Abstract
Background
Solitary pulmonary nodules (SPN) are encountered incidentally in 0.2% of patients who undergo chest X-ray or chest CT. Although SPN has malignant potential, it cannot be treated surgically by biopsy in all patients. The first stage is to determine if patients with SPN require periodic observation and biopsy or resection. An important early step in the management of patients with SPN is to estimate the clinical pretest probability of a malignancy. In every patient with SPN, it is recommended that clinicians estimate the pretest probability of a malignancy either qualitatively using clinical judgment or quantitatively using a validated model. This study examined whether Bayesian analysis or multiple logistic regression analysis is more predictive of the probability of a malignancy in SPN.
Methods
From January 2005 to December 2008, this study enrolled 63 participants with SPN at the Kangnam Sacred Hospital. The accuracy of Bayesian analysis and Bayesian analysis with a FDG-PET scan, and Multiple logistic regression analysis was compared retrospectively. The accurate probability of a malignancy in a patient was compared by taking the chest CT and pathology of SPN patients with <30 mm at CXR incidentally.
Results
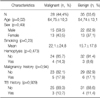
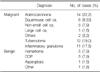
From those participated in study, 27 people (42.9%) were classified as having a malignancy, and 36 people were benign. The result of the malignant estimation by Bayesian analysis was 0.779 (95% confidence interval [CI], 0.657 to 0.874). Using Multiple logistic regression analysis, the result was 0.684 (95% CI, 0.555 to 0.796). This suggests that Bayesian analysis provides a more accurate examination than multiple logistic regression analysis.
Figures and Tables
Figure 1
ROC curves analysis to compare Bayesian analysis, and MLRA. MLRA: multiple logistic regression analysis.
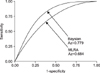
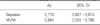
Figure 3
Interactive dot diagram of MLRA analysis. MLRA: multiple logistic regression analysis; Sens: sensitivity; Spec: specificity.

References
1. Tuddenham WJ. Glossary of terms for thoracic radiology: recommendations of the nomenclature committee of the fleischner society. AJR Am J Roentgenol. 1984. 143:509–517.
2. Swensen SJ, Morin RL, Schueler BA, Brown LR, Cortese DA, Pairolero PC, et al. Solitary pulmonary nodule: CT evaluation of enhancement with iodinated contrast material--a preliminary report. Radiology. 1992. 182:343–347.
3. Leef JL 3rd, Klein JS. The solitary pulmonary nodule. Radiol Clin North Am. 2002. 40:123–143.
4. Kim JY, Kim SK, Jang SH, Kim BI, Hong SP, Chang J, et al. Clinical observations of the solitary pulmonary nodules. Tuberc Respir Dis. 1989. 36:320–327.
5. Gweon S, Cho YG, Lee WS, Jung TH. Clinical observation on solitary pulmonary nodules. Tuberc Respir Dis. 1989. 36:63–67.
6. Shin KC, Chung JH, Lee KH, Kim CH, Park JY, Jung TH, et al. Estimating the likelihood of malignacy in solitary pulmonary nodues by Bayesian approach. Tuberc Respir Dis. 1999. 47:498–506.
7. Midthun DE, Swensen SJ, Jett JR. Approach to the solitary pulmonary nodule. Mayo Clin Proc. 1993. 68:378–385.
8. Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997. 111:1710–1717.
9. Gould MK, Fletcher J, Iannettoni MD, Lynch WR, Midthun DE, Naidich DP, et al. American College of Chest Physicians. Evaluation of patients with pulmonary nodules: when is it lung cancer? ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007. 132:108S–130S.
10. Gurney JW. Determining the likelihood of malignancy in solitary pulmonary nodules with Bayesian analysis. Part I. Theory. Radiology. 1993. 186:405–413.
11. Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch Intern Med. 1997. 157:849–855.
12. Nakamura K, Yoshida H, Engelmann R, MacMahon H, Katsuragawa S, Ishida T, et al. Computerized analysis of the likelihood of malignancy in solitary pulmonary nodules with use of artificial neural networks. Radiology. 2000. 214:823–830.
13. Oh YW, Park SY, Kang EY, Park JS, Lee KY, Kim HI, et al. Estimation of the probability of malignancy in solitary pulmonary nodules: comparative study of conventional interpretation method and Bayesian analysis. J Korean Radiol Soc. 1998. 38:67–74.
14. Gurney JW, Swensen SJ. Solitary pulmonary nodules: determining the likelihood of malignancy with neural network analysis. Radiology. 1995. 196:823–829.
15. Swensen SJ, Silverstein MD, Edell ES, Trastek VF, Aughenbaugh GL, Ilstrup DM, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999. 74:319–329.
16. Liptay MJ. Solitary pulmonary nodule: treatment options. Chest. 1999. 116:517S–518S.
17. Good CA, Wilson TW. The solitary circumscribed pulmonary nodule; study of seven hundred five cases encountered roentgenologically in a period of three and one-half years. J Am Med Assoc. 1958. 166:210–215.
18. Yankelevitz DF, Henschke CI. Does 2-year stability imply that pulmonary nodules are benign? AJR Am J Roentgenol. 1997. 168:325–328.
19. Berlin L. Failure to diagnose lung cancer: anatomy of a malpractice trial. AJR Am J Roentgenol. 2003. 180:37–45.
20. Yankelevitz DF, Henschke CI. Small solitary pulmonary nodules. Radiol Clin North Am. 2000. 38:471–478.
21. Henschke CI, McCauley DI, Yankelevitz DF, Naidich DP, McGuinness G, Miettinen OS, et al. Early lung cancer action project: overall design and findings from baseline screening. Lancet. 1999. 354:99–105.
22. Winer-Muram HT, Jennings SG, Tarver RD, Aisen AM, Tann M, Conces DJ, et al. Volumetric growth rate of stage I lung cancer prior to treatment: serial CT scanning. Radiology. 2002. 223:798–805.
23. Swensen SJ, Viggiano RW, Midthun DE, Müller NL, Sherrick A, Yamashita K, et al. Lung nodule enhancement at CT: multicenter study. Radiology. 2000. 214:73–80.
24. Keagy BA, Starek PJ, Murray GF, Battaglini JW, Lores ME, Wilcox BR. Major pulmonary resection for suspected but unconfirmed malignancy. Ann Thorac Surg. 1984. 38:314–316.
25. Gould MK, Lillington GA. Strategy and cost in investigating solitary pulmonary nodules. Thorax. 1998. 53:Suppl 2. S32–S37.
26. Melin JA, Piret LJ, Vanbutsele RJ, Rousseau MF, Cosyns J, Brasseur LA, et al. Diagnostic value of exercise electrocardiography and thallium myocardial scintigraphy in patients without previous myocardial infarction: a Bayesian approach. Circulation. 1981. 63:1019–1024.
27. Goldsmith SJ, Kostakoglu L. Nuclear medicine imaging of lung cancer. Radiol Clin North Am. 2000. 38:511–524.
28. Schultz EM, Sanders GD, Trotter PR, Patz EF Jr, Silvestri GA, Owens DK, et al. Validation of two models to estimate the probability of malignancy in patients with solitary pulmonary nodules. Thorax. 2008. 63:335–341.
29. Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Matsushita T, et al. Small solitary pulmonary nodules (< or =1 cm) detected at population-based CT screening for lung cancer: reliable high-resolution CT features of benign lesions. AJR Am J Roentgenol. 2003. 180:955–964.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download