Abstract
Background
Difficult-to-treat asthma afflicts a small percentage of the asthma population. However, these patients remain refractory to treat, and account for 40% to 50% of the health costs of asthma treatment, incurring significant morbidity. We conducted a multi-center cross-sectional study to characterize difficult-to-treat asthma in Korea.
Methods
Subjects with difficult-to-treat asthma and subjects with controlled asthma were recruited from 5 outpatient clinics of referral hospitals. We reviewed medical records of previous 6 months and obtained patient-reported questionnaires composed of treatment compliance, asthma control, and instruments for stress, anxiety, and depression.
Results
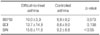
We recruited 21 subjects with difficult-to-treat asthma and 110 subjects with controlled asthma into the study. The subjects with difficult-to-treat asthma were associated with longer treatment periods, more increased health care utilization, more medication (oral corticosteroids, number of medication), and more anxiety disorder compared to those of well-controlled asthmatics. There was no difference in age, gender, history of allergy, serum IgE, blood eosinophil count, or body mass index between the 2 groups.
Figures and Tables
Acknowledgements
This study was supported by the Korean Asthma Study Group, the Korean Academy of Tuberculosis and Respiratory Diseases.
This study was supported by MSD Korea. We authors thank the members of the Korean Asthma Study Group, the Korean Academy of Tuberculosis and Respiratory Diseases: Young June Jeon, Yang Keun Rhee, Young Sil Hwang, Kwan Hyoung Kim, Deok Gyum Kim, Hyung Jung Kim, In Won Park, Jae Jeong Shim, Seoo Taek Uh, Yeon-Mok Oh, Kwang Ha Yoo, Jee Hong Yoo, Kwan Ho Lee, Yong Chul Lee, Kwang Ho In, Seong Yong Lim, Jung Hyun Chang, and Ki Suck Jung.
References
1. Weiss KB, Gergen PJ, Hodgson TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992. 326:862–866.
2. Godard P, Chanez P, Siraudin L, Nicoloyannis N, Duru G. Costs of asthma are correlated with severity: a 1-yr prospective study. Eur Respir J. 2002. 19:61–67.
3. Antonicelli L, Bucca C, Neri M, De Benedetto F, Sabbatani P, Bonifazi F, et al. Asthma severity and medical resource utilisation. Eur Respir J. 2004. 23:723–729.
4. Sullivan SD, Rasouliyan L, Russo PA, Kamath T, Chipps BE. TENOR Study Group. Extent, patterns, and burden of uncontrolled disease in severe or difficult-to-treat asthma. Allergy. 2007. 62:126–133.
5. Miller MK, Lee JH, Miller DP, Wenzel SE. TENOR Study Group. Recent asthma exacerbations: a key predictor of future exacerbations. Respir Med. 2007. 101:481–489.
6. Haselkorn T, Fish JE, Zeiger RS, Szefler SJ, Miller DP, Chipps BE, et al. Consistently very poorly controlled asthma, as defined by the impairment domain of the Expert Panel Report 3 guidelines, increases risk for future severe asthma exacerbations in The Epidemiology and Natural History of Asthma: Outcomes and Treatment Regimens (TENOR) study. J Allergy Clin Immunol. 2009. 124:895–902. e1–e4.
7. O'Byrne PM, Pedersen S, Lamm CJ, Tan WC, Busse WW. START Investigators Group. Severe exacerbations and decline in lung function in asthma. Am J Respir Crit Care Med. 2009. 179:19–24.
8. American Thoracic Society. Proceedings of current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000. 162:2341–2351.
9. European Network for Understanding Mechanisms of Severe Asthma. The ENFUMOSA cross-sectional European multicentre study of the clinical phenotype of chronic severe asthma. Eur Respir J. 2003. 22:470–477.
10. Dolan CM, Fraher KE, Bleecker ER, Borish L, Chipps B, Hayden ML, et al. Design and baseline characteristics of the epidemiology and natural history of asthma: Outcomes and Treatment Regimens (TENOR) study: a large cohort of patients with severe or difficultto-treat asthma. Ann Allergy Asthma Immunol. 2004. 92:32–39.
11. Frank SH, Zyzanski SJ. Stress in the clinical setting: the Brief Encounter Psychosocial Instrument. J Fam Pract. 1988. 26:533–539.
12. Yim JH, Bae JM, Choi SS, Kim SW, Hwang HS, Huh BY. The validity of modified Korean-translated BEPSI (brief encounter psychosocial instrument) as instrument of stress measurement in outpatient clinic. J Korean Acad Fam Med. 1996. 17:42–53.
13. Yook SP, Kim ZS. A clinical study on the Korean version of beck anxiety inventory: comparative study of patient and non-patient. Korean J Clin Psychol. 1997. 16:185–197.
14. Cho Y, Kim J. Confirmatory factor analysis of the Korean version of the beck depression inventory: testing configural and metric invariance across undergraduate and clinical samples. Korean J Clin Psychol. 2002. 21:843–857.
15. Partridge MR, van der Molen T, Myrseth SE, Busse WW. Attitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE study. BMC Pulm Med. 2006. 6:13.
16. Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, et al. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med. 2004. 170:836–844.
17. Chung KF, Godard P, Adelroth E, Ayres J, Barnes N, Barnes P, et al. ERS Task Force on Difficult/Therapy-Resistant Asthma. European Respiratory Society. Difficult/therapy-resistant asthma: the need for an integrated approach to define clinical phenotypes, evaluate risk factors, understand pathophysiology and find novel therapies. Eur Respir J. 1999. 13:1198–1208.
18. Osborne M, Deffebach M. The epidemiology and natural history of asthma: outcomes and treatment regimens (TENOR) study. Ann Allergy Asthma Immunol. 2004. 92:3–4.
19. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009. 180:59–99.
20. Bousquet J, Mantzouranis E, Cruz AA, Ait-Khaled N, Baena-Cagnani C, Bleecker ER. WHO definition of asthma severity, control and exacerbations. A draft for WHO consultation on severe asthma. 2009. 04. 6-7. geneva: WHO headquarters;(personal communication).
21. The Global Initiative for Asthma (GINA) [Internet]. National Heart Lung and Blood Institute, National Institutes of Health (USA), World Health Organization. c2009. cited 2010 Oct 30. [place unknown]: GINA;Available from: http://www.ginasthma.com.
22. Schatz M, Li JT, Sorkness CA. Responsiveness of the asthma control tes (ACT) to changes in specialist ratings of asthma control and FEV1. Am J Respir Crit Care Med. 2004. 169:A319.
23. Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004. 113:59–65.
24. Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006. 117:549–556.
25. Zhou X, Ding FM, Lin JT, Yin KS, Chen P, He QY, et al. Validity of asthma control test in Chinese patients. Chin Med J (Engl). 2007. 120:1037–1041.
26. Lai CK, Kuo SH, de Guia T, Lloyd A, Williams AE, Spencer MD. Asthma control and its direct healthcare costs: findings using a derived Asthma Control Test™ score in eight Asia-Pacific areas. Eur Respir Rev. 2006. 15:24–29.
27. Gaga M, Papageorgiou N, Yiourgioti G, Karydi P, Liapikou A, Bitsakou H, et al. Risk factors and characteristics associated with severe and difficult to treat asthma phenotype: an analysis of the ENFUMOSA group of patients based on the ECRHS questionnaire. Clin Exp Allergy. 2005. 35:954–959.
28. Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol. 2007. 119:405–413.
29. Wenzel SE, Busse WW. National Heart, Lung, and Blood Institute's Severe Asthma Research Program. Severe asthma: lessons from the Severe Asthma Research Program. J Allergy Clin Immunol. 2007. 119:14–21.
30. Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010. 181:315–323.
31. Hartert TV, Speroff T, Togias A, Mitchel EF Jr, Snowden MS, Dittus RS, et al. Risk factors for recurrent asthma hospital visits and death among a population of indigent older adults with asthma. Ann Allergy Asthma Immunol. 2002. 89:467–473.
32. DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000. 160:2101–2107.
33. Ministry of Health and Welfare, Korea. The epidemiological survey of psychiatric illnesses in Korea, 2006. 2007. Seoul: Ministry of Health and Welfare.
34. Scott KM, Von Korff M, Ormel J, Zhang MY, Bruffaerts R, Alonso J, et al. Mental disorders among adults with asthma: results from the World Mental Health Survey. Gen Hosp Psychiatry. 2007. 29:123–133.
35. ten Brinke A, Ouwerkerk ME, Zwinderman AH, Spinhoven P, Bel EH. Psychopathology in patients with severe asthma is associated with increased health care utilization. Am J Respir Crit Care Med. 2001. 163:1093–1096.
36. Campbell DA, Yellowlees PM, McLennan G, Coates JR, Frith PA, Gluyas PA, et al. Psychiatric and medical features of near fatal asthma. Thorax. 1995. 50:254–259.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download