Abstract
Background
Chronic obstructive pulmonary disease (COPD) is characterized by air flow limitation, which is one of the leading causes of mortality worldwide. There have been many studies on survival rates in the world literature, but there have been few reports regarding the survival rate in Korean patients with COPD. Acute exacerbation is regarded as a risk factor for mortality in patients with COPD. The purpose of this study was to investigate the survival rate and the effect of acute exacerbations on the survival rate of Korean patients with COPD.
Methods
A total of 502 COPD patients who were diagnosed on the basis of history and lung function tests were enrolled in this study. The frequency of acute exacerbations, body mass index (BMI), C-reactive protein (CRP) and pulmonary hypertension were analyzed.
Results
The 3- and 5-year survival rates were 98% and 83%, respectively. The median survival time was 78 months. The median survival time was 55 months in 322 patients with one or more acute exacerbations. The 3- and 5-year survival rates were significantly lower in the 322 patients with one or more acute exacerbations than in those without any. The mortality rate was significantly higher in patients with CRP >3 mg/L than in those with CRP ≤3 mg/L (p<0.005); it was significantly higher in patients with pulmonary hypertension than in those without it (p<0.01).
Chronic obstructive pulmonary disease (COPD) is a disease entity that is characterized by airway obstruction due to pulmonary inflammatory reactions1. The incidence of COPD has recently been increasing. COPD ranked sixth among the causes of death in humans in the 1990s, but it is estimated to rank third by 20202. Of the Korean population, 17.2% have airway obstruction where the forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) ratio is <0.7, emphasizing the clinical implications of COPD3.
In Japan, the 5-year survival rate was reported to be 73% in 183 patients with COPD4. The 3-year survival rate was reported to be 85% in patients with COPD who had not received any treatments5. However, there have been few studies on the survival rate in Korean patients with COPD.
A previous cross-sectional study reported that the mortality rate increased to 2.5% in COPD patients with acute exacerbations6. Additionally, acute exacerbation can reduce long-term survival in patients with COPD7,8. However, little is known about the difference in survival between patients with acute exacerbations and those without in Korea. It is generally recognized that prognosis and mortality are associated with various factors such as airflow obstruction, hypoxemia, pulmonary hyperinflation, anemia, body mass index (BMI: body weight [kg]/body surface area [m2]) and dyspnea9,10. COPD has recently been shown to be a systemic inflammatory disease1. It has been reported that C-reactive protein (CRP) has an overt effect on survival of patients with COPD11.
Therefore, this study was conducted to investigate the survival rate of Korean patients with COPD and to determine whether acute exacerbation and several clinical factors would affect their long-term survival.
This retrospective study included COPD patients with a pre-bronchodilator FEV1/FVC ratio of <0.7 who met the following criteria: 1) negativity for bronchial provocation tests or 2) changes in FEV1 by <200 mL or by <15% after administration of salbutamol, a bronchodilator (400µg). Patients with a previous history of bronchial asthma or significant radiologic findings suggestive of pulmonary dysfunction were excluded from the study. The protocol of this study was approved by the local ethics committee.
A COPD exacerbation was defined as an event in the natural course of the disease characterized by a change in the patient's baseline dyspnea, cough and/or sputum that was beyond normal day-to-day variations, was acute in onset, and warranted a change in regular medication in a patient with underlying COPD1.
Pulmonary function tests were performed by a technician who was well trained with the tests according to the 1994 American Thoracic Society (ATS) guidelines12. The tests included FVC, FEV1, FEV1/FVC ratio, diffusion capacity for carbon dioxide, TLC and RV. The severity of COPD was categorized into 4 stages from stage I to stage IV using the GOLD criteria according to the estimate of FEV1 1.
To investigate the association between clinical characteristics and survival, BMI and CRP values were measured at the time of diagnosis. The presence and patterns of pulmonary emphysema were assessed by high-resolution computed tomography (HRCT), and the presence of pulmonary hypertension was assessed by echocardiography.
All statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA) for Windows. The data are expressed as mean±standard deviation (SD). Comparisons of variables were made with the t-test, the Wilcoxon rank sum test and the Pearson chi-square test. The survival rate was analyzed using the Kaplan-Meier method. The variables affecting survival were analyzed using a multiple logistic regression model. A p-value of <0.05 was considered statistically significant.
A total of 502 patients were enrolled for this study, and there were 444 males and 58 females. The mean age was 70±9 years for all patients. It was 69±9 years for male patients and 74±10 years for female patients, with significant difference (p<0.05). The man FEV1 was 57±24% for all patients; 17% for stage I (n=85), 41% for stage II (n=206), 30% for stage III (n=151) and 12% for stage IV (n=60). The mean FEV1 was 56±23% for male patients and 61±25% for female patients. The mean BMI was 21.7±3.8 for male patients and 22.4±3.8 for female patients without any significant difference. Smoking was related to COPD in 92% of the male patients; 58% were current smokers, and 35% were ex-smokers. Smoking was related to COPD in only 70% of the female patients; 53% were current smokers, and 17% were ex-smokers (Table 1).
The number of deaths was 55 (mortality rate, 11%) for all patients, 44 (the mortality rate, 10%) for the male patients and 11 (mortality rate, 20%) for the female patients. Since the male patients were older than the female patients, the morality rate of patients aged ≥70 years was compared between both sexes. There were 235 male patients aged ≥70 years, of whom 32 died (mortality rate, 14%). There were 42 female patients aged ≥70 years, of whom 7 died (mortality rate, 17%). This difference was not statistically significant.
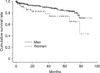
The overall median survival time was 78 months, and the 3-year and 5-year survival rate were 98% and 83%, respectively. Although there were fewer females than males, the morality rate was significantly higher in females than in males (Table 1). Additionally, the cumulative survival rate was significantly higher in males than in females (p<0.05). The mean survival time was 80 months for the male patients and 66 months for the female patients. The 3-year and 5-year survival rates were 90% and 84%, respectively, for the male patients, and 78% and 74% for the female patients, respectively (Figure 1).
Of a total of 502 patients with COPD, 322 suffered acute exacerbations of COPD. The most common cause of acute exacerbation was infection (78%), followed by congestive heart failure (4.0%), pneumothorax (2.3%), pulmonary embolism (1.7%), other diseases (3.7%) and unknown etiologies (3.7%). One acute exacerbation was observed in 190 patients, 2 acute exacerbations in 67 patients, 3 acute exacerbations in 24 patients, 4 acute exacerbations in 12 patients, and ≥5 acute exacerbations in 29 patients. The median survival time was 55 months for patients who suffered only 1 acute exacerbation. There was a significant difference in the cumulative survival rate between patients with no experience of acute exacerbations and those with 1 ≥ acute exacerbations (p=0.01, Figure 1), and also, this difference was observed between only 1 acute exacerbation and those with ≥2 acute exacerbations (p=0.001, Figure 2).
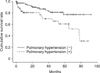
Based on the result of previous studies that COPD is frequently associated with weight loss and is a systemic inflammatory disease, the survival rate was analyzed in terms of BMI and CRP. Patients were categorized into 3 groups: those with BMI ≤20, those with 20< BMI <25 and those with BMI ≥25. There were no significant differences between the 3 groups (Figure 2). By using categories of CRP ≤3 and CRP >3, patients with CRP >3 showed a lower survival rate than those with CRP ≤3 (p=0.001). By using categories of CRP ≤5, 5 < CRP <15 and CRP ≥15, the cumulative survival rate significantly decreased with increasing CRP value (p<0.001) (Figure 3).
Pulmonary hypertension was defined as a value of ≥20 mm Hg. The mortality rate was analyzed in 167 patients who underwent echocardiography according to the absence/presence of pulmonary hypertension in a multiple logistic regression model. The mortality rate was approximately 3 times higher in patients with pulmonary hypertension than in those without (p<0.005). The cumulative survival rate was significantly higher in patients without pulmonary hypertension (p<0.001) (Figure 4).
The mortality rate was investigated according to the patterns of pulmonary emphysema assessed by HRCT. Patients were divided into 4 groups: those with a centrilobular pattern, those with a mixed pattern, those with a panlobular pattern and those without emphysema. There were no significant differences in the mortality rate between the 4 groups (Table 2).
The aim of this study was to investigate the survival rate of Korean patients with COPD. In this study, the 5-year survival rate was found to be 83% for Korean patients with COPD, whereas it was reported to be 45~73% in other ethnic group4,13,14. This difference can be explained by the following reasons. The first reason may be that the survival time studied differed between the international reports and ours. Furthermore, there have been few reports on the 5-year survival rate in previous reports. The second reason may be an ethnic difference considering that the 5-year survival rate was reported to be 73% in Japanese patients4, another Asian ethnic group.
The definition of COPD differs among investigators; some investigators define it according to changes in clinical symptoms1,15,16, and others define it according to responses to treatments17. Although the frequency of acute exacerbation may differ due to its different definition, it has not yet been determined which definition would be appropriate. In most studies, COPD was defined according to changes in clinical symptoms. In our study, the survival rate was lower in patients who suffered ≥1 acute exacerbations of COPD. Soler-Cataluna et al18 reported a similar result that in 304 patients with COPD, the 5-year survival rate was 80% for those with ≤3 acute exacerbations and 30% for those with ≥4 acute exacerbations. Based on these results, it is conceivable that acute exacerbation of COPD may reduce the survival rate in the Korean and other ethnic groups. Therefore, it is indicated that the prevention of acute exacerbation of COPD may increase the survival rate and improve the quality of life.
The results of this study are subjected to some limitations. First, 30% of the female patients with COPD did not have relations to smoking. Although all risk factors could not be detected only based on a carefully taken history, many women appeared to inhale smoke while cooking because they used heat produced by burning wood in Korea in the past. This point is supported by the result that indoor smoke is a risk factor for COPD in developing countries19,20. In addition, to avoid chronic persistent airway obstruction due to airway remodeling in patients with asthma21, those with a previous history of asthma or those with responsiveness to bronchodilators were excluded from the study. Second, in our study, the survival rate was not significantly different according to FEV1 values at the time of diagnosis (p=0.753, data not shown). However, many studies have shown that the initial FEV1 value is closely related to prognosis of COPD13,22. The reason for this difference may be explained by the fact that FEV1 values were taken before administration of bronchodilators in our study. It is thought that if we used FEV1 values taken after administration of bronchodilators, our result may have been similar to those of the aforementioned studies.
Although COPD is characterized by airway obstruction, it is well known as a systemic inflammatory disease1. Thus, various systemic diseases are frequently associated with COPD1,23. CRP, a marker for systemic inflammatory disease, is closely related to age, body weight, dyspnea, quality of life, physical activities and degree of airway obstruction in patients with COPD24,25. A previous study with a limited number of patients with moderate to severe COPD has suggested that CRP is related to the degree of cardiovascular disease and its mortality rate, whereas it is not related to the survival rate of COPD26. In our study, the survival rate of patients with COPD significantly decreased as CRP values increased, implying that COPD is a systemic disease. Based on these results, it is believed that CRP can be used as a biological marker for COPD.
Although weight loss has not yet been elucidated as a definite etiologic factor for COPD, skeletal muscle dysfunction is related to COPD as well as other chronic diseases such as cardiovascular disease27. However, simple weight loss is an independent predictor of prognosis of COPD28. In addition, Landbo et al29 have demonstrated that a decrease in muscle volume is closely related to prognosis of COPD on the basis of the result that weight gain resulted in better prognosis. It has been shown that BMI is significantly related to the survival rate of patients with COPD30. Conversely, in our study, it was found that BMI was not significantly related to the survival rate of patients with COPD. This result may be attributed to the fact that the proportions of patients according to the severity of COPD were different between the previous study and ours. In our study, patients with stage III/IV accounted for 42% of all patients, whereas in the aforementioned study, they accounted for 6%. In our study, BMI significantly decreased as severity of COPD increased as shown in Table 1, which was similar to the results of the aforementioned study. Therefore, it is thought that there was no specific problem in the measurement of BMI in our study.
Pulmonary hyperinflation, which is a characteristic finding of COPD, can be diagnosed by radiological studies including simple chest X-rays and CT31,32, but there is still no definite diagnostic method. Although our previous study has documented that radiologic quantity of hyperinflation assessed by HRCT can be used as an objective marker for dyspnea of patients with COPD33, the presence and patterns of pulmonary emphysema were not significantly related to their survival rates.
In this study, women were found to be at a higher risk of death. This results are compatible the other study conducted by Machado et al34. After adjusting for age, pack-years smoked, arterial oxygen tension, FEV1, and body mass index, they found women had a poor prognosis than men. But, recent report showed mean survival and time to rehospitalization time for obstructive airway diseases are significantly better for woman35. These findings suggest there is no good explanation of a higher risk of death in women.
In summary, the 5-year survival rate was 83% for Korean patients with COPD, which was slightly higher than those reported by international studies. The results of this study suggest that acute exacerbation of COPD may decrease the survival rate. Therefore, the prevention of acute exacerbation should be considered in the management of patients with COPD.
Figures and Tables
Figure 2
There were no differences of cumulative survival rate between the 3 groups divided by the level of BMI. BMI: body mass index.
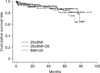
Figure 3
The cumulative survival rate significantly decreased with increasing CRP value (p<0.001). CRP: C-reactive protein.

Figure 4
The cumulative survival rate was significantly higher in patients without pulmonary hypertension compared to that in those with (p<0.001).
Acknowledgements
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A090548).
References
1. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007. 176:532–555.
2. Chapman KR, Mannino DM, Soriano JB, Vermeire PA, Buist AS, Thun MJ, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006. 27:188–207.
3. Kim DS, Kim YS, Jung KS, Chang JH, Lim CM, Lee JH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. Am J Respir Crit Care Med. 2005. 172:842–847.
4. Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002. 121:1434–1440.
5. Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007. 356:775–789.
6. Patil SP, Krishnan JA, Lechtzin N, Diette GB. In-hospital mortality following acute exacerbations of chronic obstructive pulmonary disease. Arch Intern Med. 2003. 163:1180–1186.
7. Ai-Ping C, Lee KH, Lim TK. In-hospital and 5-year mortality of patients treated in the ICU for acute exacerbation of COPD: a retrospective study. Chest. 2005. 128:518–524.
8. Berkius J, Nolin T, Mårdh C, Karlström G, Walther SM. Swedish Intensive Care Registry. Characteristics and long-term outcome of acute exacerbations in chronic obstructive pulmonary disease: an analysis of cases in the Swedish Intensive Care Registry during 2002-2006. Acta Anaesthesiol Scand. 2008. 52:759–765.
9. Gerardi D, ZuWallack R. Non-pulmonary factors affecting survival in patients completing pulmonary rehabilitation. Monaldi Arch Chest Dis. 2001. 56:331–335.
10. Ringbaek T, Seersholm N, Viskum K. Standardised mortality rates in females and males with COPD and asthma. Eur Respir J. 2005. 25:891–895.
11. Dahl M, Vestbo J, Lange P, Bojesen SE, Tybjaerg-Hansen A, Nordestgaard BG. C-reactive protein as a predictor of prognosis in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2007. 175:250–255.
12. American Thoracic Society. Standardization of sirometry, 1994 update. Am J Respir Crit Care Med. 1995. 152:1107–1136.
13. Postma DS, Gimeno F, van der Weele LT, Sluiter HJ. Assessment of ventilatory variables in survival prediction of patients with chronic airflow obstruction: the importance of reversibility. Eur J Respir Dis. 1985. 67:360–368.
14. Vestbo J, Prescott E, Lange P, Schnohr P, Jensen G. Vital prognosis after hospitalization for COPD: a study of a random population sample. Respir Med. 1998. 92:772–776.
15. Kanner RE, Renzetti AD Jr, Klauber MR, Smith CB, Golden CA. Variables associated with changes in spirometry in patients with obstructive lung diseases. Am J Med. 1979. 67:44–50.
16. Monto AS, Higgins MW, Ross HW. The Tecumseh study of respiratory illness. VIII. Acute infection in chronic respiratory disease and comparison groups. Am Rev Respir Dis. 1975. 111:27–36.
17. Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000. 320:1297–1303.
18. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005. 60:925–931.
19. Boman C, Forsberg B, Sandström T. Shedding new light on wood smoke: a risk factor for respiratory health. Eur Respir J. 2006. 27:446–447.
20. Ezzati M. Indoor air pollution and health in developing countries. Lancet. 2005. 366:104–106.
21. Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, FitzGerald M, et al. Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J. 2008. 31:143–178.
22. Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. A 15-year follow-up study. Am Rev Respir Dis. 1979. 119:895–902.
23. Wouters EF. Local and systemic inflammation in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005. 2:26–33.
24. Pinto-Plata VM, Müllerova H, Toso JF, Feudjo-Tepie M, Soriano JB, Vessey RS, et al. C-reactive protein in patients with COPD, control smokers and non-smokers. Thorax. 2006. 61:23–28.
25. de Torres JP, Cordoba-Lanus E, López-Aguilar C, Muros de Fuentes M, Montejo de Garcini A, Aguirre-Jaime A, et al. C-reactive protein levels and clinically important predictive outcomes in stable COPD patients. Eur Respir J. 2006. 27:902–907.
26. de Torres JP, Pinto-Plata V, Casanova C, Mullerova H, Córdoba-Lanús E, Muros de Fuentes M, et al. C-reactive protein levels and survival in patients with moderate to very severe COPD. Chest. 2008. 133:1336–1343.
27. Gosker HR, Wouters EF, van der Vusse GJ, Schols AM. Skeletal muscle dysfunction in chronic obstructive pulmonary disease and chronic heart failure: underlying mechanisms and therapy perspectives. Am J Clin Nutr. 2000. 71:1033–1047.
28. Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is a reversible factor in the prognosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998. 157:1791–1797.
29. Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999. 160:1856–1861.
30. Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, et al. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. 2006. 173:79–83.
31. Nakano Y, Muro S, Sakai H, Hirai T, Chin K, Tsukino M, et al. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am J Respir Crit Care Med. 2000. 162:1102–1108.
32. Rothpearl A, Varma AO, Goodman K. Radiographic measures of hyperinflation in clinical emphysema. Discrimination of patients from controls and relationship to physiologic and mechanical lung function. Chest. 1988. 94:907–913.
33. Jung EJ, Kim YK, Lee YM, Kim KU, Uh S, Kim YH, et al. The Correlation of dyspnea and radiologic quantity in patients with COPD. Tuberc Respir Dis. 2009. 66:288–294.
34. Machado MC, Krishnan JA, Buist SA, Bilderback AL, Fazolo GP, Santarosa MG, et al. Sex differences in survival of oxygen-dependent patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006. 174:524–529.
35. Gonzalez AV, Suissa S, Ernst P. Gender differences in survival following hospitalisation for COPD. Thorax. 2011. 66:38–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download