Abstract
Background
First-line drugs, if sensitive, are the most potent drugs in the treatment of multidrug-resistant tuberculosis (MDR-TB). This study examined the frequency and risk factors associated with acquired drug resistance to first-line drugs during a standardized treatment using first-line drugs in patients with MDR-TB.
Methods
This study included patients who were diagnosed with MDR-TB at the National Masan Tuberculosis Hospital between January 2004 and May 2008, treated with standardized first-line drugs, and for whom the preand post-treatment results of the drug susceptibility test were available. Their medical records were reviewed retrospectively.
Results
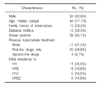
Of 41 MDR-TB patients, 14 (34.1%) acquired additional resistance to ethambutol (EMB) or pyrazinamide (PZA). Of 11 patients initially resistant to isoniazid (INH) and rifampicin (RFP), 3 (27.3%) acquired additional resistance to both EMB and PZA, and 3 (27.3%) to PZA. Of 18 patients initially resistant to INH, RFP and EMB, 6 (33.3%) acquired additional resistance to PZA. Of 6 patients initially resistant to INH, RFP and PZA, 2 (33.3%) acquired additional resistance to EMB. Ten of the 41 MDR-TB patients (24.4%) changed from resistant to susceptible. No statistically significant risk factors associated with acquired resistance could be found.
Figures and Tables
References
1. Kim HJ, Hong YP, Kim SJ, Lew WJ, Lee EG. Ambulatory treatment of multidrug-resistant pulmonary tuberculosis patients at a chest clinic. Int J Tuberc Lung Dis. 2001. 5:1129–1136.
2. Park SK, Lee WC, Lee DH, Mitnick CD, Han L, Seung KJ. Self-administered, standardized regimens for multidrug-resistant tuberculosis in South Korea. Int J Tuberc Lung Dis. 2004. 8:361–368.
3. Kim HR, Hwang SS, Kim HJ, Lee SM, Yoo CG, Kim YW, et al. Impact of extensive drug resistance on treatment outcomes in non-HIV-infected patients with multidrug-resistant tuberculosis. Clin Infect Dis. 2007. 45:1290–1295.
4. Kwon YS, Kim YH, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Treatment outcomes for HIV-uninfected patients with multidrug-resistant and extensively drug-resistant tuberculosis. Clin Infect Dis. 2008. 47:496–502.
5. Kim DH, Kim HJ, Park SK, Kong SJ, Kim YS, Kim TH, et al. Treatment outcomes and long-term survival in patients with extensively drug-resistant tuberculosis. Am J Respir Crit Care Med. 2008. 178:1075–1082.
6. Mukherjee JS, Rich ML, Socci AR, Joseph JK, Virú FA, Shin SS, et al. Programmes and principles in treatment of multidrug-resistant tuberculosis. Lancet. 2004. 363:474–481.
7. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis: emergency update 2008. 2008. Geneva: World Health Organization.
8. Migliori GB, Besozzi G, Girardi E, Kliiman K, Lange C, Toungoussova OS, et al. Clinical and operational value of the extensively drug-resistant tuberculosis definition. Eur Respir J. 2007. 30:623–626.
9. Joh JS, Lee CH, Lee JE, Park YK, Bai GH, Kim EC, et al. The interval between initiation of anti-tuberculosis treatment in patients with culture-positive pulmonary tuberculosis and receipt of drug-susceptibility test results. J Korean Med Sci. 2007. 22:26–29.
10. Kim MN, Lee SH, Yang SE, Pai CH. Mycobacterial testing in hospital laboratories in Korea: results of a survey of 40 university or tertiary-care hospitals. Korean J Clin Pathol. 1999. 19:86–91.
11. National Tuberculosis Association. Diagnostic standards and classification of tuberculosis. 1961. 11th ed. New York: National Tuberculosis Assoication.
12. American Thoracic Society. Centers for Disease Control and Prevention. Infectious Diseases Society of America. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: controlling tuberculosis in the United States. Am J Respir Crit Care Med. 2005. 172:1169–1227.
13. Mitchison DA. How drug resistance emerges as a result of poor compliance during short course chemotherapy for tuberculosis. Int J Tuberc Lung Dis. 1998. 2:10–15.
14. Farmer P, Bayona J, Becerra M, Furin J, Henry C, Hiatt H, et al. The dilemma of MDR-TB in the global era. Int J Tuberc Lung Dis. 1998. 2:869–876.
15. Umubyeyi A, Shamputa IC, Rigouts L, Dediste A, Struelens M, Portaels F. Evidence of 'amplifier effect' in pulmonary multidrug-resistant tuberculosis: report of three cases. Int J Infect Dis. 2007. 11:508–512.
16. Quy HT, Lan NT, Borgdorff MW, Grosset J, Linh PD, Tung LB, et al. Drug resistance among failure and relapse cases of tuberculosis: is the standard re-treatment regimen adequate? Int J Tuberc Lung Dis. 2003. 7:631–636.
17. Yoshiyama T, Yanai H, Rhiengtong D, Palittapongarnpim P, Nampaisan O, Supawitkul S, et al. Development of acquired drug resistance in recurrent tuberculosis patients with various previous treatment outcomes. Int J Tuberc Lung Dis. 2004. 8:31–38.
18. Temple B, Ayakaka I, Ogwang S, Nabanjja H, Kayes S, Nakubulwa S, et al. Rate and amplification of drug resistance among previously-treated patients with tuberculosis in Kampala, Uganda. Clin Infect Dis. 2008. 47:1126–1134.
19. Seung KJ, Gelmanova IE, Peremitin GG, Golubchikova VT, Pavlova VE, Sirotkina OB, et al. The effect of initial drug resistance on treatment response and acquired drug resistance during standardized short-course chemotherapy for tuberculosis. Clin Infect Dis. 2004. 39:1321–1328.
20. Han LL, Sloutsky A, Canales R, Naroditskaya V, Shin SS, Seung KJ, et al. Acquisition of drug resistance in multidrug-resistant Mycobacterium tuberculosis during directly observed empiric retreatment with standardized regimens. Int J Tuberc Lung Dis. 2005. 9:818–821.
21. Cox HS, Niemann S, Ismailov G, Doshetov D, Orozco JD, Blok L, et al. Risk of acquired drug resistance during short-course directly observed treatment of tuberculosis in an area with high levels of drug resistance. Clin Infect Dis. 2007. 44:1421–1427.
22. Tenover FC, Crawford JT, Huebner RE, Geiter LJ, Horsburgh CR Jr, Good RC. The resurgence of tuberculosis: is your laboratory ready? J Clin Microbiol. 1993. 31:767–770.
23. Oh SH, Kim YJ, Park SK, Hwang SH, Kim HH, Lee EY, et al. Comparison of anti-mycobacterial drug susceptibility test results by institutes and methods. Korean J Clin Microbiol. 2008. 11:43–48.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download