Abstract
Background
There is limited data on the epidemiology and relative frequency of idiopathic interstitial pneumonia (IIP) worldwide. This survey was performed to assess the epidemiology and relative frequency of IIP in Korea.
Methods
The patients with IIP and who were confirmed by lung biopsy, except those patients with idiopathic pulmonary fibrosis, (IPF) over a 5 year period (from Jan. 1st, 2003 to Dec. 31st, 2007) were registered by a web-base questionnaire.
Results
A total of 3,156 cases were registered, but 970 cases were excluded due to duplicative registration, inadequate data and the unmet ATS/ERS diagnostic criteria. A total of 2,186 cases were analyzed. The male to female ratio was about 2 : 1 and their mean age was 65 (range: 11~94). The most frequent disease was IPF (77.1%), followed in decreasing order by nonspecific interstitial pneumonia (NSIP) (11.9%), cryptogenic organizing pneumonia (COP) (8.5%), acute interstitial pneumonia (AIP) (1.1%), desquamative interstitial pneumonia (DIP) (0.9%), respiratory bronchiolitis-interstitial lung disease (RB-ILD) (0.4%) and lymphocytic interstitial pneumonia (LIP) (0.1%). The mean age of the patients with IPF, NSIP and COP was 67.8, 57.1 and 57.7 years old, respectively. The most frequent symptom was dyspnea on exertion (69%) followed by coughing (61%) and sputum (33%) for the whole population. The three year survival rate was 62% for the patients with IPF and the five year survival
rate was 85% in both the NSIP and COP patients.
Figures and Tables
Figure 1
Age and sex distribution of 2,186 patients with IIP. Generally male predominates female, but female predominate male a little less than 50 year-old. IIP: idiopathic interstitial pneumonias.

Figure 2
Frequency of IIP in Korean population. Percen tages and numbers in square mean relative frequency and population of female and male, respectively. IPF was the most frequent disease in IIP. IIP: idiopathic interstitial pneumonias; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; DIP: desquamative interstitial pneumomia; LIP: lymphocytic interstitial pneumonia; NSIP: nonspecific interstitial pneumonia; RB-ILD: respiratory bronchiolitis-intertitial lung disease; IPF: idiopathic pulmonary fibrosis.

Figure 3
Mean age of patients with IIP. The age of patients with IPF was significantly older than those of COP and LIP (p<0.05). Bars mean standard deviation. IIP: idiopathic interstitial pneumonias; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; DIP: desquamative interstitial pneumomia; LIP: lymphocytic interstitial pneumonia; NSIP: nonspecific interstitial pneumonia; RB-ILD: respiratory bronchiolitis-intertitial lung disease; IPF: idiopathic pulmonary fibrosis.

Figure 4
Smoking rate in patients with IIP. DIP and RB-ILD are associated with smoking. IIP: idiopathic interstitial pneumonias; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; DIP: desquamative interstitial pneumomia; NSIP: nonspecific interstitial pneumonia; RB-ILD: respiratory bronchiolitis-intertitial lung disease; IPF: idiopathic pulmonary fibrosis.
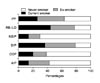
Figure 5
Associated symptoms in patients with IIP. The frequent symptoms were DOE, coughing, and sputum. IIP: idiopathic interstitial pneumonias; DOE: dyspnea on exertion; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; NSIP: nonspecific interstitial pneumonia; IPF: idiopathic pulmonary fibrosis.

Figure 6
HRCT findings in patients with IIP. IIP: idiopathic interstitial pneumonias; GGO: ground-glass opacity; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; DIP: desquamative interstitial pneumomia; NSIP: nonspecific interstitial pneumonia; RB-ILD: respiratory bronchiolitis-intertitial lung disease; IPF: idiopathic pulmonary fibrosis.

Figure 7
Treatment response in Korean patients with IIP. IIP: idiopathic interstitial pneumonias; AIP: acute interstitial pneumonia; COP: cryptogenic organizing pneumonia; DIP: desquamative interstitial pneumomia; NSIP: nonspecific interstitial pneumonia; RB-ILD: respiratory bronchiolitis-intertitial lung disease; IPF: idiopathic pulmonary fibrosis.

Figure 8
Kaplan-Meier survival curves of idiopathic interstitial pneumonia in Korean population. According to Kaplan-Meier survival curves, 3 year survival rates of AIP, IPF, and DIP were 57%, 62%, and 94%, respectively. Five years survival rates of COP and NSIP were equally 85%. AIP: acute interstitial pneumonia; IPF: idiopathic pulmonary fibrosis; DIP: desquamative interstitial pneumomia; COP: cryptogenic organizing pneumonia; NSIP: nonspecific interstitial pneumonia.

References
1. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Class ification of the Idiopathic Interstitial Pneumonias. This joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001. Am J Respir Crit Care Med. 2002. 165:277–304.
2. Xaubet A, Ancochea J, Morell F, Rodriguez-Arias JM, Villena V, Blanquer R, et al. Report on the incidence of interstitial lung diseases in Spain. Sarcoidosis Vasc Diffuse Lung Dis. 2004. 21:64–70.
3. Coultas DB, Zumwalt RE, Black WC, Sobonya RE. The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med. 1994. 150:967–972.
4. Roelandt M, Demedts M, Callebaut W, Coolen D, Slabbynck H, Bockaert J, et al. Epidemiology of interstitial lung disease (ILD) in flanders: registration by pneumologists in 1992-1994. Working group on ILD, VRGT. Vereniging voor Respiratoire Gezondheidszorg en Tuberculosebestrijding. Acta Clin Belg. 1995. 50:260–268.
5. Schweisfurth H, Kieslich C, Satake N, Loddenkemper R, Schonfeld N, Mader I, et al. How are interstitial lung diseases diagnosed in Germany? Results of the scientific registry for the exploration of interstitial lung diseases ("Fibrosis registry") of the WATL. Pneumologie. 2003. 57:373–382.
6. Tinelli C, De Silvestri A, Richeldi L, Oggionni T. The Italian register for diffuse infiltrative lung disorders (RIPID): a four-year report. Sarcoidosis Vasc Diffuse Lung Dis. 2005. 22:Suppl 1. S4–S8.
7. KIm JH, Choi SJ, Kim DS, You JH, Kang HM, You SH, et al. The etiology of the diffuse infiltrative disease of the lung in Korea. Tuberc Respir Dis. 1991. 38:1–7.
8. Flint A, Martinez FJ, Young ML, Whyte RI, Toews GB, Lynch JP 3rd. Influence of sample number and biopsy site on the histologic diagnosis of diffuse lung disease. Ann Thorac Surg. 1995. 60:1605–1607. discussion 1607-8.
9. Nagai S, Kitaichi M, Itoh H, Nishimura K, Izumi T, Colby TV. Idiopathic nonspecific interstitial pneumonia/fibrosis: comparison with idiopathic pulmonary fibrosis and BOOP. Eur Respir J. 1998. 12:1010–1019.
10. Flaherty KR, Travis WD, Colby TV, Toews GB, Kazerooni EA, Gross BH, et al. Histopathologic variability in usual and nonspecific interstitial pneumonias. Am J Respir Crit Care Med. 2001. 164:1722–1727.
11. Enomoto T, Usuki J, Azuma A, Nakagawa T, Kudoh S. Diabetes mellitus may increase risk for idiopathic pulmonary fibrosis. Chest. 2003. 123:2007–2011.
12. Bouros D, Hatzakis K, Labrakis H, Zeibecoglou K. Association of malignancy with diseases causing interstitial pulmonary changes. Chest. 2002. 121:1278–1289.
13. Ma Y, Seneviratne CK, Koss M. Idiopathic pulmonary fibrosis and malignancy. Curr Opin Pulm Med. 2001. 7:278–282.
14. Kawasaki H, Nagai K, Yokose T, Yoshida J, Nishimura M, Takahashi K, et al. Clinicopathological characteristics of surgically resected lung cancer associated with idiopathic pulmonary fibrosis. J Surg Oncol. 2001. 76:53–57.
15. Oshikawa K, Sugiyama Y. Serum anti-p53 autoantibodies from patients with idiopathic pulmonary fibrosis associated with lung cancer. Respir Med. 2000. 94:1085–1091.
16. Uematsu K, Yoshimura A, Gemma A, Mochimaru H, Hosoya Y, Kunugi S, et al. Aberrations in the fragile histidine triad (FHIT) gene in idiopathic pulmonary fibrosis. Cancer Res. 2001. 61:8527–8533.
17. Wells C, Mannino DM. Pulmonary fibrosis and lung cancer in the United States: analysis of the multiple cause of death mortality data, 1979 through 1991. South Med J. 1996. 89:505–510.
18. Desai SR, Ryan SM, Colby TV. Smoking-related interstitial lung diseases: histopathological and imaging perspectives. Clin Radiol. 2003. 58:259–268.
19. Baumgartner KB, Samet JM, Stidley CA, Colby TV, Waldron JA. Cigarette smoking: a risk factor for idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1997. 155:242–248.
20. Travis WD, Hunninghake G, King TE Jr, Lynch DA, Colby TV, Galvin JR, et al. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project. Am J Respir Crit Care Med. 2008. 177:1338–1347.
21. Lynch DA, Newell JD, Logan PM, King TE Jr, Müller NL. Can CT distinguish hypersensitivity pneumonitis from idiopathic pulmonary fibrosis? AJR Am J Roent genol. 1995. 165:807–811.
22. American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med. 2000. 161:646–664.
23. Riha RL, Duhig EE, Clarke BE, Steele RH, Slaughter RE, Zimmerman PV. Survival of patients with biopsy-proven usual interstitial pneumonia and nonspecific interstitial pneumonia. Eur Respir J. 2002. 19:1114–1118.
24. Flaherty KR, Toews GB, Travis WD, Colby TV, Kazerooni EA, Gross BH, et al. Clinical significance of histological classification of idiopathic interstitial pneumonia. Eur Respir J. 2002. 19:275–283.
25. Jeon K, Chung MP, Lee KS, Chung MJ, Han J, Koh WJ, et al. Prognostic factors and causes of death in Korean patients with idiopathic pulmonary fibrosis. Respir Med. 2006. 100:451–457.
26. Jegal Y, Kim DS, Shim TS, Lim CM, Do Lee S, Koh Y, et al. Physiology is a stronger predictor of survival than pathology in fibrotic interstitial pneumonia. Am J Respir Crit Care Med. 2005. 171:639–644.
27. Bjoraker JA, Ryu JH, Edwin MK, Myers JL, Tazelaar HD, Schroeder DR, et al. Prognostic significance of histopathologic subsets in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 1998. 157:199–203.
28. Thomeer MJ, Costabe U, Rizzato G, Poletti V, Demedts M. Comparison of registries of interstitial lung diseases in three European countries. Eur Respir J. 2001. 32:114s–118s.
29. Hodgson U, Laitinen T, Tukiainen P. Nationwide prevalence of sporadic and familial idiopathic pulmonary fibrosis: evidence of founder effect among multiplex families in Finland. Thorax. 2002. 57:338–342.
30. Turner-Warwick M, Burrows B, Johnson A. Cryptogenic fibrosing alveolitis: clinical features and their influence on survival. Thorax. 1980. 35:171–180.
31. Mapel DW, Hunt WC, Utton R, Baumgartner KB, Samet JM, Coultas DB. Idiopathic pulmonary fibrosis: survival in population based and hospital based cohorts. Thorax. 1998. 53:469–476.
32. Hubbard R, Johnston I, Britton J. Survival in patients with cryptogenic fibrosing alveolitis: a population-based cohort study. Chest. 1998. 113:396–400.
33. Hubbard R, Johnston I, Coultas DB, Britton J. Mortality rates from cryptogenic fibrosing alveolitis in seven countries. Thorax. 1996. 51:711–716.
34. King TE Jr, Tooze JA, Schwarz MI, Brown KR, Cherniack RM. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med. 2001. 164:1171–1181.
35. Schwartz DA, Merchant RK, Helmers RA, Gilbert SR, Dayton CS, Hunninghake GW. The influence of cigarette smoking on lung function in patients with idiopathic pulmonary fibrosis. Am Rev Respir Dis. 1991. 144:504–506.
36. Panos RJ, Mortenson RL, Niccoli SA, King TE Jr. Clinical deterioration in patients with idiopathic pulmonary fibrosis: causes and assessment. Am J Med. 1990. 88:396–404.
37. Katzenstein AL, Fiorelli RF. Nonspecific interstitial pneumonia/fibrosis. Histologic features and clinical significance. Am J Surg Pathol. 1994. 18:136–147.
38. Nicholson AG, Colby TV, du Bois RM, Hansell DM, Wells AU. The prognostic significance of the histologic pattern of interstitial pneumonia in patients presenting with the clinical entity of cryptogenic fibrosing alveolitis. Am J Respir Crit Care Med. 2000. 162:2213–2217.
39. Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000. 24:19–33.
40. Bellomo R, Finlay M, McLaughlin P, Tai E. Clinical spectrum of cryptogenic organising pneumonitis. Thorax. 1991. 46:554–558.
41. Yousem SA, Colby TV, Gaensler EA. Respiratory bronchiolitis-associated interstitial lung disease and its relationship to desquamative interstitial pneumonia. Mayo Clin Proc. 1989. 64:1373–1380.
42. Johkoh T, Muller NL, Pickford HA, Hartman TE, Ichikado K, Akira M, et al. Lymphocytic interstitial pneumonia: thin-section CT findings in 22 patients. Radiology. 1999. 212:567–572.
43. Vourlekis JS, Brown KK, Cool CD, Young DA, Cherniack RM, King TE, et al. Acute interstitial pneumonitis. Case series and review of the literature. Medicine (Baltimore). 2000. 79:369–378.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download