Abstract
Nocardia farcinia, an aerobic, gram-positive bacilli actinomycetes of the genus Nocardia, is an uncommon pathogen found in humans. The most common Nocardia infection sites are the lung, central nervous system, and skin. Even though hematogenous dissemination can occur, isolation of the organism from blood cultures is very rare. We report a case of Nocardia infection that was isolated on blood cultures. A 59-year-old male with a medical history that includes a liver transplantation 6-years prior due to hepatocellular carcinoma secondary to chronic hepatitis B, developed pneumonia and was transferred to Severance Hospital. At the time of admission, the patient's initial exam showed hypothermia, tachypnea, and hypotension. His chest radiograph showed severe pneumonia and a large abscess on left upper lobe. Under the presumptive diagnosis of bacterial pneumonia or other opportunistic infection, we started broad spectrum antibiotics. However, he developed Nocardia sepsis, rapidly deteriorated, and subsequently died.
Figures and Tables
Figure 1
Initial chest X-ray showed air containing consolidation and abscess at left lung and multiple small nodules at both lungs.
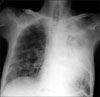
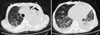
Figure 2
The chest computed tomography revealed necrosis and volume expansion of left upper lobe. Several multiple nodules appeared at both lungs.
References
1. Ambrosioni J, Lew D, Garbino J. Nocardiosis: updated clinical review and experience at a tertiary center. Infection. 2010. 38:89–97.
2. Brown-Elliott BA, Brown JM, Conville PS, Wallace RJ Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin Microbiol Rev. 2006. 19:259–282.
3. Naik S, Mateo-Bibeau R, Shinnar M, Mahal M, Freudenberger R. Successful treatment of Nocardia nova bacteremia and multilobar pneumonia with clarithromycin in a heart transplant patient. Transplant Proc. 2007. 39:1720–1722.
4. Park K, Chong Y, Lee SY. Pulmonary nocardiosis in a renal transplant patient. Yonsei Med J. 1987. 28:157–161.
5. Chang SJ, Lee KN, Sung YK, Lee HS, Uhm WS, Kim TH, et al. Pulmonary nocardiosis in a patient with lupus nephritis. J Korean Rheum Assoc. 2005. 12:47–51.
6. Sim SH, Park HC, Kim CJ, Jeon JH, Kim EC, Oh MD, et al. A case of Nocardia farcinica brain abscess in the patient receiving steroid treatment. Infect Chemother. 2008. 40:301–304.
7. Beaman BL, Beaman L. Nocardia species: host-parasite relationships. Clin Microbiol Rev. 1994. 7:213–264.
8. Kontoyiannis DP, Ruoff K, Hooper DC. Nocardia bacteremia: report of 4 cases and review of the literature. Medicine (Baltimore). 1998. 77:255–267.
9. Roth A, Andrees S, Kroppenstedt RM, Harmsen D, Mauch H. Phylogeny of the genus Nocardia based on reassessed 16S rRNA gene sequences reveals underspeciation and division of strains classified as Nocardia asteroides into three established species and two unnamed taxons. J Clin Microbiol. 2003. 41:851–856.
10. Filice GA. Inhibition of Nocardia asteroides by neutrophils. J Infect Dis. 1985. 151:47–56.
11. Goodfellow M, Williams ST. Ecology of actinomycetes. Annu Rev Microbiol. 1983. 37:189–216.
12. Wallace RJ Jr, Tsukamura M, Brown BA, Brown J, Steingrube VA, Zhang YS, et al. Cefotaxime-resistant Nocardia asteroides strains are isolates of the controversial species Nocardia farcinica. J Clin Microbiol. 1990. 28:2726–2732.
13. Lerner PI. Nocardiosis. Clin Infect Dis. 1996. 22:891–903.
14. Wilson RW, Steingrube VA, Brown BA, Blacklock Z, Jost KC Jr, McNabb A, et al. Recognition of a Nocardia transvalensis complex by resistance to aminoglycosides, including amikacin, and PCR-restriction fragment length polymorphism analysis. J Clin Microbiol. 1997. 35:2235–2242.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download