Abstract
Background
D-dimer testing is widely applied as a first step in the diagnostic work-up of pulmonary embolism (PE). Although this is the most sensitive assay for ruling out PE, the prognostic implications of D-dimer testing in patients with normotensive PE are not well known. The aim of this study was to determine if D-dimer testing on admission predicts major adverse cardiac events (MACE) in patients with normotensive PE.
Methods
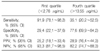
A total of 180 consecutive patients with normotensive PE admitted between January 2003 and June 2009 were included. The group was divided into quartiles on the basis of their D-dimer levels. We compared the frequency of MACE by quartile of D-dimer level and estimated sensitivity, specificity, and predictive values for MACE in the first and fourth quartile.
Results
In the 37 (20.6%) patients with MACEs, the median D-dimer level (7.94 [IQR: 4.03~18.17] µg/mL) was higher than in patients with a benign course (5.29 [IQR: 2.60~11.52] µg/mL, p<0.01). The occurrence of MACEs was increased with increasing D-dimer level (p=0.017). In the first quartile (D-Dimer <2.76 µg/mL) sensitivity, specificity, and positive and negative predictive values for predicting MACEs were, respectively, 91.9%, 29.4%, 25.2%, and 93.3%.
Figures and Tables
Figure 1
D-dimer level in patients with pulmonary embolism with or without major adverse cardiac event (MACE). Data are presented as box-plots of median with 25th and 75th percentiles, whiskers showing points that are 1.5 times the interquartile range below the 25th percentile or above 75th percentile.

Figure 2
Receiver operating characteristic curve of D-dimer for the determination of major adverse cardiac events in normotensive pulmonary embolism.
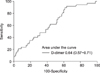
Table 1
Baseline characteristics of major adverse cardiac events (MACE) group and non-MACE group

MACE: major adverse cardiac event; IQR: inter-quartile range; DM: diabetes mellitus; COPD: chronic obstructive pulmonary disease; NYHA: New York Heart Association; SBP: systolic blood pressure; DBP: diastolic blood pressure; CRP: c-reactive protein; BNP: B-type natriuretic peptide.
*Mann-Whitney U test, †Fisher's exact test.
References
1. Goldhaber SZ, Elliott CG. Acute pulmonary embolism: part II: risk stratification, treatment, and prevention. Circulation. 2003. 108:2834–2838.
2. Kreit JW. The impact of right ventricular dysfunction on the prognosis and therapy of normotensive patients with pulmonary embolism. Chest. 2004. 125:1539–1545.
3. Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J, et al. Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med. 2005. 172:1041–1046.
4. Punukollu G, Gowda RM, Vasavada BC, Khan IA. Role of electrocardiography in identifying right ventricular dysfunction in acute pulmonary embolism. Am J Cardiol. 2005. 96:450–452.
5. Logeart D, Lecuyer L, Thabut G, Tabet JY, Tartiere JM, Chavelas C, et al. Biomarker-based strategy for screening right ventricular dysfunction in patients with non-massive pulmonary embolism. Intensive Care Med. 2007. 33:286–292.
6. Schoepf UJ, Kucher N, Kipfmueller F, Quiroz R, Costello P, Goldhaber SZ. Right ventricular enlargement on chest computed tomography: a predictor of early death in acute pulmonary embolism. Circulation. 2004. 110:3276–3280.
7. Ghanima W, Abdelnoor M, Holmen LO, Nielssen BE, Ross S, Sandset PM. D-dimer level is associated with the extent of pulmonary embolism. Thromb Res. 2006. 120:281–288.
8. Konstantinides S, Geibel A, Heusel G, Heinrich F, Kasper W. Heparin plus alteplase compared with heparin alone in patients with submassive pulmonary embolism. N Engl J Med. 2002. 347:1143–1150.
9. Galle C, Papazyan JP, Miron MJ, Slosman D, Bounameaux H, Perrier A. Prediction of pulmonary embolism extent by clinical findings, D-dimer level and deep vein thrombosis shown by ultrasound. Thromb Haemost. 2001. 86:1156–1160.
10. Klok FA, Djurabi RK, Nijkeuter M, Eikenboom HC, Leebeek FW, Kramer MH, et al. High D-dimer level is associated with increased 15-d and 3 months mortality through a more central localization of pulmonary emboli and serious comorbidity. Br J Haematol. 2008. 140:218–222.
11. Blamoun J, Alfakir M, Sedfawy AI, Moammar MQ, Maroules M, Khan MA, et al. The association of D-dimer levels with clinical outcomes in patients presenting with acute pulmonary embolism. Lab Hematol. 2009. 15:4–9.
12. Lobo JL, Zorrilla V, Aizpuru F, Grau E, Jimenez D, Palareti G, et al. D-dimer levels and 15-day outcome in acute pulmonary embolism. Findings from the RIETE registry. J Thromb Haemost. 2009. 7:1795–1801.
13. Grau E, Tenias JM, Soto MJ, Gutierrez MR, Lecumberri R, Perez JL, et al. D-dimer levels correlate with mortality in patients with acute pulmonary embolism: findings from the RIETE registry. Crit Care Med. 2007. 35:1937–1941.
14. Kabbara R, Labarere J, Pernod G, Bosson JL. D-dimer level is not a prognostic biomarker specific of pulmonary embolism. Crit Care Med. 2008. 36:652–653. author reply 653.
15. Bova C, Pesavento R, Marchiori A, Palla A, Enea I, Pengo V, et al. Risk stratification and outcomes in hemodynamically stable patients with acute pulmonary embolism: a prospective, multicentre, cohort study with three months of follow-up. J Thromb Haemost. 2009. 7:938–944.
16. Söhne M, Ten Wolde M, Büller HR. Biomarkers in pulmonary embolism. Curr Opin Cardiol. 2004. 19:558–562.
17. Aujesky D, Roy PM, Guy M, Cornuz J, Sanchez O, Perrier A. Prognostic value of D-dimer in patients with pulmonary embolism. Thromb Haemost. 2006. 96:478–482.
18. Agterof MJ, van Bladel ER, Schutgens RE, Snijder RJ, Tromp EA, Prins MH, et al. Risk stratification of patients with pulmonary embolism based on pulse rate and D-dimer concentration. Thromb Haemost. 2009. 102:683–687.
19. Vuilleumier N, Le Gal G, Verschuren F, Perrier A, Bounameaux H, Turck N, et al. Cardiac biomarkers for risk stratification in non-massive pulmonary embolism: a multicenter prospective study. J Thromb Haemost. 2009. 7:391–398.
20. Kucher N, Printzen G, Goldhaber SZ. Prognostic role of brain natriuretic peptide in acute pulmonary embolism. Circulation. 2003. 107:2545–2547.
21. Kline JA, Zeitouni R, Marchick MR, Hernandez-Nino J, Rose GA. Comparison of 8 biomarkers for prediction of right ventricular hypokinesis 6 months after submassive pulmonary embolism. Am Heart J. 2008. 156:308–314.
22. Vuilleumier N, Righini M, Perrier A, Rosset A, Turck N, Sanchez JC, et al. Correlation between cardiac biomarkers and right ventricular enlargement on chest CT in non massive pulmonary embolism. Thromb Res. 2007. 121:617–624.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download