Abstract
Background
The aim of the study was to describe the characteristics, treatments, and outcomes of critically ill patients with pandemic Influenza A/H1N1 2009 at a major medical center in Korea.
Methods
This retrospective observational study examined critically ill adult patients with pandemic Influenza A/H1N1 2009, who were admitted to the AMC between August and December 2009.
Results
27 patients with confirmed pandemic Influenza A/H1N1 2009 were admitted to the intensive care unit (ICU) at the Asan Medical Center (AMC). The median age (IQR) was 59 years (41~67), and 66.7% of the patients were older than 51 years. A total of 81.5% of the patients had 2 or more co-morbidities. The median time (IQR) from symptom onset to presentation was 2 days (1~4), and the median time from presentation to ICU admission was 0 days (0~1.5). All patients received oseltamivir (300 mg/day) and 13 patients received triple combination therapy (oseltamivir, amantadine, ribavirin). Twelve patients required mechanical ventilation on the first day of ICU admission. A total of 6 patients (22.2%) died within 28 days of admission. The patients who died had significantly higher acute physiology and chronic health evaluation (APACHE) II and sequential organ failure assessment (SOFA) scores at presentation. There were no significant differences in age, co-morbidities, or antiviral regimens between survivors and non-survivors.
Conclusion
Critical illness related to pandemic Influenza A/H1N1 2009 was common in elderly patients with chronic co-morbidities. All patients were given high-dose oseltamivir or triple combination antiviral therapy. Nonetheless, patients with critical illnesses associated with pandemic Influenza A/H1N1 2009 had a death rate of 22.2%.
In early April 2009, there were reports of human infection with Influenza A/H1N1 2009 in southern California and Mexico, and by late April the virus had spread to other regions of the world1. On June 11, 2009, the 2009 H1N1 pandemic led the World Health Organization to declare the first phase-6 global influenza pandemic of the century2.
In Korea, the first case of pandemic Influenza A/H1N1 2009 was documented on May 2, 2009. Since then, confirmed Korean cases were reported mainly in overseas travelers or those who had direct contact with infected people. By October, 2009, the incidence of pandemic Influenza A/H1N1 2009 was significantly greater, and by April 17, 2010, there were about 750,000 Korean patients with confirmed pandemic Influenza A/H1N1 2009, 252 of whom had died3. Several countries of the northern and southern hemispheres that experienced pandemic Influenza A/H1N1 2009 have reported the clinical features and disease course of critically ill patients4-7. However, there is little information available on Korean patients who were critically ill with pandemic Influenza A/H1N1 2009.
Here, we describe the characteristics, clinical features, treatments, and outcomes of Korean patients who were critically ill with pandemic Influenza A/H1N1 2009. We expect that this information may be helpful in the establishment of public health policies, identification of critically ill patients, and for comparisons with other geographical regions and races.
We retrospectively reviewed the records of all patients with confirmed pandemic Influenza A/H1N1 2009 related critical illnesses from August 26 to December 31, 2009 who were treated at the Asan Medical Center (AMC), a 2,800-bed, tertiary referral hospital in Seoul, Korea. This study was approved by the Institutional Review Board. Informed consent was not necessary because this was not an interventional study.
All eligible patients were aged at least 15 years, were critically ill, and were admitted to our hospital with confirmed pandemic Influenza A/H1N1 2009. Confirmation was determined by a positive result from a probe-based reverse-transcriptase polymerase-chain-reaction (RT-PCR) for 2009 H1N1 virus from a nasopharyngeal swab or broncho-alveolar lavage (BAL). Critically ill patients were defined as those who 1) were admitted to the ICU or required mechanical ventilation (invasive or noninvasive); 2) had a ratio of partial pressure of oxygen in arterial blood (PaO2) to inspired fraction of oxygen (FIO2) less than 300 mm Hg; or 3) required intravenous infusion of an inotropic or vasopressor medication.
We reviewed the medical records and recorded the following data: dates of admission to the hospital and ICU, age, sex, weight and height (for calculation of body mass index [BMI]), date of first symptoms, presence and type of influenza syndrome, laboratory data, radiographic findings, and comorbidities. Severity of illness was assessed using the acute physiology and chronic health evaluation (APACHE) II and the sequential organ failure assessment (SOFA) scores on the day of admission.
Continuous variables are presented as medians and interquartile ranges (IQRs). For categorical variables, the percentage of patients in each category is given. To test for the significance of differences in baseline characteristics between survivors and non-survivors, the Mann-Whitney test was used for continuous variables and the χ2 test or Fisher's exact test was used for discrete variables. A p value less than 0.05 was considered to indicate statistical significance. All analyses were performed with SPSS for Windows release 12.0 (SPSS Inc., Chicago, IL, USA).
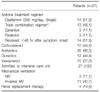
At the AMC, the first critically ill patient with pandemic Influenza A/H1N1 2009 was identified on August 26, 2009. Subsequently, there were 3 cases in September, 5 in October, 12 in November, and 6 in December. Median patient age was 59 years and 70.4% of patients were male. Table 1 shows additional characteristics of the 27 study patients. Three cases were due to nosocomial transmission, none of these patients were healthcare workers. At initial presentation, the median (IQR) APACHE II score was 17.0 (11.5~24.0). Twenty-two (81.5%) patients had two or more comorbidities. The median number of comorbid conditions was 2 (IQR, 1~3). The most common comorbidities were smoking (44.4%), malignancy (40.7%), chronic lung disease (25.9%), hypertension (25.9%), and diabetes (22.2%). The median BMI (IQR) was 23.3 (20.3~24.8), and 3 patients (11.1%) were obese (BMI >30). None of our patients were pregnant. The most common presenting symptoms were respiratory symptoms such as cough (81.5%), sputum production (63.0%), shortness of breath (70.4%), and fever (77.8%). Leukocytosis was present in 44.4% of patients and lymphopenia was present in 81.5% of patients (Table 2). Based on chest radiography at presentation, 20 patients (74.1%) had bilateral infiltrates.
The median time (IQR) from symptom onset to presentation was 2 days (1~4) and the median time from presentation to ICU admission was 0 days (0~1.5). Most patients (66.7%) had acute respiratory distress syndrome or viral pneumonia, and two patients (7.4%) were diagnosed with concurrent bacterial pneumonia at presentation (one due to Staphylococcus aureus, one due to Streptococcus pneumoniae). Other concomitant conditions included exacerbation of asthma or chronic obstructive pulmonary disease (14.8%), congestive heart failure (7.4%), and ischemic chest pain (3.7%).
All patients received oseltamivir (300 mg/day) and 13 patients received a triple combination regimen (oseltamivir, amantadine, ribavirin) (Table 3). About half of the patients were given antiviral therapy within 48 hours of symptom onset. The other medical treatments included antibiotics (26 patients, 96.3%), corticosteroids (12 patients, 44.4%), and diuretics (12 patients, 44.4%). Inotropes or vasopressors were given to 7 patients (25.9%) on the day of presentation. Twelve patients (44.4%) required mechanical ventilation on the first day of ICU admission, 9 (33.4%) of these procedures were invasive and 3 (11.1%) were noninvasive. Two of the three patients who received noninvasive ventilation ultimately required invasive ventilation. Rescue therapies for oxygenation failure required neuromuscular blockade in nine patients (33.3%), inhaled nitric oxide in four patients (14.8%), prone positioning ventilation in four patients (14.8%), and extracorporeal membrane oxygenation in two patients (7.4%). Barotrauma occurred in two patients during mechanical ventilation. Hospital-acquired pneumonia or ventilator-associated pneumonia developed in five patients during the course of treatment (two from methicillin-resistant Staphylococcus aureus, two from carbapenem-resistant Acinetobacter baumannii, and one from Klebsiella pneumonia).
Among our 27 patients, 6 died, 19 recovered and were discharged from the hospital within 24 days, and 2 remained in the hospital more than 60 days. Of the six patients who died, two patients died within the first 14 days of onset of critical disease and all six died within 28 days from critical disease onset (Table 4). The median (IQR) length of ICU stay was 5 days (3~8) for all patients, 5 days (3~7) for survivors and 19.5 days (7~20.8) for non-survivors. The median (IQR) duration of ventilation was 9 days (3~21) for all patients, 4.5 days (2.5~8) for survivors and 20 days (19~21) for non-survivors. The median (IQR) length of hospitalization among all cases was 7.5 days (5~20).
Five of the six patients who died were more than 51 years old (Figure 1). Four of these six patients had malignancies and the other two were chronic alcohol abusers. Two of the three patients who were infected by nosocomial transmission died.
Patients who died had significantly higher APACHE II and SOFA scores at presentation (Table 5). There were no significant differences in age, sex, comorbidities, and antiviral regimens between survivors and non-survivors. Most non-survivors began treatment with antiviral agents at 48 hours or longer from symptom onset, but this was not significantly different from that for survivors (p=0.077).
In our study population, we found that critical illness related to pandemic Influenza A/H1N1 2009 was most common in elderly patients with multiple comorbidities, and that mortality was greater in elderly patients. In our patients, chronic lung disease and malignancy (solid cancer or hematologic malignancy) were common comorbidities, but, in contrast to other studies4,5,7, obesity was rare, and none of our patients was pregnant. Although there was not a statistically significant difference in the time from symptom onset to initiation of antiviral agents between survivors and non-survivors, most non-survivors began antiviral agents more than 48 hours after symptom onset. All patients were given high-dose oseltamivir or triple combination therapy, and there was no significant difference in survival rate between these two treatment groups.
Several early reports indicated that critical illnesses related to pandemic Influenza A/H1N1 2009 were more common in young patients than is typically observed for seasonal influenza4,5,7,8. This may be because elderly patients are more likely to have cross-reactive antibodies to 2009 H1N1 due to their exposure to a related 1957 influenza virus9. According to a previous epidemiologic report, most deaths associated with pandemic Influenza A/H1N1 2009 (51%) were middle-aged patients (age, 20~49 years)10. However, in our Korean population, patients older than 51 years were more likely to die and more likely to be admitted to an ICU. In a global survey of 2009 H1N1 mortality, Vaillant et al.10 reported that 12% of deaths were in patients aged at least 60 years, but that 36% of reported deaths in Canada and 28% of reported deaths in Australia were in patients aged at least 60 years. Additionally, a pandemic Influenza A/H1N1 2009 study by Louie et al.6 reported that persons aged at least 50 years in California had the highest mortality rates once hospitalized. Thus, the pandemic Influenza A/H1N1 2009 mortality rate seems to depend on geography and/or race.
Pandemic Influenza A/H1N1 2009 is associated with many of the same comorbidities as seasonal influenza, in addition to obesity and pregnancy4-7,10. In this study, more than 80% of our patients had a comorbidity such as malignancy (solid cancer or and hematologic malignancy) and chronic lung disease. The high incidence of malignancy among our patients may be explained by the fact that this study was conducted at a tertiary referral hospital. Patients with malignant diseases are immunocompromised, and death from influenza-related infections has been reported to be more common in cancer patients11. However, in contrast to other populations, only 11% of our patients were obese. This is presumably related to the low rate of obesity in Korea. A recent report indicated that Korea has the lowest obesity rate (3.5%) among all OECD nations12. None of our patients was pregnant and there has been only one reported case of pandemic Influenza A/H1N1 2009 associated mortality in a pregnant woman in Korea3.
In this study, the time from symptom onset to hospitalization was less than in most previous reports. However, only half of our patients received antiviral agents within 48 hours of symptom onset. There was no statistical difference in the time from symptom onset to initiation of antiviral agent between survivors and non-survivors (2 days vs. 4.5 days, respectively), but non-survivors tended to receive treatment for longer after symptom onset. Moreover, only one of the six patients who died received an antiviral agent within 48 hours of symptom onset. Recent reports of Canadian and Taiwanese patients showed that severe pandemic Influenza A/H1N1 2009 that required admission to the ICU was associated with a longer time from symptom onset to initiation of antiviral therapy13,14. Zarychanski et al.14 reported that the median time from symptom onset to initiation of antiviral therapy was 2 days for patients with community-acquired disease, 4 days for patients admitted to hospital, and 6 days for those admitted to an ICU. Moreover, delayed administration of antiviral agent (s) was the strongest predictor of respiratory failure and death in those studies13,14.
Some reports have indicated that high-dose oseltamivir (300 mg/day) may be more effective for H5N1 (avian influenza) patients with severe pulmonary disease15. Nguyen et al.16 reported that the drugs in the triple combination treatment (oseltamivir, amantadine, ribavirin) acted synergistically against influenza A virus. In particular, they found that the triple combination therapy had 2-fold to 13-fold greater potency (depending on the influenza virus subtype) than any double combination. At present, there are insufficient clinical data on the efficacy of high-dose oseltamivir or triple combination regimens in treatment of pandemic Influenza A/H1N1 2009. Our pandemic Influenza A/H1N1 2009 patients received high-dose oseltamivir or triple combination therapy, and there was no difference in antiviral regimens between survivors and non-survivors. However, this study was limited in direct comparisons between the single regimen and triple regimen because the follow-up RT-PCR data were insufficient and more severely ill patients were more likely to receive the triple regimen rather than the single regimen. In Taiwan, some patients received oseltamivir at a dose of 150 mg twice-daily, but oseltamivir dosage was not significantly associated with death13. We suggest that future research assesses the effects of different treatment regimens for pandemic Influenza A/H1N1 2009.
This study has several limitations. First, the retrospective design could have led to selection bias. Second, we could have missed certain relevant patient data, such as history of vaccination. Third, this study was conducted at a single institution and only included patients who were aged at least 15 years. Thus, it is possible that we underestimated the number of young and healthy patients infected with pandemic Influenza A/H1N1 2009.
In our Korean population, elderly patients with chronic comorbidities, especially malignancy or chronic lung disease, were more likely to have a critical illness related to pandemic Influenza A/H1N1 2009 infection and were more likely to die from this infection. In contrast to other study populations, obesity and pregnancy were unrelated to pandemic Influenza A/H1N1 2009 infection or mortality. All of our patients received high-dose oseltamivir or triple combination antiviral regimen after hospital admission. Nonetheless, respiratory failure progressed rapidly in some patients, necessitating prolonged mechanical ventilation and/or frequent use of rescue therapies. In our population, patients with critical illnesses associated with pandemic Influenza A/H1N1 2009 had a death rate of 22.2%.
Figures and Tables
Figure 1
Age distribution of 27 critically ill patients with confirmed pandemic Influenza A/H1N1 2009.

Table 1
Demographic characteristics of critically ill patients with confirmed pandemic Influenza A/H1N1 2009

Table 2
Laboratory and radiographic findings on admission of critically ill patients with confirmed pandemic Influenza A/H1N1 2009

Acknowledgements
We thank Kil H, Jo EM and Lee NY for their assistance in the statistical review and the preparation of the manuscript. Lastly, we acknowledge an informative and insightful review by an anonymous reviewer.
References
1. Centers for Disease Control and Prevention (CDC). Swine influenza A (H1N1) infection in two children--Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009. 58:400–402.
2. Global alert and response, pandemic (H1N1) 2009, frequently asked questions: what is phase 6? [Internet]. World Health Organization. c2011. cited 2011 Jan 10. Geneva: WHO;Available from: http://www.who.int/csr/disease/swineflu/frequently_asked_questions/levels_pandemic_alert/en/index.html.
3. KCDC Newsletters [Internet]. Korea Centers for Disease Control and Prevention. c2011. cited 2011 Jan 10. Cheongwon: KCDC;Available from: http://www.cdc.go.kr/kcdchome/jsp/home/common/brd/COMMBRD0200List.jsp?menuid=100047&contentid=null&boardid=1010&appid=&pageNum=1&sub=1&sub2=2&tabinx=1&q_had01=A&q_had02=2011&loadType=null&boardseq=null.
4. Domínguez-Cherit G, Lapinsky SE, Macias AE, Pinto R, Espinosa-Perez L, de la Torre A, et al. Critically ill patients with 2009 influenza A (H1N1) in Mexico. JAMA. 2009. 302:1880–1887.
5. Kumar A, Zarychanski R, Pinto R, Cook DJ, Marshall J, Lacroix J, et al. Critically ill patients with 2009 influenza A (H1N1) infection in Canada. JAMA. 2009. 302:1872–1879.
6. Louie JK, Acosta M, Winter K, Jean C, Gavali S, Schechter R, et al. Factors associated with death or hospitalization due to pandemic 2009 influenza A (H1N1) infection in California. JAMA. 2009. 302:1896–1902.
7. Rello J, Rodríguez A, Ibañez P, Socias L, Cebrian J, Marques A, et al. Intensive care adult patients with severe respiratory failure caused by Influenza A (H1N1)v in Spain. Crit Care. 2009. 13:R148.
8. Davies A, Jones D, Bailey M, Beca J, Bellomo R, Blackwell N, et al. Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Extracorporeal Membrane Oxygenation for 2009 Influenza A (H1N1) Acute Respiratory Distress Syndrome. JAMA. 2009. 302:1888–1895.
9. Hancock K, Veguilla V, Lu X, Zhong W, Butler EN, Sun H, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009. 361:1945–1952.
10. Vaillant L, La Ruche G, Tarantola A, Barboza P. epidemic intelligence team at InVS. Epidemiology of fatal cases associated with pandemic H1N1 influenza 2009. Euro Surveill. 2009. 14(33):pii.19309.
11. Cooksley CD, Avritscher EB, Bekele BN, Rolston KV, Geraci JM, Elting LS. Epidemiology and outcomes of serious influenza-related infections in the cancer population. Cancer. 2005. 104:618–628.
12. OECD factbook 2009: economic, environmental and social statistics. 2009. Paris: OECD.
13. Chien YS, Su CP, Tsai HT, Huang AS, Lien CE, Hung MN, et al. Predictors and outcomes of respiratory failure among hospitalized pneumonia patients with 2009 H1N1 influenza in Taiwan. J Infect. 2010. 60:168–174.
14. Zarychanski R, Stuart TL, Kumar A, Doucette S, Elliott L, Kettner J, et al. Correlates of severe disease in patients with 2009 pandemic influenza (H1N1) virus infection. CMAJ. 2010. 182:257–264.
15. Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, deJong MD, et al. Writing Committee of the Second World Health Organization Consultation on Clinical Aspects of Human Infection with Avian Influenza A (H5N1) Virus. Update on avian influenza A (H5N1) virus infection in humans. N Engl J Med. 2008. 358:261–273.
16. Nguyen JT, Hoopes JD, Smee DF, Prichard MN, Driebe EM, Engelthaler DM, et al. Triple combination of oseltamivir, amantadine, and ribavirin displays synergistic activity against multiple influenza virus strains in vitro. Antimicrob Agents Chemother. 2009. 53:4115–4126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download