. Clin Cancer Res. 2005. 11:6459–6465.
11. Chambers AF, Wilson SM, Kerkvliet N, O'Malley FP, Harris JF, Casson AG. Osteopontin expression in lung cancer. Lung Cancer. 1996. 15:311–323.
12. Brown LF, Berse B, Van de Water L, Papadopoulos-Sergiou A, Perruzzi CA, Manseau EJ, et al. Expression and distribution of osteopontin in human tissues: wide-spread association with luminal epithelial surfaces. Mol Biol Cell. 1992. 3:1169–1180.
13. Nau GJ, Guilfoile P, Chupp GL, Berman JS, Kim SJ, Kornfeld H, et al. A chemoattractant cytokine associated with granulomas in tuberculosis and silicosis. Proc Natl Acad Sci USA. 1997. 94:6414–6419.
14. O'Regan AW, Hayden JM, Body S, Liaw L, Mulligan N, Goetschkes M, et al. Abnormal pulmonary granuloma formation in osteopontin-deficient mice. Am J Respir Crit Care Med. 2001. 164:2243–2247.
15. Miyazaki Y, Tashiro T, Higuchi Y, Setoguchi M, Yamamoto S, Nagai H, et al. Expression of osteopontin in a macrophage cell line and in transgenic mice with pulmonary fibrosis resulting from the lung expression of a tumor necrosis factor-alpha transgene. Ann N Y Acad Sci. 1995. 760:334–341.
16. Takahashi F, Takahashi K, Okazaki T, Maeda K, Ienaga H, Maeda M, et al. Role of osteopontin in the pathogenesis of bleomycin-induced pulmonary fibrosis. Am J Respir Cell Mol Biol. 2001. 24:264–271.
17. Pardo A, Gibson K, Cisneros J, Richards TJ, Yang Y, Becerril C, et al. Up-regulation and profibrotic role of osteopontin in human idiopathic pulmonary fibrosis. PLoS Med. 2005. 2:e251.
18. Gan WQ, Man SF, Senthilselvan A, Sin DD. Association between chronic obstructive pulmonary disease and systemic inflammation: a systematic review and a meta-analysis. Thorax. 2004. 59:574–580.
19. Madsen KM, Zhang L, Abu Shamat AR, Siegfried S, Cha JH. Ultrastructural localization of osteopontin in the kidney: induction by lipopolysaccharide. J Am Soc Nephrol. 1997. 8:1043–1053.
20. Furger KA, Menon RK, Tuck AB, Bramwell VH, Chambers AF. The functional and clinical roles of osteopontin in cancer and metastasis. Curr Mol Med. 2001. 1:621–632.
21. Schneider DJ, Lindsay JC, Zhou Y, Molina JG, Blackburn MR. Adenosine and osteopontin contribute to the development of chronic obstructive pulmonary disease. FASEB J. 2010. 24:70–80.
22. Rittling SR, Denhardt DT. Osteopontin function in pathology: lessons from osteopontin-deficient mice. Exp Nephrol. 1999. 7:103–113.
23. Ham HS, Lee HY, Lee SJ, Cho YJ, Jung YY, Kim HC, et al. Relationship between systemic inflammatory marker, oxidative stress and body mass index in stable COPD patient. Tuberc Respir Dis. 2006. 61:330–338.
24. MacNee W. Pulmonary and systemic oxidant/antioxidant imbalance in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:50–60.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download