Abstract
A 55-year old woman with advanced stage non-small cell lung cancer was admitted to hospital for the management of severe chest pain, which measured 7 out of 10 on a numerical rating scale (NRS). Despite palliative radiation and the application of multiple epidural blocks, she continued to experience severe cancer pain. We gradually increased the dose of transdermal fentanyl patches from 500 µg/hr to 3,650 µg/hr, for 3 months without any significant side effects. Concomitantly, adjuvant therapy with antidepressants and anticonvulsants were added, decreasing the patient's pain to NRS 3~4 down from 7. After being transferred to a hospice clinic, her chest pain was well-controlled below NRS 4 by means of strong opioid medications, including the highest dose of transdermal fentanyl 4,050 µg/hr for more than 16 months.
Cancer pain, which occurs in three quarters of patients with advanced malignancy, is a common symptom that must be resolved1. Although many guidelines about the management of cancer pain have been created, finding a satisfactory pain control without complications of strong opioid analgesics is very hard. We herein report on a patient who used very high-dose fentanyl patches without any significant side effects.
A 55-year-old woman with advanced non-small cell lung cancer (NSCLC) presented with complaints of her right chest and flank pains. Since her initial diagnosis of stage IV NSCLC with malignant pleural effusion 18 months earlier, she had undergone multiple chemotherapies (four cycles of paclitaxel and carboplatin as the 1st line drugs, followed by gefitinib medication for 8 months). However, her chest and flank pains were worse probably due to aggravated pleural metastasis and loculated effusion (Figure 1). She complained of severe, constant, sharp chest and flank pains and rated her background pain intensity at 7 out of 10 on numerical rating scale (numerical rating scale [NRS]: 0, no pain; 10, worst possible pain), with intermittent breakthrough exacerbation. In order to relieve her pains, many medications had been gradually increased from the baseline dosage (fentanyl patches 500 µg/hr, oxycodone 180 mg/day, tramadol/acetaminophen 150/1,500 mg/day, gabapentin 2,400 mg/day, alprazolam 0.5 mg/day. At the same time, 4 times of epidural nerve blockage and palliative radiation (3,000 Gy) were applied. Furthermore, additional palliative chemotherapy with two cycles of pemetrexed and weekly gemcitabine monotherapy were applied. During the hospitalization her pains were gradually decreased by the mentioned-above treatments from NRS 7/10 to 3/10, in spite of her mild somnolent depressed mood and tolerable constipation.
Several weeks later, her pains became worse and reached to NRS 9/10 and the increased tumor size was shown on the chest computed tomography imaging. She did not want further interventions, such as chemotherapy, radiotherapy, or nerve blockage, and she just wanted to increase the opioid analgecis as long as she could stand the side effects. We gradually increased fentanly patches from 500 µg/hr to 1,575 µg/hr for the first month, to 2,750 µg/hr for the second month, and finally to 3,650 µg/hr for the third month. In other words, this treatment was given for 3 months (Figure 2). By addition of other analgesics and anticonvulsant-including oxycodone 960 mg/day and gabapentin 270 mg/day, she could discharge with improved chest pain (NRS 4/10). Because total number of patches on her body was more than thirty six of transdermal fentanyl 100 µg/hr, they were placed over her chest, back, abdomen, and lower extremities (Figure 3).
Three months after discharging from our hospital, despite the current total doses of fentanyl patches were 4,050 µg/hr, she was carrying on her end of life satisfactorily with only mild somlolence and constipation. Finally, she had been doing daily activities for more than 16 months of her last lifetime.
Pain is the frequent symptom associated with malignancy, and lung cancer is one of the commonest cancers to cause pain. Pain occurs in about three quarters of patients with advanced malignancy, and this is one of the symptoms patients fear the most1. Nociceptive pain was the major pathophysiological subtype in lung cancer pains, but neuropathic pain accounted for 30% of cases2.
The most widely accepted guidelines for the treatment of cancer pain were developed by the World Health Organization (WHO)3 and the National Comprehensive Cancer Network (NCCN) Adult Cancer Pain Panel1. Opioid analgesics have no ceiling effect, and the dosage could be increased according to the pain intensity. For chronic cancer pain control, oral opioid administration is the easiest and safest method. However, the high dose opioids can cause gastrointestinal troubles, such as severe constipation and gastric ulcer. On the other hand, transdermal fentanyl patches have less gastrointestinal toxicity due to bypass the first-pass metabolism. We prescribed matrix patch (Durogesic® D-trans; Janssen Cilag, Beerse, Belgium) for this patient. This patch is the second generation with matrix design in which fentanyl is dissolved in a semisolid formation of a polyacrylate adhesive4. There are several published data about maximal dose of fentanyl patches5-8. Most patients could use the patch in a range of 1,000 to 3,000 µg/hr, but it was hard to increase higher dose because of severe side effects. However, our case reported patient could increase to the very high dose fentanyl patch (4,050 µg/hr) with other opioid and non-opioid analgesics according to her subjective pain scale for more than seven months. Fortunately, the patient could be carrying her daily activities without severe opioids complications for the last 16 months of her life. By using WHO ladder, medical treatment has been found effective in relieving pain in approximately 90% of patients with cancer and in over 75% of cancer patients who are terminally ill4.
In summary, this case illustrates that cancer pain can be successfully controlled by appropriate opioid analgesics with tolerable side effects. And we think this reported dose of transdermal fentanly patch is the highest dose in the published literatures until present.
Figures and Tables
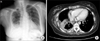 | Figure 1(A) Chest X-ray shows haziness and pleural effusion in right lower lung field. (B) Chest CT scan shows an increased amount of multiloculated pleural effusion along right pleural space with nodular pleural thickening and enhancement, considered as aggravated pleural metastasis. |
Acknowledgements
The authors are grateful to the medical team of Mokpo Christian Hospital, for the dedicated patient care.
References
1. NCCN clinical practice guidelines in oncology: adult cancer pain V.1.2009 [Internet]. National Comprehensive Cancer Network. 2009. cited 2010 Feb 16. Fort Washington: National Comprehensive Cancer Network;Available from: http://www.nccn.org/professionals/physician_gls/PDF/pain.pdf.
2. Potter J, Higginson IJ. Pain experienced by lung cancer patients: a review of prevalence, causes and pathophysiology. Lung Cancer. 2004. 43:247–257.
3. Stjernswärd J, Colleau SM, Ventafridda V. The World Health Organization Cancer Pain and Palliative Care Program: past, present, and future. J Pain Symptom Manage. 1996. 12:65–72.
4. Kress HG, Von der Laage D, Hoerauf KH, Nolte T, Heiskanen T, Petersen R, et al. A randomized, open, parallel group, multicenter trial to investigate analgesic efficacy and safety of a new transdermal fentanyl patch compared to standard opioid treatment in cancer pain. J Pain Symptom Manage. 2008. 36:268–279.
5. Menahem S, Shvartzman P. High-dose fentanyl patch for cancer pain. J Am Board Fam Pract. 2004. 17:388–390.
6. Radbruch L, Elsner F. Clinical experience with transdermal fentanyl for the treatment of cancer pain in Germany. Keio J Med. 2004. 53:23–29.
7. Seamans DP, Wong GY, Wilson JL. Interventional pain therapy for intractable abdominal cancer pain. J Clin Oncol. 2000. 18:1598–1600.
8. Ryu JS, Kim SH, Um UH, Cho JH, Kwak SM, Lee HL. Successful treatment with high dose transdermal fentanyl patch for severe cancer pain in a patient with lung cancer. Tuberc Respir Dis. 2007. 62:140–143.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download