Abstract
Erlotinib (Tarceva®) has been considered to be a new, promising oral chemotherapy agent for local advanced or metastatic non-small cell lung cancer (NSCLC). Erlotinib is regarded as relatively safe, but interstitial lung disease (ILD) related to erlotinib has been reported on an infrequent basis in Asia. We report an histologically confirmed case of recurrent erlotinib-induced ILD. Although, the patient was highly responsive to the first erlotinib treatment, the therapy was discontinued due to erlotinib-induced ILD. After intravenous high dose methylpredinisolone treatment, ILD was improved rapidly by radiologic studies, but the particular lung cancer re-emerged. We restarted the patient erlotinib on low-dose oral methylpredinisolone, resulting in a recurrence of erlotinib-induced ILD. Our case suggests that re-administration of erlotinib should be performed on a limited basis in patients that have developed ILD on previous use, even if a therapeutic effect can be estimated.
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors are a new class of drug that inhibits the downstream signaling pathways for cell growth. The overall response rate with erlotinib 150 mg per day was 8.9% in the pivotal BR.21 and 8.3% in the Multicenter, Open-label and Phase 3b Trial respectively1,2.
Erlotinib-induced side effects such as diarrhea, mild to moderate rash, less often keratoconjunctivitis and interstitial lung disease (ILD) have been observed1,3. Since gefitinib was approved, gefitinib-induced ILD has been reported up to 10%4 especially on Asian heritage. Incidence of erlotinib-induced ILD has been estimated at approximately 0.8~1%1,2,5 less than gefitinib. However considering the short experience period of erlotinib and fatality of pulmonary severe adverse effect, it demands great caution for prescription by assessing risk factors of ILD development.
Histopathology of erlotinib-induced ILD that could be a confirmative diagnostic clue was reported on several autopsy cases and there was no biopsy specimen of live patients showing diffuse alveolar patterns that would be thought as common pattern of erlotinib-induced ILD except one case of BOOP pattern6-9. We report the case of a patient who developed recurrent erlotinib-induced ILD. To our knowledge, this is the first case report of histopatholgically confirmed ILD following erlotinib therapy in a live patient with non-small cell lung cancer (NSCLC) in Korea.
In September 2007, a 60-year-old man with stage IV NSCLC was admitted in our hospital with dyspnea. The patient had 9-days of progressive dyspnea and exertional dyspnea but no complaints of other pulmonary symptoms. He had a history of 60 pack years of tobacco use. Stage IV left upper lobe (LUL) adenocarcinoma was diagnosed eighteen months ago. He had received three successive regimes of chemotherapy (docetaxel plus cisplatin between March and September 2006, gemcitabine between February and March 2007, pemetrexed between May and June 2007), but size of LUL mass increased and disease progression was documented (Figure 1A). In July 2007 therapy with erlotinib 150 mg per day was initiated. Nine days after initiation of erlotinib treatment, the patient developed dyspnea and exertional dyspnea. Computed tomography (CT) scan of the chest showed response of the primary tumor, but revealed newly appearing extensive bilateral ground-glass infiltrates consistent with pneumonitis (Figure 1B). On suspecting ILD, erlotinib therapy was discontinued and intravenous methylpredinisolone (250 mg for 5 days) was started. His symptom was improved immediately and discharged with 8mg of oral methylpredinisolone after two weeks of admission.
On 28 days after discharge, radiologic findings of ILD were definitely improved but disease progression was documented on CT scan (Figure 1C). The patient and his family wished to have chemotherapy again. Although ILD had been developed during previous erlotinib therapy, erlotinib therapy had been apparently effective to the patient and there was no other choice of treatment. Since the patient and his family wished to restart erlotinib and understood the risk of recurrent ILD, erlotinib was initiated again. However, the patient was admitted with dyspnea and dry cough following 24 days of erlotinib re-therapy. On admission, his temperature was 36.6℃, blood pressure was 120/60 mmHg, pulse was 86 beats per minute. He was tachypnoeic with 30 breaths per minute. Cardiovascular evaluation was normal with no evidence of significant jugular venous distension or peripheral edema. Chest examination revealed bilateral inspiratory crackles. The laboratory findings were as follows: white blood cells, 8,100/L (91% neutrophils); C-reactive protein, 14.85 mg/dL (reference range, 0.00~0.30 mg/dL); PaO2 63 mmHg and PaCO2 25 mmHg. Chest CT showed recurrently scattered ground grass infiltrates in both lungs implying recurrent erlotinib-induced ILD (Figure 1D). Erlotinib was discontinued and intravenous methylpredinisolone (250 mg) was started. The next day, he developed high fever and C-reactive protein level further elevated (24.16 mg/dL). Transbronchial lung biopsies (TBLB) and bronchoalveolar lavage (BAL) were performed to exclude other causes. There were no neutrophils and eosinophils in BAL fluid. All cultures and stains for infectious etiologies including common bacteria and fungi were negative. Histopathology of high magnification showed mild interstitial lymphocytic infiltration with fibrosis and intra-alveolar fibrous (Figure 2). After steroid treatment, his symptoms and radiologic findings immediately improved but metastatic lung mass progressively increased on Chest X-ray. After one month of admission, the patient gradually deteriorated and hopeless discharged.
Since erlotinib was approved, ILD was exhibited in 0.8% to 1% in oriental patients1,2. Cough and dyspnea are presented as initial symptom of ILD at 6 days to 9 months after initiation of treatment and it shows more variable onset time than geftinib1; gefitinib-induced ILD occurred with median time to symptom development being 24 to 31 days in Japan and 42 days in United States8,10,11. Diagnosis of erlotinib-induced ILD is mainly dependent on symptoms following erlotinib medication and radiologic finding that is shown as a newly developed ground grass opacitiy2,9. Possible predisposing risk factors such as prior chemotherapy or radiotherapy are mentioned as obstacles to establish the real causes3,9,12.
Our case has recurrently undergone two erlotinib induced ILD episodes. In the first occurrence, dyspnea developed after 9 days of erlotinib treatment and second occurrence developed following 24 days of erlotinib re-therapy. Since discharge after first admission, the patient was on low dose oral steroid which might explain the delayed onset of ILD. Corticosteroid therapy for both episodes effectively relieved the symptoms and made improvement in radiologic findings. It shows a clinical similarity to recurrent gefitinib-induced ILD10,11 which is reported that pathogenesis of EGFR-induced ILD is immunological activation rather than direct drug cytotoxicity because of good response for corticosteroid, shortening of second attack period and more severe ILD recurrence than the first occurrence. Even though our case showed acute interstitial pneumonia (AIP) pattern with extensive bilateral ground-glass appearance on chest CT that was thought as a poor prognosis group3, obviously our patient was a good responder to erlotinib based on Chest CT finding that showed dramatic decrease of metastatic lung lesions. He had favorable characteristics such as oriental species, adenocarcinoma and predictive risk factors for ILD in male sex, smoking history1-3.
There are some cases reports of histopathology based on autopsy which revealed diffuse alveolar damage6,9, but these finding were exclusively presented on acute respiratory distress syndrome (ARDS) and end stage lung disease. In this case transbronchial lung biopsy was done relatively early stage and lung tissue of live patient was obtained. Histopathology of our patient is suggestive of organizing stage of an AIP or ARDS, which implies that pathogenesis of erlotinib-induced ILD will be similar with AIP, ARDS; dysfunction on repair systems, suggested that EGFR-TKIs will interfere with EGFR-dependent epithelial proliferation6.
Erlotinib is a palliative treatment modality that should improve survival period and not disturb to keep quality of life to a maximum by reducing drug induced side effects. Erlotinib-induced ILD shows variable prognosis from complete recovery to death. Although several prognostic factors have been proposed to predict ILD severity, rapid diagnosis with clinical clues, chest CT and lung biopsy is the most important thing to yield a good prognosis.
It is uncertain whether low dose steroid with erlotinib would delay onset of ILD development for high risk patients as like our case and no data are available to suggest erlotinib with any dose steroid as preventative regimens. Through more clinical trials, steroid effect could be assessed for high risk patients of ILD but effective to erlotinib. In conclusion, re-administration of erlotinib should be careful in patients, developed ILD following its use, even if a therapeutic effect could be estimated.
Figures and Tables
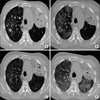 | Figure 1Low dose chest computed tomography (CT) before (A) and after (B) the first interstitial lung disease (ILD) episode. Multiple metastatic lesions on (A) are markedly decreased on (B) but diffuse GGO newly appeared. (C) After high dose methylpredinisolone IV treatment, the extent of ILD is decreased on following low dose chest CT. Second episode (D) represented more severe diffuse GGO on both lung fields. |
References
1. Johnson JR, Cohen M, Sridhara R, Chen Y, Williams GM, Duan J, et al. Approval summary for erlotinib for treatment of patients with locally advanced or metastatic non-small cell lung cancer after failure of at least one prior chemotherapy regimen. Clin Cancer Res. 2005. 11:6414–6421.
2. Spigel DR, Lin M, O'Neill V, Hainsworth JD. Final survival and safety results from a multicenter, open-label, phase 3b trial of erlotinib in patients with advanced nonsmall cell lung cancer. Cancer. 2008. 112:2749–2755.
3. Kato T, Nishio K. Clinical aspects of epidermal growth factor receptor inhibitors: benefit and risk. Respirology. 2006. 11:693–698.
4. Niho S, Kubota K, Goto K, Yoh K, Ohmatsu H, Kakinuma R, et al. First-line single agent treatment with gefitinib in patients with advanced non-small-cell lung cancer: a phase II study. J Clin Oncol. 2006. 24:64–69.
5. Fukui T, Mitsudomi T. Mutations in the epidermal growth factor receptor gene and effects of EGFR-tyrosine kinase inhibitors on lung cancers. Gen Thorac Cardiovasc Surg. 2008. 56:97–103.
6. Liu V, White DA, Zakowski MF, Travis W, Kris MG, Ginsberg MS, et al. Pulmonary toxicity associated with erlotinib. Chest. 2007. 132:1042–1044.
7. Yoneda KY, Shelton DK, Beckett LA, Gandara DR. Independent review of interstitial lung disease associated with death in TRIBUTE (paclitaxel and carboplatin with or without concurrent erlotinib) in advanced non-small cell lung cancer. J Thorac Oncol. 2007. 2:537–543.
8. Cohen MH, Williams GA, Sridhara R, Chen G, Pazdur R. FDA drug approval summary: gefitinib (ZD1839) (Iressa) tablets. Oncologist. 2003. 8:303–306.
9. Makris D, Scherpereel A, Copin MC, Colin G, Brun L, Lafitte JJ, et al. Fatal interstitial lung disease associated with oral erlotinib therapy for lung cancer. BMC Cancer. 2007. 7:150.
10. Kitajima H, Takahashi H, Harada K, Kanai A, Inomata S, Taniguchi H, et al. Gefitinib-induced interstitial lung disease showing improvement after cessation: disassociation of serum markers. Respirology. 2006. 11:217–220.
11. Suzuki M, Asahina H, Konishi J, Yamazaki K, Nishimura M. Recurrent gefitinib-induced interstitial lung disease. Intern Med. 2008. 47:533–536.
12. Niho S, Goto K, Yoh K, Kim YH, Ohmatsu H, Kubota K, et al. Interstitial shadow on chest CT is associated with the onset of interstitial lung disease caused by chemotherapeutic drugs. Jpn J Clin Oncol. 2006. 36:269–273.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download