Abstract
Pulmonary mucormycosis is an uncommon, serious opportunistic infection caused by fungi belonging to the order Mucorales and it occurs exclusively in debilitated or immuno-compromised hosts. It is known that the fungi can invade the blood vessels and cause serious ischemic necrosis and bleeding5. We experienced a fatal case of pulmonary mucormycosis in a diabetic 75-year-old man who developed a progressive necrotizing lesion despite administering proper and prompt medical and surgical treatment. We report here on this case along with a review of the relevant medical literature.
Figures and Tables
 | Figure 1Initial chest PA (A) and chest CT (B, C) showed two ground glass opacities with hyperlucent area in left upper lobe and another small ground glass opacity with suspicious air-crescent sign in right upper lobe. |
 | Figure 2Bronchoscopic exam showed purulent secretion from upper division of left upper lobe. Bronchial washing and transbronchial lung biopsy was done in upper division of left upper lobe bronchus. |
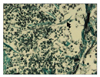 | Figure 3Microscopic finding shows non-septate broad hyphae of mucorales with infiltration of inflammatory cells in pulmonary parenchyme (Gomori-methanamine silver stain, ×400). |
 | Figure 4Serial Chest X-rays showed rapid progressive lesion in both lung field. Compared with chest X-ray at admission (A), follow up X-ray at 15th day showed to progress on both lung fields (B). Large cavitary lesion was seen in right upper lung field. It was only small ground glass opacity at admission. At 35th day, newly developed opacity in right upper lobe and near total haziness in left lung field was noted (C). |
References
1. Sugar AM. Mucormycosis. Clin Infect Dis. 1992. 14:S126–S129.
2. Rinaldi MG. Zygomycosis. Infect Dis Clin North Am. 1989. 3:19–41.
3. Virally ML, Riveline JP, Virally J, Chevojon P, Regnard JF, Belmekki A, et al. Pulmonay mucormycosis in a diabetic patient with HIV. Diabetes Care. 2002. 25:2105.
4. Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999. 341:1906–1912.
5. Davies SF, Knox KS, Sarosi GA. Mason RJ, Broaddus VC, Murray JF, Nadel JA, editors. Chapter 34. Fungal infection. Murray and Nadel's textbook of respiratory medicine. 2005. 4th ed. Philadelphia: Sanders Elsevier Inc;1073–1074. .
6. Murray HW. Pulmonary mucormycosis with massive fatal hemoptysis. Chest. 1975. 68:65–68.
7. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000. 13:236–301.
8. Chang MS, Woo JH. Opportunistic fungal infection. Hanyang Med Rev. 2006. 26:20–33.
9. McAdams HP, Rosado de Christenson M, Strollo DC, Patz EF Jr. Pulmonary mucormycosis: radiologic findings in 32 cases. AJR Am J Roentgenol. 1997. 168:1541–1548.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download