Abstract
Background
Pulmonary tuberculosis (TB) is still common disease among the elderly patients in Korea where the overall incidence of TB is decreasing. Adverse drug reactions (ADR) associated with anti-TB drugs occurs frequently. Especially the aged tends to have more frequent ADRs than younger ones. These ADRs can cause significant morbidity, compromise therapeutic effects of drugs and even induce drug resistance. Therefore we evaluated the effect of ADRs on the first-line anti-TB drugs in elderly patients with active pulmonary TB.
Methods
We retrospectively reviewed the charts and radiological findings of the patients with 65 and older who were bacteriologically confirmed as active TB and treated with standard anti-TB drugs for at least 6 months. Major ADR was defined with temporary or continuous stop of any first-line drugs intake.
Results
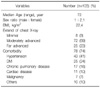
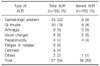
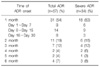
An ADR was noted in 54% of all patients. The incidence of major ADR was 32% in all elderly patients. Dermatologic ADR (9%) was the most common among the major ADRs. GI trouble (8%), arthralgia (6%), visual change (6%), hepatotoxicity (4%), and fever (1%) were also noted. The drugs responsible for major ADR were ethambutol (62%), pyrazinamide (35%), rifampin (18%) and isoniazid (9%). Major ADRs were associated with higher ESR level at the initiation of anti-TB drugs.
Figures and Tables
References
1. Ministry of Health & Welfare. Korean National Tuberculosis Association. Report on the 7th tuberculosis prevalence survey in Korea. 1996. Seoul: Korean National Tuberculosis Association.
2. Korea Center for Disease Control and Prevention. Korean Institute of Tuberculosis. Annual report on the notified tuberculosis patients in Korea: based on Korean Tuberculosis Surveillance System, 2006. 2007. Seoul: Korean Institute of Tuberculosis.
3. Stead WW, Dutt AK. Tuberculosis in elderly persons. Annu Rev Med. 1991. 42:267–276.
4. Dutt AK, Stead WW. Tuberculosis in the elderly. Med Clin North Am. 1993. 77:1353–1368.
5. Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003. 167:1472–1477.
6. Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996. 9:2026–2030.
7. Counsell SR, Tan JS, Dittus RS. Unsuspected pulmonary tuberculosis in a community teaching hospital. Arch Intern Med. 1989. 149:1274–1278.
8. National Tuberculosis and Respiratory Disease Association. Diagnostic standards and classification of tuberculosis. 1969. 12th ed. New York: National Tuberculosis and Respiratory Disease Association.
9. Kim SH, Lee BH, Lee KD, Park JS, Kim YS, Jee YK, et al. The prevalence of adverse drug reactions to a short course anti-tuberculosis regimen. Korean J Med. 2007. 73:496–502.
10. Lee JH, Han DH, Song JW, Chung HS. Diagnostic and therapeutic problems of pulmonary tuberculosis in elderly patients. J Korean Med Sci. 2005. 20:784–789.
11. Kang YJ, Lim SY, Shin JW, Choi JS, Yoo JH, Park IW, et al. Follow-up study of 6-month short course chemotherapy for pulmonary tuberculosis with 2SKHRZ/4HRZ. Tuberc Respir Dis. 1996. 43:852–861.
12. Teale C, Goldman JM, Pearson SB. The association of age with the presentation and outcome of tuberculosis: a five-year survey. Age Ageing. 1993. 22:289–293.
13. World Health Organization. WHO/CDS/TB 2003. 313. Treatment of tuberculosis: guidelines for national programs. 2003. Geneva: World Health Organization.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download