Abstract
Background
Several large outbreaks have demonstrated the threat of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) in close-contact environments, such as occurs during training and quartering of military recruits training. In South Korea, which is a hospital or healthcare-associated MRSA prevalent area, military service is compulsory for all healthy young men. We surveyed and determined the extent of CA-MRSA colonization in the upper respiratory tracts of Korean military recruits.
Methods
The Korean military recruits who were enrolled in a military training facility from November 2004 to March 2005 were eligible for this study. Sputum or nasopharyngeal swap was obtained from randomly selected subjects who displayed upper respiratory tract symptoms.
Results
Of the 181 participants, 32 participants (17.7%) were colonized with S. aureus, and 12 participants (6.6%) were colonized with MRSA. Among the cases that were colonized with S. aureus, 37.5% (12/32) were colonized with MRSA. Antimicrobial susceptibility testing showed resistant patterns that were suggestive of the CA-MRSA strains for all of the MRSA isolates.
Conclusion
This study of Korean military recruits found a great deal of showed MRSA colonization in them, and the antimicrobial resistant profile that was suggestive of a CA-MRSA strain. Further efforts to prevent the spread of MRSA infections and careful monitoring for CA-MRSA outbreaks are warranted, especially in a high risk group such as military recruits.
Recent reports indicate that the prevalence of community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) infections is increasing, but even more concerning are the recent, numerous CA-MRSA outbreaks that have involved groups of young, healthy individuals who had no direct ties to health care facilities and they had none of the typical risk factors for infection1,2. These outbreaks occurred in a well-defined population of young, healthy, military trainees who experienced relatively uniform exposures in their environment2,3. The control measures that were implemented during the outbreak may have helped to reduce the transmission of MRSA between trainees living in who had close contact2. It may be that military training itself is a risk factor due to the crowding, inadequate hygiene, and possible skin trauma, and all these factors which may contribute to S. aureus colonization and thus infection4-6. In South Korea, which is a hospital or healthcare-associated MRSA prevalent area, military service is compulsory for all healthy young men. However, there are no data available regarding CA-MRSA colonization or infection in Korean military personnel.
Periodic surveys for upper respiratory tract infections in military recruits in the South Korean army have been performed since 2004. Here, we assessed the prevalence of CA-MRSA colonization and the anti-microbialial susceptibility patterns.
Korean military recruits were enrolled for this study between November 2004 and March 2005 at a military training facility. Upper respiratory tract samples such as sputum and nasopharyngeal swaps were obtained from randomly selected patients who displayed with upper respiratory tract symptoms such as rhinorrhea, cough and sputum. Informed consents were also obtained from all the subjects of this study. Those patients with chronic diseases, those using prophylactic antibiotics, those who were admitted at a clinic or hospital and females were not included in the study.
The respiratory culture specimens were transported to the Armed Forces Medical Research Institute for microbiological testing. Identification and susceptibility testing of the S. aureus isolates were performed by using an automated broth microdilution method (Vitek II; bio-Mérieux, Hazelwood, MO, USA). The breakpoints used for the in vitro susceptibility testing of the S. aureus isolates were those defined by the Clinical and Laboratory Standards Institute (CLSI).
A total of 181 subjects were included in study. Their median age was 20 years (range, 19~23). All the participants arrived directly from the military training sites. Of the 181 participants, 32 participants (17.7%) were colonized with S. aureus, and 12 participants (6.6%) were colonized with MRSA. Among the cases that were colonized with S. aureus, 37.5% (12/32) were colonized with MRSA.
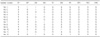
Antimicrobial susceptibility testing indicated that the resistant patterns that were suggestive of CA-MRSA strains for all of the MRSA isolates (Table 1)7. All the isolates were resistant to oxacillin, penicillin, and cephalothin, but they were uniformly susceptible to trimethoprim-sulfamathoxazole, vancomycin, and teicoplanin (Table 1).
To the best of our knowledge, this is the first study to report on the colonization of CA-MRSA in military recruits in the South Korean Army where the prevalence of MRSA prevalence in hospitals is high and where military service is compulsory for all healthy young men. Overall, this investigation demonstrated that the MRSA colonization rate in the upper respiratory tract of Korean military recruits was relatively high, and antimicrobial susceptibility testing indicated that the resistant patterns that were suggestive of CA-MRSA strains. In order to determine the prevalence of MRSA colonization, swab samples were usually obtained from the subjects' nares for the S. aureus cultures. However, we also used collateral data from the periodic survey for respiratory tract infections in military recruits and thus, our results may not reflect the correct MRSA colonization rate. Nevertheless, it was noted that 38% of the S. aureus isolates were CA-MRSA. The prevalence of CA-MRSA colonization in our study was 6.6%. This finding is similar to that of a recent meta-analysis that analyzed the prevalence of CA-MRSA prevalence in Western countries8. Kim et al. reported that less than 5% of the nasal S. aureus isolates in the community were methicillinethicillin-resistant9. Compared with this report, our data (6.6%) revealed a relatively high colonization rate.
The MRSA isolates in this study had a characteristic CA-MRSA antimicrobial susceptibility profile that was different from our prevailing hospital-associated MRSA strain7,10. Our predominant hospital-associated MRSA strain is resistant to all the β-lactam agents, fluoroquinolones, erythromycin, and clindamycin10. We did not determine the molecular profile of the isolates in this study.
A prospective, observational study of soldiers during training found that, colonization with CA-MRSA was associated with a significant risk of soft-tissue infection4. Until now, there have been no reports of CA-MRSA outbreaks in Korean military recruits. However, our data showed a high CA-MRSA colonization rate, which raises concern about the possibility ofle CA-MRSA outbreaks in military recruits.
MRSA is spread by direct contact, most often through the hands of an infected or colonized person. Some of the recent CA-MRSA outbreaks have also involved comparable close-contact environments1. The spread of CA-MRSA has also been associated with prolonged physical contact between sports participants. Activities such as hand-to-hand combat training, life-saving, and team skill-building exercises involve similar physical contact between recruits. Maintaining good hygiene and avoiding contact with open skin lesions are the primary means to prevent the spread of MRSA infections1-3. The deficiencies of hygiene noted in some recruits combined with an increasing prevalence of CA-MRSA were important factors contributing to the spread of microbes. Targeting people's education, hygiene, and personal behaviors may be the key to reducing the spread of MRSA among groups of people who are in those with close physical contact1,2.
The limitations of this study include the small sample size and the unique population. As a result, it may not be possible to generalize our findings to other populations. Large scale surveillance for determining the extent of CA-MRSA colonization in Korean military recruits is certainly warranted. In addition, careful monitoring for a CA-MRSA outbreak is also needed. Routinely submitting the incised drained abscess fluid specimens for culture should be encouraged because it could not only affect the clinical management, but this may also help to define the local resistance patterns4,11.
In conclusion, this study has demonstrated that Korean military recruits display a deal of MRSA colonization, and the an antimicrobial resistant profile was suggestive of a CA-MRSA strain. Further efforts to prevent the spread of MRSA infections and careful monitoring for a CA-MRSA outbreak are warranted, especially in a risk group such as military recruits.
Figures and Tables
References
1. Weber JT. Community-associated methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2005. 41:Suppl 4. S269–S272.
2. Campbell KM, Vaughn AF, Russell KL, Smith B, Jimenez DL, Barrozo CP, et al. Risk factors for community-associated methicillin-resistant Staphylococcus aureus infections in an outbreak of disease among military trainees in San Diego, California, in 2002. J Clin Microbiol. 2004. 42:4050–4053.
3. Zinderman CE, Conner B, Malakooti MA, LaMar JE, Armstrong A, Bohnker BK. Community-acquired methicillin-resistant Staphylococcus aureus among military recruits. Emerg Infect Dis. 2004. 10:941–944.
4. Ellis MW, Hospenthal DR, Dooley DP, Gray PJ, Murray CK. Natural history of community-acquired methicillin-resistant Staphylococcus aureus colonization and infection in soldiers. Clin Infect Dis. 2004. 39:971–979.
5. Cookson BD. Methicillin-resistant Staphylococcus aureus in the community: new battlefronts, or are the battles lost? Infect Control Hosp Epidemiol. 2000. 21:398–403.
6. Martinez-Lopez LE, Friedl KE, Moore RJ, Kramer TR. A longitudinal study of infections and injuries of Ranger students. Mil Med. 1993. 158:433–437.
7. Naimi TS, LeDell KH, Como-Sabetti K, Borchardt SM, Boxrud DJ, Etienne J, et al. Comparison of community- and health care-associated methicillin-resistant Staphylococcus aureus infection. JAMA. 2003. 290:2976–2984.
8. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003. 36:131. 139.
9. Kim HB, Shin DH, Park KU, Oh MD, Kim EC, Choe KW. The methicillin-resistance rate of Staphylococcus aureus isolatd from anterior nares of healthy adults in the community. Korean J Infect Dis. 1998. 30:527–531.
10. Kim HB, Jang HC, Nam HJ, Lee YS, Kim BS, Park WB, et al. In vitro activities of 28 antimicrobial agents against Staphylococcus aureus isolates from tertiary-care hospitals in Korea: a nationwide survey. Antimicrob Agents Chemother. 2004. 48:1124–1127.
11. Stevens DL. Community-acquired Staphylococcus aureus infections: increasing virulence and emerging methicillin resistance in the new millennium. Curr Opin Infect Dis. 2003. 16:189. 191.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download