Abstract
Background
The aim of this study was to consider the significance of pleural fluid adenosine deaminase (ADA) activity combined with lymphocyte/neutrophil (L/N) ratio in the diagnosis of tuberculous pleurisy (TBpl) in a region of intermediate prevalence of tuberculosis (TB).
Methods
We collected data from 388 patients with exudative pleural effusions. The final diagnoses were compared to the results from our diagnostic method using pleural fluid ADA and L/N ratio.
Results
108 patients had a final diagnosis of TBpl; 102 cases had high levels of ADA (≥40 IU/L). When we considered ADA ≥40 IU/L as a diagnostic criterion, the sensitivity was 94.4%, specificity 87.5%, and post-test probability 74.5%. However, when we considered ADA ≥40 IU/L combined with the L/N ratio ≥0.75 as a diagnostic criterion, the specificity and post-test probability were rose to 97.5% and 93%, respectively. The other causes of high ADA and L/N ratios were lymphoma and metastatic carcinoma, but mass-like lesions were found on the chest radiographs or CT scans.
According to the WHO report in 2007, South Korea is the region of intermediate prevalence of tuberculosis (TB). Tuberculous pleurisy (TBpl) is the most common cause of lymphocyte-dominant, exudative pleural effusion in Korea, but the diagnosis can be difficult because of the low sensitivities and specificities of the traditional bacteriologic diagnostic methods. One third of the patients with TBpl have a negative tuberculin test, only about 5% are detected by Ziehl-Neelsen stain, and only 25~37% are identified by the culture of Mycobacterium tuberculosis in pleural fluid samples, which furthermore takes 2~6 weeks1. Meanwhile, diagnostic yields of needle pleural biopsy are about 80%. Needle biopsy done with both histological and microbiological studies can improve the results, and thoracoscopic biopsy demonstrates better diagnostic yields of over 90%2. However, pleural biopsy might cause serious complications such as hemothorax, and it can't be easily performed in uncoorperative patients. Hence, there are an abundance of studies regarding the ancillary utilities for diagnosing TBpl.
Measuring the level of adenosine deaminase (ADA) activity in pleural fluid is the best-known marker of TBpl. The pathogenesis in development of pleural effusion in patients with TBpl is considered as a delayed hypersensitivity to the protein of acid-fast bacilli3, and it is suggested that macrophages and activated CD4+ T lympocytes take part in the process1. ADA is known to contribute to the differentiation and maturation of these T-lymphocytes and macrophages4. Since 1978, when Piras et al5 first reported the utility of its determination in pleural fluid as a means of diagnosing TBpl, many studies have investigated the usefulness of ADA for the rapid diagnosis of TBpl6,7. A recent meta-analysis of original articles pertaining to the diagnostic value of ADA found that overall sensitivity and specificity of ADA was as high as 92.2%8. It was also suggested that pleural biopsy might not be necessary in the regions where the prevalence of TB is high and if lymphocytes predominate in the pleural fluid8,9. Additionally, a report displayed that using pleural fluid ADA combined with the lymphocyte/neutrophil (L/N) ratio increased the specificity up to 95% in diagnosing TBpl10. Thereafter, many researchers tried to make up for the shortage of ADA by integrating other clinical data such as age, the level of lactate dehydrogenase (LDH), and the pleural fluid lymphocyte/neutrophil ratio in pleural fluid with ADA11-14.
Attempts have been made to use other ancillary markers in diagnosing TBpl, but actually ADA is the most useful owing to its convenience, higher sensitivity, and lower cost. However, it has some problems related with false-positivity and variable diagnostic values according to the prevalence of TB. Therefore, we observed the differences in sensitivity, specificity, negative predictive value, likelihood ratio, and post-test probability among the different levels of ADA. We also reevaluated the possibility of improving diagnostic efficiency when we applied the L/N ratio combined with pleural fluid ADA in diagnosing TBpl in a region of intermediate prevalence of TB.
Among the patients who were admitted into Kangdong Sacred Heart Hospital between January 1, 2004 and December 31, 2005, we selected 487 patients on whom diagnostic thoracentesis was performed and the level of pleural fluid ADA activity was measured. We excluded 14 patients because the differential count of pleural fluid leukocyte had not been examined. 85 patients were additionally excluded because their pleural effusions were transudates according to Light's criteria. After all, we collected data from 388 patients with exudative pleural effusion and reviewed their medical histories, clinical features, and radiologic findings. The results from our diagnostic method using pleural fluid ADA activity combined with the L/N ratio were compared with their final diagnoses. The review of patients' charts was approved by the institutional review board of the hospital.
Pleural effusions were diagnosed as TB if they corresponded with these 4 subclasses: (1) identification of TB in pleural fluid or biopsy specimen by stain, culture, or PCR (polymerase chain reaction); (2) presence of granulomas in pleural biopsy tissue; (3) positive sputum stain, culture, or PCR for Mycobacterium tuberculosis in the presence of clinical or radiologic evidence for TB in the absence of any other obvious cause associated with pleural effusions; (4) clinical or radiologic suspicion for TB in the absence of any other obvious cause associated with pleural effusions and related to a positive response to antituberculous therapy.
The level of pleural fluid ADA activity was measured by an autoanalyzer (model 7170; Hitachi, Tokyo, Japan). The unit of ADA was given in IU/L. All statistical data were presented as average±standard deviation. Data were analyzed with SPSS Windows version 10.0.7 (SPSS Inc., Chicago, IL, USA). We used Independent Samples T-test to compare differences. Correlations were quantified by means of the Pearson Correlation Coefficient. Differences were considered significant at p<0.05 in all statistical tests.
108 out of a total of 388 patients were finally diagnosed as having TBpl. Ages of the cases were distributed rom 15 to 89. The mean age was 45.6±21.7, and 73% of the patients were less than 65. A relatively higher frequency of TBpl occurred in patients in their 20~30's and 50~70's (Table 1), and the number of male patients was slightly larger (61%).
Concerning the method of diagnosis, M. tuberculosis was identified in pleural fluid by culture or PCR in 4 cases, granulomas were found in pleural biopsy tissue in 56 cases, sputum culture or PCR were positive in 26 cases, and the other 22 cases were clinically suspected and improved by antituberculous therapy.
The mean level of pleural fluid ADA activities in 108 patients of TBpl was 87.2±33.8 IU/L. There was no difference in the mean level of ADA between patients over 65 and less than 65 (Table 2).
When we regarded pleural fluid ADA activity ≥40 IU/L as a diagnostic criterion, the sensitivity was 94.4%, specificity 87.5%, negative predictive value 97.6%, and post-test probability 74.5%. Using the criterion of ADA activity ≥45 IU/L, the sensitivity fell slightly to 93.5%, and negative predictive value was much the same, but specificity and post-test probability increased to 90% and 78.3%, respectively. Considering ADA ≥48 IU/L, the positive likelihood ratio was over 10 (Table 3). The area under the ROC curve for pleural fluid ADA activity was 0.943. It would be considered as 'very good' for separating TBpl from the other causes of exudative pleural effusion (Figure 1).
However, when we considered ADA activity ≥40 IU/L combined with L/N ratio ≥0.75 as diagnostic criteria, the specificity and post-test probability rose considerably to 97.5% and 93%, respectively. Also, the positive likelihood ratio was 35.9, which was far more than 10. Using the criteria of ADA ≥45 IU/L and L/N ratio ≥0.75, the specificity and post-test probability increased a little more, but the sensitivity tended to decline. In brief, considering pleural fluid ADA activity combined with the L/N ratio demonstrated a higher positive likelihood ratio and better specificity and post-test probability in spite of the lower level of pleural fluid ADA (Table 3).
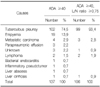
The other causes of exudative pleural effusions with elevated ADA level (≥40 IU/L) except TB were empyema, parapneumonic effusion, metastatic carcinoma, lymphoma, bacterial endocarditis, inflammatory pseudotumor, liver abscess, and liver cirrhosis. However, when combined with the L/N ratio, all of the patients with infectious causes such as empyema, parapneumonic effusion, and liver abscess were completely excluded. In other words, using the criteria of ADA ≥40 IU/L and L/N ratio ≥0.75, 93.4% patients had real TBpl, and other patients had malignancy including lymphoma (Table 4). Among them, of 2 patients diagnosed as having lymphoma, mass lesions were detected on the chest radiographs and CT scans. In all the 4 patients with metastatic carcinoma, we also could find mass-like lesions on their chest or abdominal CT scans which were finally identified as primary lung cancer, gastric cancer with lung metastasis, and rectal cancer with hepatic metastasis.
Meanwhile, there were 6 patients who were finally diagnosed as TBpl but had pleural fluid ADA activities below 40 IU/L. They accounted for 5.6% of the 108 patients with TBpl. Three of them were diagnosed by pleural biopsies, one by culture of sputum, another one by TB-PCR of sputum, and the other was diagnosed clinically on the basis of a positive response to anti-tuberculous therapy.
The definite diagnosis of TBpl requires either identification of Mycobacterium tuberculosis in cultures of pleural fluid or pleural biopsy tissue, or observation of granulomas in the latter. However, the efficiency of culture is quite low, and the procedure of pleural biopsy is somewhat invasive. Owing to these shortcomings, diverse ancillary markers were evaluated to be used in diagnosing TBpl such as ADA, lysozyme, interferon-γ, and TB-PCR. However, the cost of TB-PCR was high and its sensitivity was very low. The sensitivity of lysozyme also was not high. The sensitivity and specificity of interferon-γ were as high as ADA activity, yet it is much more expensive to quantify than ADA1,2,15,16. Several cytokines and receptors were investigated as potential markers of TBpl, but until now, the determination of ADA activity in pleural fluid has been the most useful method in regard to the aspects of sensitivity, specificity, and cost.
For the differentiation of the lymphoid cells, particularly T lymphocytes, and the maturation of monocytesmacrophages because of the metabolic requirement, it is necessary to rely on the presence of ADA4,17. For that reason, ADA has been looked on as a marker of cell-mediated immunity, which is the key mechanism of tuberculous pleural effusion. Meanwhile, age-associated immune decline is characterized by decreases in both B and T lymphocyte function, and the former may be largely a result of the latter. Therefore, pleural fluid ADA activity would be lower in old rather than in young patients with TBpl18. However, the level of pleural fluid ADA among HIV-positive patients complicated with TBpl did not differ from the level among HIV-negative patients19. In our study, there was no significant relationship between age and pleural fluid ADA activity.
Several reports describe the sensitivity and specificity of ADA level in the patients with pleural effusion. The sensitivity is 90~100% and the specificity is 89~100%. Unfortunately, knowledge of the sensitivity and specificity of the test offers little clinical utility when evaluating individual patients. The utility was determined by the prevalence of TBpl20,21. In the area with high prevalence of TB, the proportion of false-positive results is lower, but positive predictive value decreases. We would like to clarify which parameters could be used as alternative to invasive pleural biopsy in countries with intermediate prevalence of tuberculous pleural effusion.
Clinical parameters such as age, sex, history of contact with patients with TB, and chest radiographic findings of tuberculous lesions held no predictive value although the data were not shown.
Likelihood ratio is the likelihood that a given test result would be expected in a patient with the target disorder compared to the likelihood that the same result would be expected in a patient without the target disorder. Likelihood ratio can combine the information about the prevalence of the disease and characteristics of the patient pool.
When we use the criterion of ADA activity ≥48 IU/L, the positive likelihood ratio was 10.37. Likelihood ratios of >10 or <0.1 generate large and often conclusive shifts from pretest to posttest probability (indicating high accuracy)22. Because we considered ADA ≥40 IU/L combined with the L/N ratio ≥0.75 as diagnostic criteria, specificity and post-test probability were exceedingly high, and the positive likelihood ratio was even higher at 35.9. This value suggests that patients with TBpl have an approximately 36-fold more chance of being ADA assay-positive compared with patients without TBpl.
There are other causes of exudative lymphocytic pleural effusions excluding TB such as malignancy, connective tissue disorders, sarcoidosis, chylothorax, and pulmonary thromboembolism23. Besides TBpl, ADA levels are also raised in empyema, rheumatoid pleurisy, and malignancy24,25. In this study, the other causes of exudative pleural effusions with elevated ADA were empyema, parapneumonic effusion, metastatic carcinoma, lymphoma, liver abscess, bacterial endocarditis, inflammatory pseudotumor, and liver cirrhosis, and when combined with the L/N ratio, the causes related to bacterial infection were completely excluded. Like this, the combined approach with pleural fluid ADA and the L/N ratio proved to be useful in differentiating between TBpl and para-infective effusions10, but it was of no use for discerning TBpl from malignancy including lymphoma. However, in the cases of malignancy, we could detect mass-like lesions on simple chest radiographs or CT scans.
As we put the results of our study and the literature cited together, it became clear that using pleural fluid ADA activity in combination with the L/N ratio is a minimally invasive, inexpensive, relatively accurate, and the most efficient method for diagnosing TBpl. Therefore, to evaluate the causes of exudative pleural effusions in a region of intermediate prevalence of TB, we recommend measuring pleural fluid ADA and the L/N ratio first. If the result is high enough, and malignancy is not suspected clinically or radiographically, it can be diagnosed as TBpl.
There is a limitation because it is a retrospective observational study. A prospective trial is needed on a larger group of patients. Especially, a larger proportion of malignant effusion will enhance the generalizability of our findings.
Figures and Tables
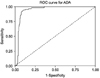 | Figure 1The receiver operator characteristic (ROC) curve for pleural fluid ADA activity. The area under the curve is 0.943. |
References
1. Valdés L, Pose A, San José E, Martínez Vázquez JM. Tuberculous pleural effusions. Eur J Intern Med. 2003. 14:77–88.
2. Ferrer J. Pleural tuberculosis. Eur Respir J. 1997. 10:942–947.
3. Berger HW, Mejia E. Tuberculous pleurisy. Chest. 1973. 63:88–92.
4. Pérez-Rodriguez E, Jiménez Castro D. The use of adenosine deaminase and adenosine deaminase isoenzymes in the diagnosis of tuberculous pleuritis. Curr Opin Pulm Med. 2000. 6:259–266.
5. Piras MA, Gakis C, Budroni M, Andreoni G. Adenosine deaminase activity in pleural effusions: an aid to differential diagnosis. Br Med J. 1978. 2:1751–1752.
6. Mo EK, Oh YM, Jung MP, Lee KY, Yoo CG, Kim YW. A prospective study on the diagnostic value of adenosine deaminase activity in tuberculous pleural effusion. Korean J Med. 1995. 48:625–632.
7. Valdés L, Alvarez D, San José E, Penela P, Valle JM, García-Pazos JM, et al. Tuberculous pleurisy: a study of 254 patients. Arch Intern Med. 1998. 158:2017–2021.
8. Goto M, Noguchi Y, Koyama H, Hira K, Shimbo T, Fukui T. Diagnostic value of adenosine deaminase in tuberculous pleural effusion: a meta-analysis. Ann Clin Biochem. 2003. 40:374–381.
9. Valdés L, Alvarez D, San José E, Juanatey JR, Pose A, Valle JM, et al. Value of adenosine deaminase in the diagnosis of tuberculous pleural effusions in young patients in a region of high prevalence of tuberculosis. Thorax. 1995. 50:600–603.
10. Burgess LJ, Maritz FJ, Le Roux I, Taljaard JJ. Combined use of pleural adenosine deaminase with lymphocyte/ neutrophil ratio. Increased specificity for the diag nosis of tuberculous pleuritis. Chest. 1996. 109:414–419.
11. Diacon AH, Van de Wal BW, Wyser C, Smedema JP, Bezuidenhout J, Bolliger CT, et al. Diagnostic tools in tuberculous pleurisy: a direct comparative study. Eur Respir J. 2003. 22:589–591.
12. Ghanei M, Aslani J, Bahrami H, Adhami H. Simple method for rapid diagnosis of tuberculosis pleuritis: a statistical approach. Asian Cardiovasc Thorac Ann. 2004. 12:23–29.
13. Porcel JM, Vives M. Differentiating tuberculous from malignant pleural effusions: a scoring model. Med Sci Monit. 2003. 9:CR175–CR180.
14. Jeon EJ, Kwak HW, Song JH, Lee YW, Jeong JW, Choi JC, et al. Diagnostic value of ADA multiplied by lymphocyte to neutrophil ratio in tuberculous pleurisy. Tuberc Respir Dis. 2007. 63:17–23.
15. Roth BJ. Searching for tuberculosis in the pleural space. Chest. 1999. 116:3–5.
16. Ferrer Sancho J. Pleural tuberculosis: incidence, pathogenesis, diagnosis, and treatment. Curr Opin Pulm Med. 1996. 2:327–334.
17. Pace E, Gjomarkaj M, Melis M, Profita M, Spatafora M, Vignola AM, et al. Interleukin-8 induces lymphocyte chemotaxis into the pleural space: role of pleural macrophages. Am J Respir Crit Care Med. 1999. 159:1592–1599.
18. Kim CJ, Yeon KM, Kim ST, Wang JH, Yoo KH. Relationship between age and pleural fluid adenosine deaminase activity in patients with tuberculous pleural effusion. Tuberc Respir Dis. 2002. 52:608–615.
19. Riantawan P, Chaowalit P, Wongsangiem M, Rojanaraweewong P. Diagnostic value of pleural fluid adenosine deaminase in tuberculous pleuritis with reference to HIV coinfection and a Bayesian analysis. Chest. 1999. 116:97–103.
20. Laniado-Laborin R. Adenosine deaminase in the diagnosis of tuberculous pleural effusion: is it really an ideal test? A word of caution. Chest. 2005. 127:417–418.
21. Kataria YP, Khurshid I. Adenosine deaminase in the diagnosis of tuberculous pleural effusion. Chest. 2001. 120:334–336.
22. Jaeschke R, Guyatt G, Lijmer J. Guyatt G, Rennie D, editors. Diagnostic tests. Users' guides to the medical literature: a manual for evidence-based clinical practice. 2002. 1st ed. Chicago: AMA Press;121–140.
23. Lee YC, Rogers JT, Rodriguez RM, Miller KD, Light RW. Adenosine deaminase levels in nontuberculous lymphocytic pleural effusions. Chest. 2001. 120:356–361.
24. Light RW. Diagnostic principles in pleural disease. Eur Respir J. 1997. 10:476–481.
25. Maskell NA, Butland RJ. BTS guidelines for the investigation of a unilateral pleural effusion in adults. Thorax. 2003. 58:Suppl 2. ii8–ii17.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download