Abstract
Background
Belotecan (Camtobell, CKD-602, Chongkundang Pharm., Korea), a camptothecin derivative, has anticancer effects by inhibiting topoisomerase I such as topotecan. This study observed the response, survival and toxicity of belotecan monotherapy after the failure of etoposide and platinum (EP).
Methods
Forty nine small cell lung cancer (SCLC) patients (M/F=41/8; age, 64.5±7.6 (mean±SD) years), who failed in their first line chemotherapy were enrolled in this study. Twenty one SCLC patients showed relapsed lung cancer more than 90 days after their prior EP chemotherapy (sensitive relapse group, SR) and 28 patients relapsed within 90 days (refractory relapse group, RR).
Results
The response rate was 25%. Eleven patients showed partial responses and 5 patients could not be checked. The response rate of the SR and RR patients was similar. The relative dose intensity was lower in the responders (78±15%) than non-responders (83±13%, p=0.03). The median survival time (MST) was 10.3 months (290 days). The MST of the non-responders and responders was 186 days (95% CI; 67~305) and 401 days (95% CI; 234~568, p=0.07), respectively. The median progression free survival (MPFS) was similar in the SR (79 days) and RR (67 days) patients. Grade 3~4 neutropenia, anemia, and thrombocytopenia were observed in 59.6%, 12.8% and 23.4% of patients, respectively.
Small cell lung cancer (SCLC) accounts for 14% of new lung cancer cases, or about 77,000 of the estimated 550,000 lung cancers in the USA and Europe in 20041. Chemotherapy is the main treatment option for patients with SCLC, leading to a 5-year survival of about 20% in limited disease (LD), and less than 5% in extensive disease (ED). Although initial tumor response rate to Etoposide and Cisplatin combination (EP) chemotherapy is very high2, the vast majority of SCLC patients relapses in approximately 4 months in ED and 12 months in LD after completion of first-line chemotherapy3.
These relapsed small cell lung cancers have been treated by camptothecin analogues and Topotecan has been extensively tested in the second-line therapy of SCLC. In a phase II Study of Topotecan, overall response rate and median survival were 6.4% and 4.7 months in refractory relapse, 37.8% and 6.9 months in sensitive relapse patients4. Belotecan (Camtobell, CKD-602, Chongkundang Pharm., Seoul, Korea), newly developed camptothecin analog derived from Camptotheca acuminata, is a semi-synthetic and total synthetic water-soluble agent with targeting to topoisomerase I and activity various human tumor cell lines. Phase I studies, involving many different schedules of administration, have identified neutropenia as the dose-limiting toxicity and enabled identification of 0.5 mg/m2/d intravenously daily for 5 days repeated every 21 days, as the recommended dose and schedule for phase II studies. But, the clinical results of belotecan have not been published sufficiently. To aim of this study is to assess response rate, hematologic and non hematologic toxicity and overall clinical experiences of belotecan.
The eligible patients for this study were required to meet all of the following criteria: 1) Histologically or cytologically confirmed SCLC, 2) progressive disease after one first-line chemotherapy not including camptothecin analogues, 3) age 18~80 years inclusive, 4) ECOG Performance score below 2, 5) life expectancy above 3 months, and 6) written informed consent, 7) presence of at least one bidimensionally measurable disease, 8) WBC count greater than 3,500×109/L, absolute granulocyte count ≥1,500×109/L, hemoglobin ≥9.0 g/dl, platelet ≥100×109/L, 9) total bilirubin level ≤1.5 mg/dl, AST and ALT ≤two times the upper normal limit in absence of liver metastasis, creatinine level ≤1.5 mg/dl and a calculated creatinine clearance >60 ml/min. Patients with increased bilirubin (up to 2.5 times the upper normal limit) because of liver metastases were also considered eligible. Patients must have been off all previous systemic chemotherapy at least 3 weeks before study entry and must have recovered from the side effects of prior therapy. Patients with brain metastases were eligible provided that neurologic symptoms were under control with radiotherapy or steroid treatment, and the brain was not the only site of assessable disease.
Belotecan (CKD-602) was administered intravenously, 0.5 mg/m2/d (diluted in 100 ml of 5% dextrose water) as a 30-minute infusion for 5 consecutive days. Chemotherapy treatment schedule were repeated every 3 weeks if neutrophil count was more than or equal to 1.5×109/L, the platelet count was more than or equal to 100×109/L and recovery to Common Toxicity Criteria (CTC) grade I nonhematologic toxicity had occurred. Belotecan dose reduction 0.1 mg/m2/d was to be performed in case of grade IV neutropenia complicated by fever or lasing 7 days or longer, grade III neutropenia lasting beyond day 21 of the treatment cycle, or grade IV thrombocytopenia. Also same dose reduction were applied to grade III or IV nonhematologic toxicity (excluding grade III Nausea), or the patient could be withdrawn from the study.
To evaluate the Responses of tumor lesions and toxicity profiles, we monitored chest radiography, computed tomography (CT) scans, complete blood cell counts, and blood chemistries. The response could be evaluated in 42 patients who were treated with belotecan above 1 cycle. And we observed overall response rate, survival and toxicities of belotecan monotherapy (0.5 mg/m2 for 5 days every 21 days) after failure of etoposide and platinum (EP).
Statistical analyses were done using SPSS for Window version 12.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics, frequency tables, x2 tests were used.
Survival time and time to progression were recorded as days from the beginning of belotecan treatment. Kaplan-Meier method was used to calculate survival and time to progression according to predictors were done using a log-rank test.
From Aug 2004 to Oct 2006, the 49 patients were entered onto the study and 44 patients could be evaluated the response and toxicity profiles. 5 patients could not follow up on the response. Reason for loss to follow-up were death and poor physical status. The characteristics of enrolled patients are summarized in Table 1. The mean age of 64.5±7.6 (mean±SD) years. All of patients were treated by etoposide and platinum combination chemotherapy (EP) as first-line chemotherapy. Responses to previous first-line chemotherapy (etoposide/platinum) were partial remission (PR) in 29, stable disease (SD) in 7, progression (PD) in 9, and not evaluable in 4 cases. 21 patients showed relapse more than 90 days after prior EP therapy (sensitive relapse, SR) and 28 patients relapsed within 90 days after prior chemotherapy (refractory relapse, RR).
Dose intensity was calculated as the sum of the daily doses delivered during the course divided by the duration of the course in weeks. Relative dose intensity was 78±15% in responders and 83±13% in non-responders (p=0.03).
Within the 49 eligible patients, 5 patients could not be evaluated for response because of inadequate radiologic assessment. After receiving belotecan above at least 1 cycle of the 44 assessable patients, 11 patients showed partial remission, 19 patients remained stable, and 10 patients showed progression of their disease. The overall response rate was 25% (11/44) and the disease control rate (partial remission+stable disease) was 75%. There were no significant difference in response rate between sensitive and refractory patients group (6 PRs, 10 SDs and 4 PDs in sensitive relapses; 5 PRs, 12 SDs and 7 PDs in refractory patients).
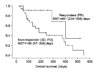
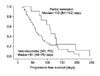
Median survival time (MST) from the beginning of belotecan treatment was 10.3 months (290 days). MST of non-responders were 186 days (95% CI; 67~305), while responders were 401 days (95% CI; 234~568, p=0.07) (Figure 1). MST was not different between SR (290 days) and RR (376 days). Median progression free survival (MPFS) was 73 days (95% CI; 48~98 days). MPFS of responders was 112 days in contrast to 61 days of non-responders (p=0.06, Figure 2). MPFS was not different between SR (79 days) and RR (67 days).
The overall survival of small cell lung cancer patients has not been increased in spite of high response rate to initial chemotherapy5. In the relapsed patient after first-line chemotherapy, survival for patients on supportive care is not sufficiently long. But world-wide used second line chemotherapeutic agents showed somewhat improving survival and cancer related symptoms6.
Belotecan, novel camptothecin derivative agent, is a cytotoxic alkaloid that is extracted from leaves of Camptotheca acuminate, which is a tree endemic in China. The preclinical studies showed the equivalent or superior to those of camptothecin and topotecan in the tumor cell cytotoxicity7.
In phase II study of topotecan, the overall response rate was 37.8% and median survival of 5.4 months4,5. Ardizzoni et al.4 also reported 74.9% of grade III/IV neutropenia, 29.5% of grade III/IV thrombocytopenia and mild nonhematologic adverse events. Also, von Pawel et al.8 reported the overall response of 54% and median survival of 25 weeks.
Irinotecan is the other available topoisomerase I inhibitor. In the phase II clinical trials, irinotecan appears the 33.3% in the relapsed small cell lung cancer after first-line chemotherapy, also showed the major toxicities in hematologic complications and diarrhea.
In our study, the result of belotecan showed 25% of overall response rate and 75% of disease control rate in chemo-sensitive and resistant groups. This result was no inferiority compared with other topoisomerase I inhibitors.
The median survival and progression free survival (MPFS) of all patients was 10.3 months (290 days) and 73 days. We have analyzed the MST and MPFS to chemo-sensitive and resistant groups. The MST and MPFS show no significant differences between SR and RR. Eckardt et al.9 reported an overall survival time of 30 weeks in the pooled analysis of 3 trials in which patients with chemo-sensitive SCLC were treated with topotecan. The median survival of these two studies showed the more reliable result in Belotecan treatment group. And we are following up survival time of remained responders.
In the other phase II clinical trials, Belotecan appears the 24% of overall objective response rates in the rlapsed small cell lung cancer after first-line chemotherapy. Median follow-up duration of 6.3 months, median time to progression was 4.4 months (95% CI; 2.6~6.3) and median overall survival wasn't reached10. Overall response rate was not different with our results.
In conclusion, this result of belotecan, new camptothecin derivative, showed possibility of development of new chemotherapeutic agent in small cell lung cancer, which warrants the comparative study between belotecan and other camptothecins.
Figures and Tables
Figure 1
Overall survival in responders. The figure showed better overall survival in responders with belotecan compared to in non-responders: mean survival time of non-responders was 186 days (95% CI; 67~305), while was 401 days in responders (95% CI; 234~568, p=0.07).
References
1. Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004. 54:8–29.
2. Jackman DM, Johnson BE. Small-cell lung cancer. Lancet. 2005. 366:1385–1396.
3. Simon GR, Wagner H. Small cell lung cancer. Chest. 2003. 123:259S–271S.
4. Ardizzoni A, Hansen H, Dombernowsky P, Gamucci T, Kaplan S, Postmus P, et al. Topotecan, a new active drug in the second-line treatment of small-cell lung cancer: a phase II study in patients with refractory and sensitive disease. The european organization for research and treatment of cancer early clinical studies group and new drug development office, and the lung cancer cooperative group. J Clin Oncol. 1997. 15:2090–2096.
5. Rocha Lima CM, Chiappori A. Treatment of relapsed small-cell lung cancer--a focus on the evolving role of topotecan. Lung Cancer. 2003. 40:229–236.
6. Spiro SG, Souhami RL, Geddes DM, Ash CM, Quinn H, Harper PG, et al. Duration of chemotherapy in small cell lung cancer: a cancer research campaign trial. Br J Cancer. 1989. 59:578–583.
7. Lee JH, Lee JM, Lim KH, Kim JK, Ahn SK, Bang YJ, et al. Preclinical and phase I clinical studies with Ckd-602, a novel camptothecin derivative. Ann N Y Acad Sci. 2000. 922:324–325.
8. von Pawel J, Schiller JH, Shepherd FA, Fields SZ, Kleisbauer JP, Chrysson NG, et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol. 1999. 17:658–667.
9. Eckardt JR, Ardizzoni A, von Pawel J, Fields S. Pooled analysis of topotecan in the second-line treatment of patients with sensitive small cell lung cancer. Proc Am Soc Clin Oncol. 1997. 15:1624a.
10. Jeong JH, Kim SH, Choi HJ, Shin SJ, Cho BC, Kuen IC, et al. Phase II trial of belotecan in patients with relapsed small-cell lung cancer after irinotecan-containing chemotherapy. Korean J Med. 2007. 73:S155.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download