Abstract
A 63-year old woman was admitted to our hospital for an evaluation of thrombocytopenia. She had been diagnosed with tuberculous pericarditis three months earlier in a local clinic and treated with anti-tuberculosis medication. Two months later, thrombocytopenia developed. The medication was subsequently stopped because it was suspected that the anti-tuberculosis medication, particularly rifampin, might have caused the severe platelet reduction. However, the thrombocytopenia was more aggravated. A bone marrow biopsy was performed, which showed moderate amounts of histiocytes with active hemophagocytosis. This finding strongly suggested that the critical thrombocytopenia had been caused by hemophagocytic syndrome, not by the side effects of the anti-tuberculosis medication. Furthermore, the development of hemophagocytosis might have been due to an uncontrolled tuberculosis infection and its associated aberrant immunity. Therefore, she was started with both standard anti-tuberculosis medication and chemotherapy using etoposide plus steroid. One month after the initiation of treatment, the thrombocytopenia had gradually improved and she was discharged in a tolerable condition. At the third month of the follow-up, her platelet level and ferritin, the activity marker of hemophagocytic syndrome, was within the normal range.
Figures and Tables
Figure 2
Echocardiogram shows focal calcification of the pericardium, which was possibly caused by tuberculous pericarditis.
Figure 3
Bone marrow aspirate reveals histiocytes showing active hemophagocytosis (H&E stain, ×1,000).

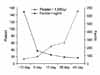
Figure 4
Platelet count was minimally improved, even though antituberculous medication and high dose steroid (1 mg/kg) were started at the time when the patient was diagnosed with tuberculosis-associated hemophagocytic syndrome (4th hospital day). After substituting steroid to chemotherapy which consisted of etoposide and steroid on the 14th hospital day, platelet count was increased and serum ferritin level was decreased within the normal range.
References
1. Scott R, Robb-Smith AH. Histiocytic medullary reticulosis. Lancet. 1939. 2:194–198.
2. Mills MJ. Post-viral haemophagocytic syndrome. J R Soc Med. 1982. 75:555–557.
3. Risdall RJ, Brunning RD, Hernandez JI, Gordon DH. Bacteria-associated hemophagocytic syndrome. Cancer. 1984. 54:2968–2972.
4. Campo E, Condom E, Miro MJ, Cid MC, Romagosa V. Tuberculosis-associated hemophagocytic syndrome: a systemic process. Cancer. 1986. 58:2640–2645.
5. Brastianos PK, Swanson JW, Torbenson M, Sperati J, Karakousis PC. Tuberculosis-associated haemophagocytic syndrome. Lancet Infect Dis. 2006. 6:447–454.
6. Yang CW, Lee JH, Kim YG, Kim YO, Lee SH, Kim BK, et al. Tuberculosis-associated hemophagocytic syndrome in a hemodialysis patient: case report and review of the literature. Nephron. 1996. 72:690–692.
7. Park SS, Kang JH, Kim CH, Chang ED. A case of pancytopenia associated with disseminated tuberculosis and reactive histiocytic hemophagocytic syndrome. Korean J Hematol. 1996. 31:167–173.
8. Yu SE, Kim HW, Shin YS, Kim HS, Lee JM, Kim HJ, et al. A case of tuberculosis-associated hemophagocytic syndrome in renal transplant recipient. Korean J Nephrol. 2002. 21:1037–1042.
9. Shin BC, Kim SW, Ha SW, Sohn JW, Lee JM, Kim NS. Hemophagocytic syndrome associated with bilateral adrenal gland tuberculosis. Korean J Intern Med. 2004. 19:70–73.
10. Larroche C, Mouthon L. Pathogenesis of hemophagocytic syndrome (HPS). Autoimmun Rev. 2004. 3:69–75.
11. Rouphael NG, Talati NJ, Vaughan C, Cunningham K, Moreira R, Gould C. Infections associated with haemophagocytic syndrome. Lancet Infect Dis. 2007. 7:814–822.
12. Jain D, Dash S. Pancytopenia due to extensive hemophagocytosis following anti-tubercular treatment. Am J Hematol. 2004. 75:118–119.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download